Abstract
Thanks to the pioneering work done by Professor Hamao Umezawa, bioactive compounds have been used in treatment of several diseases including cancer. In this review, we discuss our work, which focuses on developing new candidates for anti-tumor drugs by screening for bioactive natural compounds in microbial cultures using unique experimental systems. We summarize our recent progress including the following: (1) small-molecule modulators of tumor–stromal cell interactions, (2) inhibitors of three-dimensional spheroid formation of cancer cells, (3) multi-cancer cell panel screening and (4) new experimental animal models for cancer metastasis.
Similar content being viewed by others
Introduction
Professor Hamao Umezawa is known for his innovations in the field of antibiotics as well as anti-tumor drugs from microbial cultures.1 He was a pioneer who first used microbial cultures for the development of anti-tumor drugs. This work led to the discovery of several drugs that are currently used in the clinic, such as bleomycin, peplomycin, aclarubicin, bestatin and pirarubicin. At present, we at the Laboratory of Oncology and the Numazu Branch are mainly focused on cancer in the BIKAKEN institute. In this review, we describe our recent progress concerning cancer research.
Small-molecule modulators of tumor–stromal cell interactions
Tumor tissues contain cancer cells and stroma, which consists of the extracellular matrix and various types of cells such as macrophages, endothelial cells, immune cells and fibroblast-like cells (stromal cells). The stromal cells are also referred to as cancer-associated fibroblasts and regulate cancer growth and metastasis through secreted factors and cellular adhesion (tumor–stromal cell interactions). Consequently, the interactions between the tumor cells and stromal cells are attractive targets for cancer therapy. It is possible that the modulation of tumor–stromal cell interactions could suppress cancer growth and metastasis and thus we have been searching for natural compounds that target these interactions.2
In order to screen for active small molecules, we established a co-culture system, in which cancer cells are co-cultured with stromal cells (Figure 1). Using this system, we have identified compounds that inhibit the growth of cancer cells in co-culture but do not affect growth of either type of cell alone (Figure 1). Our efforts yielded several natural compounds from the cultured broth of microorganisms such as actinomycetes and fungi (Figure 1).
Modulators of tumor–stromal cell interactions. For co-culture experiments, cultures were initiated with stromal cells after which cancer cells were directly inoculated onto the layer of stromal cells. Active compounds showed selective growth inhibitory activity against cancer cells co-cultured with stromal cells, but not against cancer cells or stromal cells cultured alone. NBRI23477s, NBRI16716s and intervenolin are novel compounds discovered in our laboratory. This figure is modified from Kawada.2 A full colour version of this figure is available at the Journal of Antibiotics journal online.
Phthoxazolins3 and leucinostatins4 were originally discovered from metabolites produced by streptomycetes and fungi as an inhibitor of cellulose synthesis and an antifungal compound, respectively (Figure 1). We discovered that these compounds could also serve as modulators of tumor-stromal cell interactions of human prostate cancer (PC). In our previously described co-culture system, the addition of the compounds resulted in a higher rate of inhibition for co-cultured PC cells than those cultured alone.5, 6 The mechanism of inhibition is believed to rely on the downregulation of secreted factors. Phthoxazolin A and leucinostatin A were found to inhibit the secretion of insulin-like growth factor-I, a growth factor for PC cells, from the prostate stromal cells. In addition, leucinostatins were found to show antitumor activity in vivo when PC cells were co-injected with stromal cells in nude mice.4
NBRI23477s, new atpenin derivatives, and NBRI16716s are novel compounds derived from fungal strains Penicillium atramentosum PF1420 and Perisporiopsis melioloides Mer-f16716, respectively (Figure 1). They showed growth inhibitory activity against PC cells in co-culture.7, 8 A hydroxyl moiety linked to nitrogen at R2 position was found to be critical for the activity of NBRI16716s. NBRI16716 C, which lacked this moiety, was ineffective against the co-cultured PC cells, whereas the NBRI16716s containing it exhibited growth inhibiting activity. NBRI16716s did not have any adverse effects in mice even when administered at 50 mg kg−1. Furthermore, NBRI16716s showed significant antitumor activity in a PC co-culture xenograft mouse model. Unlike the above-mentioned compounds, phthoxazolins and leucinostatins, our preliminary experiments suggested that NBRI16716s did not affect insulin-like growth factor-I secretion from stromal cells, but rather possibly stimulated the stromal cells to secrete growth inhibitory factors against cancer cells.
