Abstract
Objective:
To determine if implementation of a protocol based on a neonatal early-onset sepsis (EOS) calculator developed by Kaiser Permanente would safely reduce antibiotic use in well-appearing term infants born to mothers with chorioamnionitis in the unique setting of an Observation Nursery.
Study design:
Data obtained from a retrospective chart review of well-appearing term infants born between 2009 and 2016 were entered into the EOS calculator to obtain management recommendations.
Results:
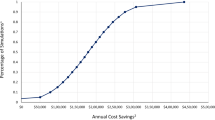
Three hundred and sixty-two infants met the study criteria. Management according to the EOS calculator would reduce antibiotic use from 99% to 2.5% (P<0.0001) of patients. Average length of therapy would also decrease from 2.08 to 0.05 days (P<0.0001). One infant, who remained asymptomatic, had Enterococcus bacteremia and received a 7-day course of broad-spectrum antibiotics.
Conclusions:
Culture-positive sepsis in asymptomatic neonates born to mothers with chorioamnionitis is rare. Management according to the EOS calculator would markedly reduce the potential complications of antibiotic use. These data should initiate re-examination of existing protocols for management of this cohort of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Verani JR, McGee L, Schrag SJ, Division of Bacterial Diseases NCfIaRD, Centers for Disease Control and Prevention (CDC). Prevention of perinatal group B streptococcal disease—revised guidelines from CDC, 2010. MMWR Recomm Rep 2010; 59 (RR-10): 1–36.
Polin RA . Newborn CoFa. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics 2012; 129 (5): 1006–1015.
Schulman J, Saiman L . Metrics for NICU antibiotic use: which rate is right? J Perinatol 2011; 31 (8): 511–513.
Schulman J, Dimand RJ, Lee HC, Duenas GV, Bennett MV, Gould JB . Neonatal intensive care unit antibiotic use. Pediatrics 2015; 135 (5): 826–833.
Mukhopadhyay S, Lieberman ES, Puopolo KM, Riley LE, Johnson LC . Effect of early-onset sepsis evaluations on in-hospital breastfeeding practices among asymptomatic term neonates. Hosp Pediatr 2015; 5 (4): 203–210.
Soll RF, Edwards WH . Antibiotic use in neonatal intensive care. Pediatrics 2015; 135 (5): 928–929.
Braun D, Bromberger P, Ho NJ, Getahun D . Low rate of perinatal sepsis in term infants of mothers with chorioamnionitis. Am J Perinatol 2016 33 (2): 143–150.
Mukhopadhyay S, Taylor JA, Von Kohorn I, Flaherman V, Burgos AE, Phillipi CA et al. Variation in sepsis evaluation across a national network of nurseries. Pediatrics 2017; 139 (3): e20162845.
Benitz WE, Wynn JL, Polin RA . Reappraisal of guidelines for management of neonates with suspected early-onset sepsis. J Pediatr 2015; 166 (4): 1070–1074.
Cantey JB, Patel SJ . Antimicrobial stewardship in the NICU. Infect Dis Clin N Am 2014; 28 (2): 247–261.
Taylor JA, Opel DJ . Choriophobia: a 1-act play. Pediatrics 2012; 130 (2): 342–346.
Polin RA, Watterberg K, Benitz W, Eichenwald E . The conundrum of early-onset sepsis. Pediatrics 2014; 133 (6): 1122–1123.
Kiser C, Nawab U, McKenna K, Aghai ZH . Role of guidelines on length of therapy in chorioamnionitis and neonatal sepsis. Pediatrics 2014; 133 (6): 992–998.
Shakib J, Buchi K, Smith E, Young PC . Management of newborns born to mothers with chorioamnionitis: is it time for a kinder, gentler approach? Acad Pediatr 2015; 15 (3): 340–344.
Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K et al. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol 2016; 127 (3): 426–436.
Mukhopadhyay S, Eichenwald EC, Puopolo KM . Neonatal early-onset sepsis evaluations among well-appearing infants: projected impact of changes in CDC GBS guidelines. J Perinatol 2013; 33 (3): 198–205.
Flidel-Rimon O, Galstyan S, Juster-Reicher A, Rozin I, Shinwell ES . Limitations of the risk factor based approach in early neonatal sepsis evaluations. Acta Paediatr 2012; 101 (12): e540–e544.
Buckler B, Bell J, Sams R, Cagle W, Bell SA, Allen C et al. Unnecessary workup of asymptomatic neonates in the era of group B streptococcus prophylaxis. Infect Dis Obstet Gynecol 2010; 2010: 369654.
Berardi A, Fornaciari S, Rossi C, Patianna V, Bacchi Reggiani ML, Ferrari F et al. Safety of physical examination alone for managing well-appearing neonates ≥35 weeks' gestation at risk for early-onset sepsis. J Matern Fetal Neonatal Med 2015; 28 (10): 1123–1127.
