Abstract
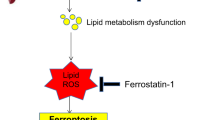
Hepatic ischemia–reperfusion (IR) injury is a common clinical issue lacking effective therapy and validated pharmacological targets. Here, using integrative 'omics' analysis, we identified an arachidonate 12-lipoxygenase (ALOX12)–12-hydroxyeicosatetraenoic acid (12-HETE)–G-protein-coupled receptor 31 (GPR31) signaling axis as a key determinant of the hepatic IR process. We found that ALOX12 was markedly upregulated in hepatocytes during ischemia to promote 12-HETE accumulation and that 12-HETE then directly binds to GPR31, triggering an inflammatory response that exacerbates liver damage. Notably, blocking 12-HETE production inhibits IR-induced liver dysfunction, inflammation and cell death in mice and pigs. Furthermore, we established a nonhuman primate hepatic IR model that closely recapitulates clinical liver dysfunction following liver resection. Most strikingly, blocking 12-HETE accumulation effectively attenuated all pathologies of hepatic IR in this model. Collectively, this study has revealed previously uncharacterized metabolic reprogramming involving an ALOX12–12-HETE–GPR31 axis that functionally determines hepatic IR procession. We have also provided proof of concept that blocking 12-HETE production is a promising strategy for preventing and treating IR-induced liver damage.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Zhai, Y., Petrowsky, H., Hong, J.C., Busuttil, R.W. & Kupiec-Weglinski, J.W. Ischaemia–reperfusion injury in liver transplantation—from bench to bedside. Nat. Rev. Gastroenterol. Hepatol. 10, 79–89 (2013).
Vollmar, B. & Menger, M.D. The hepatic microcirculation: mechanistic contributions and therapeutic targets in liver injury and repair. Physiol. Rev. 89, 1269–1339 (2009).
Uchida, Y. et al. T-cell immunoglobulin mucin-3 determines severity of liver ischemia/reperfusion injury in mice in a TLR4-dependent manner. Gastroenterology 139, 2195–2206 (2010).
Wang, J.H. et al. Autophagy suppresses age-dependent ischemia and reperfusion injury in livers of mice. Gastroenterology 141, 2188–2199 (2011).
Clavien, P.A. et al. A prospective randomized study in 100 consecutive patients undergoing major liver resection with versus without ischemic preconditioning. Ann. Surg. 238, 843–850, discussion 851–852 (2003).
Eltzschig, H.K. & Eckle, T. Ischemia and reperfusion—from mechanism to translation. Nat. Med. 17, 1391–1401 (2011).
Zhai, Y., Busuttil, R.W. & Kupiec-Weglinski, J.W. Liver ischemia and reperfusion injury: new insights into mechanisms of innate-adaptive immune-mediated tissue inflammation. Am. J. Transplant. 11, 1563–1569 (2011).
Peralta, C., Jiménez-Castro, M.B. & Gracia-Sancho, J. Hepatic ischemia and reperfusion injury: effects on the liver sinusoidal milieu. J. Hepatol. 59, 1094–1106 (2013).
Mashima, R. & Okuyama, T. The role of lipoxygenases in pathophysiology; new insights and future perspectives. Redox Biol. 6, 297–310 (2015).
Tourdot, B.E. & Holinstat, M. Targeting 12-lipoxygenase as a potential novel antiplatelet therapy. Trends Pharmacol. Sci. 38, 1006–1015 (2017).
Powell, W.S. & Rokach, J. Biosynthesis, biological effects, and receptors of hydroxyeicosatetraenoic acids (HETEs) and oxoeicosatetraenoic acids (oxo-ETEs) derived from arachidonic acid. Biochim. Biophys. Acta 1851, 340–355 (2015).
Un, K. et al. Efficient suppression of murine intracellular adhesion molecule-1 using ultrasound-responsive and mannose-modified lipoplexes inhibits acute hepatic inflammation. Hepatology 56, 259–269 (2012).
Moles, A. et al. A TLR2/S100A9/CXCL-2 signaling network is necessary for neutrophil recruitment in acute and chronic liver injury in the mouse. J. Hepatol. 60, 782–791 (2014).
Tang, K. et al. Convergence of eicosanoid and integrin biology: 12-lipoxygenase seeks a partner. Mol. Cancer 14, 111 (2015).
Porro, B., Songia, P., Squellerio, I., Tremoli, E. & Cavalca, V. Analysis, physiological and clinical significance of 12-HETE: a neglected platelet-derived 12-lipoxygenase product. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 964, 26–40 (2014).
Johnson, E.N., Brass, L.F. & Funk, C.D. Increased platelet sensitivity to ADP in mice lacking platelet-type 12-lipoxygenase. Proc. Natl. Acad. Sci. USA 95, 3100–3105 (1998).
Luci, D.K. et al. Synthesis and structure–activity relationship studies of 4-((2-hydroxy-3-methoxybenzyl)amino)benzenesulfonamide derivatives as potent and selective inhibitors of 12-lipoxygenase. J. Med. Chem. 57, 495–506 (2014).