Intervenolin is a novel quinoline that we recently discovered from the cultured broth of Nocardia sp. ML96-86F2 using a co-culture system of human gastric cancer and gastric stromal cells (Figure 1).9 While the production levels of intervenolin alone were very low (about 4 mg per 10 l culture), we were able to achieve better results using a total synthesis method. This also allowed us to obtain the original compound as well as its derivatives.10 Intervenolin was found to be non-toxic, as it showed no adverse effects in mice up to 50 mg kg−1. Furthermore, intervenolin was found to exert potent antitumor activity against mouse xenograft models of human gastric and colorectal cancers. Our preliminary results suggested that intervenolin might stimulate stromal cells to secrete growth inhibitory factors against cancer cells. Interestingly, intervenolin has also been shown to have a strong and selective anti-Helicobacter pylori activity without any effect on intestinal bacteria. This provides a clinical advantage as many antibiotics currently used have severe anti-microbial activity against native intestinal bacteria. Moreover, H. pylori infection is one of the causes of gastric cancer. Thus, intervenolin is an attractive drug candidate, because it exhibits both anti-tumor and anti-H. pylori activities. Moreover, one particular intervenolin derivative showed efficient anti-H. pylori activity against mice infected with the bacteria when compared to the standard therapy (paper submitted). We are currently pursuing the development of intervenolin derivatives for use as anti-tumor and anti-H. pylori drugs.
Inhibitors of 3D spheroid formation of cancer cells
EGFRvIII is a mutant form of the epidermal growth factor receptor gene (EGFR) that lacks exons 2–7.11 The resulting protein does not bind to ligands and is constitutively activated.12 The EGFRvIII gene has been found in various cancers such as glioblastoma and lung cancer.13, 14 There is extensive evidence indicating that EGFRvIII is a cancer-specific protein14 and aberrant EGFRvIII signaling has been shown to be important in cancer progression.
Cancer cells can survive and grow in the absence of adhesion or anchorage to a substratum. This ‘anchorage independence’ is one of the most important oncogenic properties of cancer cells and cancer stem cells.15, 16, 17, 18 EGFRvIII cDNA-transfected NIH3T3 cells (NIH3T3/EGFRvIII) formed three-dimensional (3D) spheroids on ultra-low attachment surface plates, whereas the control NIH3T3 cells did not (Figure 2a). NIH3T3/EGFR wild-type cells also formed spheroids when they were cultured with EGF (Figure 2a), but not in the absence of EGF (Figure 2a). Thus, EGFRvIII confers anchorage independence in normal cells. To identify inhibitors of 3D spheroid formation of cancer cells, we developed a screening system for compounds that suppress the cell survival of NIH3T3/EGFRvIII spheroids under 3D-culture conditions, but retain normal NIH3T3 cell growth under two-dimensional (2D) culture conditions (Figure 2b). Using this technique, we identified 3-(2-amino-5-bromophenyl)-2(1H)-quinoxalinone as an active compound among a chemical library containing 30 000 low-molecular-weight compounds (Figure 2c). We named this compound ertredin, derived from ‘EGF receptor three dimensional inhibitor’.19 Ertredin significantly inhibited 3D spheroid growth of NIH3T3/EGFRvIII cells and NIH3T3/EGFR wild-type cells with EGF, but it did not inhibit 2D growth of NIH3T3, NIH3T3/EGFRvIII or NIH3T3/EGFR wild-type cells (Figure 2d). Ertredin treatment by intraperitoneal injection at 30 mg kg−1 per day produced a downregulation of tumorigenicity of NIH3T3/EGFRvIII cells equal to that of a positive control, gefitinib, which was administered orally at 100 or 200 mg kg−1 per day, while also having no detectable adverse effects on the mice. Although ertredin did not directly inhibit recombinant EGFR kinase in vitro, it reduced the amount of EGFRvIII in NIH3T3/EGFRvIII cells. Our preliminary experiments suggest that ertredin upregulates the ubiquitination of EGFRvIII.19
Inhibitors of 3D-spheroid formation of cancer cells. (a) Overexpression of EGFRvIII or EGFRwt induced anchorage-independent growth of NIH3T3 cells. Details in figures are described previously in Atsumi et al.19 (b) Outline of the screening system developed to identify inhibitors of anchorage-independent growth induced by EGFRvIII. (c) Structure of Ertredin. (d) Ertredin inhibited anchorage-independent growth of NIH3T3/EGFRvIII cells. Inhibitory activity of Ertredin against 3D growth of NIH3T3/EGFRvIII (red solid line) or NIH3T3/EGFR wild type (EGFRwt) (blue solid line). Cells were seeded and cultured on ultra-low attachment surface plates (3D) or normal tissue culture plates (2D). Extent of inhibition was detected on day 3. EGF (100 ng ml−1) was added to NIH/3T3/EGFRwt culture. A full colour version of this figure is available at the Journal of Antibiotics journal online.