Duvoisin G, Fischer C, Maucort-Boulch D, Giannoni E . Reduction in the use of diagnostic tests in infants with risk factors for early-onset neonatal sepsis does not delay antibiotic treatment. Swiss Med Wkly 2014; 144: w13981.
Alm B, Erdes L, Möllborg P, Pettersson R, Norvenius SG, Aberg N et al. Neonatal antibiotic treatment is a risk factor for early wheezing. Pediatrics 2008; 121 (4): 697–702.
Azad MB, Bridgman SL, Becker AB, Kozyrskyj AL . Infant antibiotic exposure and the development of childhood overweight and central adiposity. Int J Obes (Lond) 2014; 38 (10): 1290–1298.
Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA . Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr 2014; 168 (11): 1063–1069.
Murphy R, Stewart AW, Braithwaite I, Beasley R, Hancox RJ, Mitchell EA et al. Antibiotic treatment during infancy and increased body mass index in boys: an international cross-sectional study. Int J Obes (Lond) 2014; 38 (8): 1115–1119.
Kronman MP, Zaoutis TE, Haynes K, Feng R, Coffin SE . Antibiotic exposure and IBD development among children: a population-based cohort study. Pediatrics 2012; 130 (4): e794–e803.
Hviid A, Svanström H, Frisch M . Antibiotic use and inflammatory bowel diseases in childhood. Gut 2011; 60 (1): 49–54.
Rutten NB, Rijkers GT, Meijssen CB, Crijns CE, Oudshoorn JH, van der Ent CK et al. Intestinal microbiota composition after antibiotic treatment in early life: the INCA study. BMC Pediatr 2015; 15: 204.
Alexander VN, Northrup V, Bizzarro MJ . Antibiotic exposure in the newborn intensive care unit and the risk of necrotizing enterocolitis. J Pediatr 2011; 159 (3): 392–397.
Kuppala VS, Meinzen-Derr J, Morrow AL, Schibler KR . Prolonged initial empirical antibiotic treatment is associated with adverse outcomes in premature infants. J Pediatr 2011; 159 (5): 720–725.
Mukhopadhyay S, Dukhovny D, Mao W, Eichenwald EC, Puopolo KM . 2010 perinatal GBS prevention guideline and resource utilization. Pediatrics 2014; 133 (2): 196–203.
Malloy MH . Chorioamnionitis: epidemiology of newborn management and outcome United States 2008. J Perinatol 2014; 34 (8): 611–615.
Patel SJ, Saiman L . Principles and strategies of antimicrobial stewardship in the neonatal intensive care unit. Semin Perinatol 2012; 36 (6): 431–436.
Falciglia G, Hageman JR, Schreiber M, Alexander K . Antibiotic therapy and early onset sepsis. NeoReviews 2012 13 (2): e86–e93.
Kaiser Permanente. Neonatal Early-Onset Sepsis Calculator, 2015. Available at: https://neonatalsepsiscalculator.kaiserpermanente.org/(last accessed 7 February 2017.)
Escobar GJ, Puopolo KM, Wi S, Turk BJ, Kuzniewicz MW, Walsh EM et al. Stratification of risk of early-onset sepsis in newborns ≥34 weeks' gestation. Pediatrics 2014; 133 (1): 30–36.
Puopolo KM, Escobar GJ . Early-onset sepsis: a predictive model based on maternal risk factors. Curr Opin Pediatr 2013; 25 (2): 161–166.
Kuzniewicz MW, Walsh EM, Li S, Fischer A, Escobar GJ . Development and implementation of an early-onset sepsis calculator to guide antibiotic management in late preterm and term neonates. Jt Comm J Qual Patient Saf 2016; 42 (5): 232–239.
Kuzniewicz MW, Puopolo KM, Fischer A, Walsh EM, Li S, Newman TB et al. A quantitative, risk-based approach to the management of neonatal early-onset sepsis. JAMA Pediatr 2017 171 (4): 365–371.
Kerste M, Corver J, Sonnevelt MC, van Brakel M, van der Linden PD, M Braams-Lisman BA et al. Application of sepsis calculator in newborns with suspected infection. J Matern Fetal Neonatal Med 2016; 29 (23): 3860–3865.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG . Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42 (2): 377–381.
Cordero L, Sananes M, Ayers LW . Bloodstream infections in a neonatal intensive-care unit: 12 years' experience with an antibiotic control program. Infect Control Hosp Epidemiol 1999; 20 (4): 242–246.
Kumar A, Kumar P, Basu S . Enterococcus fecalis sepsis and leukemoid reaction: an unusual association at birth. J Pediatr Hematol Oncol 2015; 37 (7): e419–e420.