Husted, A.S., Trauelsen, M., Rudenko, O., Hjorth, S.A. & Schwartz, T.W. GPCR-mediated signaling of metabolites. Cell Metab. 25, 777–796 (2017).
Milligan, G., Alvarez-Curto, E., Hudson, B.D., Prihandoko, R. & Tobin, A.B. FFA4/GPR120: pharmacology and therapeutic opportunities. Trends Pharmacol. Sci. 38, 809–821 (2017).
Lu, J. et al. Structural basis for the cooperative allosteric activation of the free fatty acid receptor GPR40. Nat. Struct. Mol. Biol. 24, 570–577 (2017).
Im, D.S. FFA4 (GPR120) as a fatty acid sensor involved in appetite control, insulin sensitivity and inflammation regulation. Mol. Aspects Med. S0098-2997(17)30064-X (2017).
Guo, Y. et al. Identification of the orphan G protein–coupled receptor GPR31 as a receptor for 12-(S)-hydroxyeicosatetraenoic acid. J. Biol. Chem. 286, 33832–33840 (2011).
Garcia, V. et al. 20-HETE signals through G-protein-coupled receptor GPR75 (Gq) to affect vascular function and trigger hypertension. Circ. Res. 120, 1776–1788 (2017).
Luci, D. et al. Discovery of ML355, a potent and selective inhibitor of human 12-lipoxygenase. in Probe Reports from the NIH Molecular Libraries Program (National Institutes of Health, 2010).
Gregus, A.M. et al. Systematic analysis of rat 12/15-lipoxygenase enzymes reveals critical role for spinal eLOX3 hepoxilin synthase activity in inflammatory hyperalgesia. FASEB J. 27, 1939–1949 (2013).
Cooper, D.K., Gollackner, B. & Sachs, D.H. Will the pig solve the transplantation backlog? Annu. Rev. Med. 53, 133–147 (2002).
Robertson, F.P., Fuller, B.J. & Davidson, B.R. An evaluation of ischaemic preconditioning as a method of reducing ischaemia reperfusion injury in liver surgery and transplantation. J. Clin. Med. 6, E69 (2017).
Brenner, C., Galluzzi, L., Kepp, O. & Kroemer, G. Decoding cell death signals in liver inflammation. J. Hepatol. 59, 583–594 (2013).
Ju, C., Colgan, S.P. & Eltzschig, H.K. Hypoxia-inducible factors as molecular targets for liver diseases. J. Mol. Med. (Berl.) 94, 613–627 (2016).
van Golen, R.F., van Gulik, T.M. & Heger, M. The sterile immune response during hepatic ischemia/reperfusion. Cytokine Growth Factor Rev. 23, 69–84 (2012).
Datta, G., Fuller, B.J. & Davidson, B.R. Molecular mechanisms of liver ischemia reperfusion injury: insights from transgenic knockout models. World J. Gastroenterol. 19, 1683–1698 (2013).
Selzner, N., Rudiger, H., Graf, R. & Clavien, P.A. Protective strategies against ischemic injury of the liver. Gastroenterology 125, 917–936 (2003).
Corcoran, S.E. & O'Neill, L.A. HIF1α and metabolic reprogramming in inflammation. J. Clin. Invest. 126, 3699–3707 (2016).
Shimano, H. & Sato, R. SREBP-regulated lipid metabolism: convergent physiology— divergent pathophysiology. Nat. Rev. Endocrinol. http://dx.doi.org/10.1038/nrendo.2017.91 (2017).
Chouchani, E.T. et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature 515, 431–435 (2014).
Fehrenbacher, N. et al. The G protein–coupled receptor GPR31 promotes membrane association of KRAS. J. Cell Biol. 216, 2329–2338 (2017).
Honn, K.V. et al. 12-HETER1/GPR31, a high-affinity 12(S)-hydroxyeicosatetraenoic acid receptor, is significantly up-regulated in prostate cancer and plays a critical role in prostate cancer progression. FASEB J. 30, 2360–2369 (2016).
Zhang, Q., Lenardo, M.J. & Baltimore, D. 30 years of NF-κB: a blossoming of relevance to human pathobiology. Cell 168, 37–57 (2017).
King, L.A., Toledo, A.H., Rivera-Chavez, F.A. & Toledo-Pereyra, L.H. Role of p38 and JNK in liver ischemia and reperfusion. J. Hepatobiliary Pancreat. Surg. 16, 763–770 (2009).
Stevens, R.C. et al. The GPCR Network: a large-scale collaboration to determine human GPCR structure and function. Nat. Rev. Drug Discov. 12, 25–34 (2013).
Wacker, D., Stevens, R.C. & Roth, B.L. How ligands illuminate GPCR molecular pharmacology. Cell 170, 414–427 (2017).
Rask-Andersen, M., Almén, M.S. & Schiöth, H.B. Trends in the exploitation of novel drug targets. Nat. Rev. Drug Discov. 10, 579–590 (2011).
Strasser, A., Wittmann, H.J. & Seifert, R. Binding kinetics and pathways of ligands to GPCRs. Trends Pharmacol. Sci. 38, 717–732 (2017).