As mitochondrial metabolite inhibitors such as piericidin also suppressed 3D spheroid formation, we examined the effect of ertredin on oxidative phosphorylation. As a result, we found that ertredin inhibited mitochondrial ATP synthesis in both 3D- and 2D-cultured NIH3T3/EGFRvIII cells. Rotenone, an inhibitor of respiratory chain complex I, also inhibited ATP synthesis and cell growth under 3D conditions but not under 2D conditions. Interestingly, ertredin and rotenone decreased many glycolytic-pathway enzymes under 3D conditions, but not under 2D conditions.19 Thus, due to the downregulation of the glycolytic pathway under 3D conditions, the cells became more sensitive to mitochondrial inhibition by ertredin and rotenone. As the action of ertredin is similar to that of rotenone, we are now studying the target molecules and the effect of ertredin and its derivatives on human tumors.
Multi-cancer cell panel screening and new trehalose analogues
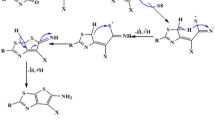
Soil microbes were screened against 40 human cancer cell lines for anti-tumor activity. An extract sample from the culture of an actinomycete strain Lentzea sp. ML457-mF8 showed a cytotoxic effect on the cells.20 The cytotoxic agents of the extract were identified to be pyrazomycins and staurosporine, which due to their combination, presented a unique cytotoxicity pattern. Although pyrazomycins were first reported around 1970,21 they are rare compounds that we have only encountered a few times in our institutional screening history. The isolated pyrazofurin (β-D-form pyrazomycin) showed a cell-line specific cytotoxicity to an amelanotic melanoma cell line LOX-IMVI with an IC50 value <1/10 that of the second most sensitive cell line. During the isolation of pyrazofurin by ODS-HPLC, we found an unidentified compound of molecular weight 444 in the pyrazomycin-containing fraction. The compound was isolated and determined to be a new trehalose derivative due to its structure. We named it lentztrehalose. Changing the culture medium component from barley to rice, two analogue compounds were subsequently isolated. Lentztrehalose was renamed lentztrehalose A and the new analogues were named lentztrehaloses B and C.22 These analogues would be created by transference of dimethylallyl to C-4 of trehalose (lentztrehalose B) and then dihydroxylated (A) and cyclized (C) (Figure 3a). According to the Dictionary of Natural Products (CRC Press), <50 trehalose-containing small compounds have been reported. The 2,3-dihydroxy-3-methylbutoxy moiety of lentztrehalose A is rare and present on only 65 compounds in the database. No cytotoxicity was observed with lentztrehaloses at concentrations up to 200 μg ml−1 in 52 human cancer cell lines.20
Enzyme stable trehalose analogues lentztrehaloses. (a) Structures of trehalose and lentztrehaloses. (b) Enzyme stability of lentztrehaloses.22 Trehalose (TRH) and lentztrehaloses A, B and C (LTA, B and C) were reacted with porcine kidney trehalase and the concentrations of released glucose were determined by a hexokinase assay. Mean±s.e. from triplicate determinations. It is noteworthy that the graphs of lentztrehaloses are overlapped at the bottom.
As lentztrehalose A is an analogue of trehalose, we hypothesized that it was an inhibitor of trehalose-hydrolyzing enzyme trehalase. We tested the inhibitory activity of all three lentztrehalose analogues against porcine kidney trehalase. Lentztrehaloses A and C at concentrations up to 10 mM did not show any inhibitory effect and lentztrehalose B showed only weak inhibition at 10 mM.20, 22 Because the lentztrehaloses were produced under rather dry conditions and lentztrehalose B showed an anti-oxidative effect,22 we next tested whether lentztrehaloses were enzyme-stable analogues of trehalose, meaning they would function as a preferable osmolyte or protector in the producing actinomycete. Lentztrehaloses A, B and C were minimally hydrolyzed by the trehalase (Figure 3b)20, 22 and were not thoroughly digested by any of 12 diverse species of microbes and two human culture cell lines.23
Trehalose is a non-reducing disaccharide formed by an α,α-1,1-glucoside bond between two molecules of α-glucose. Trehalose is currently used as an additive in many foods, dosage forms, cosmetics, preserving solutions and so on because of its moderate sweetness, high water retention capability and ability to protect starch, proteins and lipids from deterioration.24 Trehalose is also expected as an active ingredient of medicine as an autophagy inducer and molecular chaperone.25 Trehalose, however, is readily hydrolyzed by trehalase ubiquitously expressed in species ranging from microbes to humans. Although trehalose is chemically very stable, its biological fragility would limit its further application. Lentztrehaloses, enzyme-stable analogues of trehalose, are promising substitutes for trehalose, as a non-perishable material and a long-acting medicine.