Resch B, Renoldner B, Hofer N . Comparison between pathogen associated laboratory and clinical parameters in early-onset sepsis of the newborn. Open Microbiol J 2016; 10: 133–139.
Wortham JM, Hansen NI, Schrag SJ, Hale E, Van Meurs K, Sánchez PJ et al. Chorioamnionitis and culture-confirmed, early-onset neonatal infections. Pediatrics 2016; 137 (1): e20152323.
Vouloumanou EK, Plessa E, Karageorgopoulos DE, Mantadakis E, Falagas ME . Serum procalcitonin as a diagnostic marker for neonatal sepsis: a systematic review and meta-analysis. Intens Care Med 2011; 37 (5): 747–762.
Christensen RD, Rothstein G, Hill HR, Hall RT . Fatal early onset group B streptococcal sepsis with normal leukocyte counts. Pediatr Infect Dis 1985; 4 (3): 242–245.
Benitz WE . Adjunct laboratory tests in the diagnosis of early-onset neonatal sepsis. Clin Perinatol 2010; 37 (2): 421–438.
Mithal LB, Palac HL, Yogev R, Ernst LM, Mestan KK . Cord blood acute phase reactants predict early onset neonatal sepsis in preterm infants. PLoS ONE 2017; 12 (1): e0168677.
Arnon S, Litmanovitz I, Regev RH, Bauer S, Shainkin-Kestenbaum R, Dolfin T . Serum amyloid A: an early and accurate marker of neonatal early-onset sepsis. J Perinatol 2007; 27 (5): 297–302.
Gad GI, Ismail RI, El-Masry SA, Gouda HR . Serum apelin in early-onset neonatal sepsis: is it diagnostic? J Neonatal Perinatal Med 2014; 7 (3): 207–212.
Newman TB, Draper D, Puopolo KM, Wi S, Escobar GJ . Combining immature and total neutrophil counts to predict early onset sepsis in term and late preterm newborns: use of the I/T2. Pediatr Infect Dis J 2014; 33 (8): 798–802.
He Y, Du WX, Jiang HY, Ai Q, Feng J, Liu Z et al. Multiplex cytokine profiling identifies interleukin-27 as a novel biomarker for neonatal early onset sepsis. Shock 2017; 47 (2): 140–147.
Al-Zahrani AKh, Ghonaim MM, Hussein YM, Eed EM, Khalifa AS, Dorgham LS . Evaluation of recent methods versus conventional methods for diagnosis of early-onset neonatal sepsis. J Infect Dev Ctries 2015; 9 (4): 388–393.
Franz AR, Bauer K, Schalk A, Garland SM, Bowman ED, Rex K et al. Measurement of interleukin 8 in combination with C-reactive protein reduced unnecessary antibiotic therapy in newborn infants: a multicenter, randomized, controlled trial. Pediatrics 2004; 114 (1): 1–8.
Newman TB, Puopolo KM, Wi S, Draper D, Escobar GJ . Interpreting complete blood counts soon after birth in newborns at risk for sepsis. Pediatrics 2010; 126 (5): 903–909.
Antibiotics for Early-Onset Neonatal Infection. NICE Clinical Guideline. National Institute for Health and Clinical Excellence: Manchester, UK, 2014; 149.
Cotten CM, Smith PB . Duration of empirical antibiotic therapy for infants suspected of early-onset sepsis. Curr Opin Pediatr 2013; 25 (2): 167–171.
Acknowledgements
This research was presented, in part, at Hot Topics in Neonatology conference in Washington DC in 2016, the Eastern Society for Pediatric Research, Philadelphia, PA in 2017 and the Pediatric Academic Society Meeting, San Francisco, CA in 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Money, N., Newman, J., Demissie, S. et al. Anti-microbial stewardship: antibiotic use in well-appearing term neonates born to mothers with chorioamnionitis. J Perinatol 37, 1304–1309 (2017). https://doi.org/10.1038/jp.2017.137
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.137
This article is cited by
-
Chorioamnionitis and neonatal outcomes
Pediatric Research (2022)
-
Early-onset sepsis risk calculator: a review of its effectiveness and comparative study with our evidence-based local guidelines
Italian Journal of Pediatrics (2021)
-
A comparison of Triple I classification with neonatal early-onset sepsis calculator recommendations in neonates born to mothers with clinical chorioamnionitis
Journal of Perinatology (2020)
-
Management of Late Preterm and Term Neonates exposed to maternal Chorioamnionitis
BMC Pediatrics (2019)
-
Induction of labor and early-onset Sepsis guidelines: impact on NICU admissions in Erie County, NY
Maternal Health, Neonatology and Perinatology (2019)