Although some properties such as sweetness and autophagy inducing activity are comparable to trehalose,22 lentztrehaloses show better biological activity than trehalose in several aspects. The improved stability of lentztrehaloses is believed to contribute to the increase in antitumor and bone reinforcement activities. The stability may also play a role in lentztrehaloses’ in vivo suppression of obesity activities. Mice administered lentztrehalose A were less obese compared with those treated with trehalose, even though the dose of lentztrehalose A was 1/4–1/2 lower than that of trehalose.20 Lentztrehaloses also showed better bioavailability than trehalose. Although trehalose was not clearly detected in the peripheral circulation, lentztrehaloses A, B and C were detected up to about 10 μg ml−1 in the short time after and more than 1 μg ml−1 for about 8 h after oral administration at 500 mg kg−1.23 Moreover, blood glucose levels temporarily increased in the trehalose-administrated mice while there was no detectable change in the levels of mice treated with lentztrehaloses.23
One limitation to the clinical use of lentztrehaloses is the production yield; currently, the max yield is 5 g of lentztrehalose from 1 kg grain. We are presently investigating methods for mass production of lentztrehaloses or enzyme-stable trehalose analogues by improving fermentation, breeding of the producing strain and chemical synthesis.26
New experimental animal models for cancer metastasis
Metastasis is the spread of cancer cells from the primary tumor site to distant areas of the body. Metastatic cancer is largely incurable due to its systemic distribution and higher rates of drug resistance, and metastasis is responsible for the vast majority of cancer fatalities. In the case of small cell lung cancer (SCLC), early and widespread metastasis is characteristic of the disease and new therapies to treat the metastases are needed.27 However, the molecular mechanism of SCLC metastasis remains largely unknown. Orthotopic tumor animal models are important tools in the study of metastasis because of the crucial role the tumor microenvironment has in metastasis formation and tumor progression. We have developed a novel orthotopic model for the study of SCLC metastasis.28
In our model, human SCLC cell line DMS273 cells were transfected to express green fluorescent protein (GFP) (DMS273-GFP), resuspended in matrigel, and injected orthotopically into the left lung of Balb/c nude mice. Tumor formation at the orthotopic site and metastatic foci in distant organs were monitored using fluorescence imaging and histological analyses (Figure 4a). Primary tumors were seen in 90% of mice and 40% of mice had metastatic foci 3–4 weeks after tumor cell injection. Metastases were found in the bone, adrenal gland, and brain, which reflects the metastatic pattern in human SCLC. Immunohistological analysis confirmed that the cancer cells in the orthotopic site and distant metastatic sites were GFP positive (Figure 4a), and that the tumor cells in the orthotopic site expressed neuroendocrine marker secretogranin II, which is known to be expressed in a subset of SCLC tumors.
New metastatic model of human SCLC by orthotopic grafting in nude mice. (a) Orthotopic and metastatic tumor formation of G3H, a GFP-labeled subline of human small-cell lung carcinoma cell line DMS273, in nude mice. Representative GFP fluorescent images (upper) and immunostaining with anti-GFP antibody of orthotopic, bone metastatic, and brain metastatic tumor formation. (b) Effect of cisplatin treatment on metastatic tumor formation in our model using G3H cells. The dotted lines show the means of the number of metastasis-positive organs of each group. Percentages show distant metastases incidence. *P<0.05, Fisher’s exact test. (c) Effect of PHA665752 (PHA) treatment on metastatic tumor formation in our model using G3H cells. The dotted lines show the means of the number of metastasis-positive tissues of each group. Percentages show distant metastases incidence. *P<0.05, Fisher’s exact test. This figure is modified from Sakamoto et al.28 A full colour version of this figure is available at the Journal of Antibiotics journal online.
Furthermore, we successfully established a more aggressive cellular subline (G3H) with identical metastatic tropism by recovering and subcloning DMS273-GFP cancer cells from one mouse’s bone metastases. The G3H subline showed similar rates of in vitro cell growth and orthotopic tumor formation but showed enhanced metastatic activity (over 60% of mice had distant metastases) compared with the parental line.
Using G3H cells, we examined the anti-tumor effect of cisplatin, which is used as first-line treatment for SCLC, on the mouse model. G3H cells were administered orthotopically to the lung of nude mice. The mice were then treated with 5 mg kg−1 cisplatin. Compared with the vehicle-treated group, the cisplatin-treated mice had a 45% reduction in orthotopic tumor formation and complete reduction in distant metastatic formation (P<0.05, Figure 4b). These results suggest that our orthotopic model is a useful system for the validation of anti-metastatic activity of anti-cancer compounds.
Because tumor cells often secrete cytokines that affect tumor growth and metastasis, we next investigated cytokine expression levels in the SCLC cells. The G3H subline was shown by enzyme-linked immunosorbent assay to a produce three- to four-fold larger amount of hepatocyte growth factor (HGF) than the parental line. MET protein, a natural receptor for HGF, was detected in both G3H and the parental line by immunoblot analysis. Because the HGF/MET signaling pathway is involved in cellular motility and invasion in various cancers including SCLC,29 we further analyzed the function of HGF/MET signal pathway in our orthotopic model using a specific MET inhibitor PHA665752.30 Three days of treatment in a week with PHA665752 at a dose of 15 mg kg−1 did not affect primary tumor formation but significantly inhibited metastasis formation compared with vehicle control (distant metastases incidence, P<0.05, Figure 4c). Our data suggest that HGF/MET signal plays an important role in tumor metastasis in our model.
In summary, we developed a novel orthotopic metastatic SCLC mouse model that greatly reflects clinical disease in metastasis tropism and HGF autocrine. There are only a few reports of metastatic orthotopic SCLC models and, to the best of our knowledge, our model is the first one that has potential to form spontaneous metastases in brain.
Perspective
We hope our findings can be helpful for the innovation of new clinical drugs. We continue to search for compounds that are beneficial to human health and life.
Dedication
This article is dedicated to Prof. Hamao Umezawa on the occasion of the 60th anniversary of worldwide marketing of kanamycin.
References
Umezawa, H. Secondary microbial metabolites with potentials for antineoplastic actions: anitneoplasitc antibiotics and immunopotentiatiors. Gan. To. Kagaku. Ryoho. 104, 1071–1086 (1983).
Kawada, M. Small molecules modulating tumor-stromal cell interactions: new candidates for anti-tumor drugs. J. Antibiot. 69, 411–414 (2016).
Omura, S., Tanaka, Y., Kanaya, I., Shinose, M. & Takahashi, Y. Phthoxazolin, a specific inhibitor of cellulose biosynthesis, produced by a strain of Streptomyces sp. J. Antibiot. 43, 1034–1036 (1990).
Arai, T., Mikami, Y., Fukushima, K., Utsumi, T. & Yazawa, K. A new antibiotic, leucinostatin, derived from Penicillium lilacinum. J. Antibiot. 26, 157–161 (1973).
Kawada, M., Inoue, H., Usami, I. & Ikeda, D. Phthoxazolin A inhibits prostate cancer growth by modulating tumor-stromal cell interactions. Cancer Sci. 100, 150–157 (2009).
Kawada, M. et al. Leucinostatin A inhibits prostate cancer growth through reduction of insulin-like growth factor-I expression in prostate stromal cells. Int. J. Cancer 126, 810–818 (2010).
Kawada, M., Momose, I., Someno, T., Tsujiuchi, G. & Ikeda, D. New atpenins, NBRI23477 A and B, inhibit the growth of human prostate cancer cells. J. Antibiot. 62, 243–246 (2009).
Kawada, M. et al. NBRI16716A, a new antitumor compound against human prostate cancer cells, produced by Perisporiopsis melioloides Mer-f16716. J. Antibiot. 63, 319–323 (2010).
Kawada, M. et al. Intervenolin, a new antitumor compound with anti-Helicobacter pylori activity, from Nocardia sp ML96-86F2. J. Antibiot. 66, 543–548 (2013).
Abe, H. et al. Synthesis of intervenolin, an antitumor natural quino lone with unusual substituents. Org. Lett. 15, 2124–2127 (2013).
Yamazaki, H. et al. Amplification of the structurally and functionally altered epidermal growth factor receptor gene (c-erbB) in human brain tumors. Mol. Cell Biol. 8, 1816–1820 (1988).
Yamazaki, H., Ohba, Y., Tamaoki, N. & Shibuya, M. A deletion mutation within the ligand-binding domain is responsible for activation of epidermal growth-factor receptor gene in human brain-tumors. Jpn J. Cancer Res. 81, 773–779 (1990).
Pedersen, M. W., Meltorn, M., Damstrup, L. & Poulsen, H. The type III epidermal growth factor receptor mutation. In: biological significance and potential target for anti-cancer therapy. Ann. Oncol. 12, 745–760 (2001).
Gan, H. K., Cvrljevic, A. N. & Johns, T. G. The epidermal growth factor receptor variant III (EGFRvIII): where wild things are altered. FEBS J. 280, 5350–5370 (2013).
Sakamoto, S. & Kyprianou, N. Targeting anoikis resistance in prostate cancer metastasis. Mol. Aspects Med. 31, 205–214 (2010).
Paoli, P., Giannoni, E. & Chiarugi, P. Anoikis molecular pathways and its role in cancer progression. Biochim. Biophys. Acta 1833, 3481–3498 (2013).
Guadamilas, M. C., Cerezo, A. & Pozo, M. A. D. Overcoming anoikis—pathways to anchorage-independent growth in cancer. J. Cell Sci. 24, 3189–3197 (2011).
Foley, J. M. et al. Anoikis-resistant subpopulations of human osteosarcoma display significant chemoresistance and are sensitive to targeted epigenetic therapies predicted by expression profiling. J. Transl. Med. 13, 110 (2015).
Atsumi, S. et al. New anti-cancer chemicals Ertredin and its derivatives, regulate oxidative phosphorylation and glycolysis and suppress sphere formation in vitro and tumor growth in EGFRvIII-transformed cells. BMC Cancer 16, 496 (2016).
Wada, S., Ohba, S., Someno, T., Hatano, M. & Nomoto, A. Structure and biological properties of lentztrehalose: a novel trehalose analog. J. Antibiot. 67, 319–322 (2014).
Plagemann, P. G. & Behrens, M. Inhibition of de novo pyrimidine nucleotide and DNA synthesis and growth of cultured Novikoff rat hepatoma cells and other cell lines by pyrazofurin (NSC 143095). Cancer Res. 36, 3807–3812 (1976).
Wada, S. et al. Novel autophagy inducers lentztrehaloses A, B and C. J. Antibiot. 68, 521–529 (2015).
Wada, S. et al. Stability and bioavailability of lentztrehaloses A, B, and C as replacements for trehalose. J. Agric. Food Chem. 64, 7121–7126 (2016).
Ohtake, S. & Wand, Y. J. Trehalose: current use and future applications. J. Pharm. Sci. 100, 2020–2053 (2011).
Emanuele, E. Can trehalose prevent neurodegeneration? Insights from experimental studies. Curr. Drug Targets 15, 551–557 (2014).
Zhang, M., Wada, S., Amemiya, F., Watanabe, T. & Shibasaki, M. Synthesis and determination of absolute configuration of lentztrehalose A. Chem. Pharm. Bull. 63, 961–966 (2015).
William, W. N. J. & Glisson, B. S. Novel strategies for the treatment of small-cell lung carcinoma. Nat. Rev. Clin. Oncol. 8, 611–619 (2011).
Sakamoto, S. et al. New metastatic model of human small-cell lung cancer by orthotopic transplantation in mice. Cancer Sci. 106, 367–374 (2015).
Maulik, G. et al. Modulation of the c-MET/hepatocyte growth factor pathway in small cell lung cancer. Clin. Cancer Res. 8, 620–627 (2002).
Smolen, G. A. et al. Amplification of MET may identify a subset of cancers with extreme sensitivity to the selective tyrosine kinase inhibitor PHA665752. Proc. Natl Acad. Sci. USA 103, 2316–2321 (2006).
Acknowledgements
We are deeply appreciative of all our colleagues in BIKAKEN.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kawada, M., Atsumi, S., Wada, Si. et al. Novel approaches for identification of anti-tumor drugs and new bioactive compounds. J Antibiot 71, 39–44 (2018). https://doi.org/10.1038/ja.2017.97
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2017.97
This article is cited by
-
Phenotypic screening system using three-dimensional (3D) culture models for natural product screening
The Journal of Antibiotics (2021)