Xiang, J. et al. Successful strategies to determine high-resolution structures of GPCRs. Trends Pharmacol. Sci. 37, 1055–1069 (2016).
Li, R. et al. SOAP2: an improved ultrafast tool for short read alignment. Bioinformatics 25, 1966–1967 (2009).
Mortazavi, A., Williams, B.A., McCue, K., Schaeffer, L. & Wold, B. Mapping and quantifying mammalian transcriptomes by RNA-Seq. Nat. Methods 5, 621–628 (2008).
Krzywinski, M. et al. Circos: an information aesthetic for comparative genomics. Genome Res. 19, 1639–1645 (2009).
Kim, D., Langmead, B. & Salzberg, S.L. HISAT: a fast spliced aligner with low memory requirements. Nat. Methods 12, 357–360 (2015).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Langfelder, P. & Horvath, S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinformatics 9, 559 (2008).
Wang, X. et al. Dusp14 protects against hepatic ischemia–reperfusion injury via Tak1 suppression. J. Hepatol. S0168-8278(17)32275-4 (2017).
Hu, J. et al. Targeting TRAF3 signaling protects against hepatic ischemia/reperfusions injury. J. Hepatol. 64, 146–159 (2016).
Sun, P. et al. Mindin deficiency protects the liver against ischemia/reperfusion injury. J. Hepatol. 63, 1198–1211 (2015).
Li, L. et al. Attenuation of cerebral ischemic injury in interferon regulatory factor 3 deficient rat. J. Neurochem. http://dx.doi.org/10.1111/jnc.13448 (2015).
Martin-Venegas, R., Jáuregui, O. & Moreno, J.J. Liquid chromatography–tandem mass spectrometry analysis of eicosanoids and related compounds in cell models. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 964, 41–49 (2014).
Masoodi, M., Eiden, M., Koulman, A., Spaner, D. & Volmer, D.A. Comprehensive lipidomics analysis of bioactive lipids in complex regulatory networks. Anal. Chem. 82, 8176–8185 (2010).
Zhu, Q.F. et al. Analysis of cytochrome P450 metabolites of arachidonic acid by stable isotope probe labeling coupled with ultra high–performance liquid chromatography/mass spectrometry. J. Chromatogr. A 1410, 154–163 (2015).
Wang, P.X. et al. Targeting CASP8 and FADD-like apoptosis regulator ameliorates nonalcoholic steatohepatitis in mice and nonhuman primates. Nat. Med. 23, 439–449 (2017).
Zhao, G.N. et al. Tmbim1 is a multivesicular body regulator that protects against non-alcoholic fatty liver disease in mice and monkeys by targeting the lysosomal degradation of Tlr4. Nat. Med. 23, 742–752 (2017).
Shalem, O. et al. Genome-scale CRISPR–Cas9 knockout screening in human cells. Science 343, 84–87 (2014).
Jiang, X. et al. Tumor necrosis factor receptor–associated factor 3 is a positive regulator of pathological cardiac hypertrophy. Hypertension 66, 356–367 (2015).
Ji, Y.X. et al. The ubiquitin E3 ligase TRAF6 exacerbates pathological cardiac hypertrophy via TAK1-dependent signalling. Nat. Commun. 7, 11267 (2016).
Bao, M.W. et al. Cardioprotective role of growth/differentiation factor 1 in post-infarction left ventricular remodelling and dysfunction. J. Pathol. 236, 360–372 (2015).
Guo, S. et al. Oncostatin M confers neuroprotection against ischemic stroke. J. Neurosci. 35, 12047–12062 (2015).
Acknowledgements
We thank Shanghai Metabolome Institute–Wuhan for their help in examining AA metabolites in the liver, serum and cell lysates. This work was supported by grants from the National Science Fund for Distinguished Young Scholars (no. 81425005; H.L.), the Key Project of the National Natural Science Foundation (no. 81330005 and 81630011; H.L.), the National Science and Technology Support Project (no. 2014BAI02B01 and 2015BAI08B01; H.L.), the National Key Research and Development Program (no. 2013YQ030923-05 (H.L.) and 2016YFF0101504 (Z.-G.S.)), the National Natural Science Foundation of China (no. 81770053; Z.-G.S.) and the Key Collaborative Project of the National Natural Science Foundation (no. 91639304; H.L. and Z.-G.S.).
Author information
Authors and Affiliations
Contributions
X.-J.Z., X.C., Z.-Z.Y. and J.F. designed and performed the experiments, analyzed the data and wrote the manuscript; X.W. performed animal experiments, analyzed data and edited the manuscript; W.W. and Z.-Y.L. performed biological experiments and analyzed data; L.-J.S. analyzed data and organized figures; P.Z., P.-X.W. and Y.-X.J. performed omics analyses and provided important advice for this study; R.L. performed perfusion CT experiments; J.-Y.W. performed ultra-high-performance liquid chromatography–mass spectrometry experiments; S.T. established the animal hepatic IR models; X.-Y.Z. performed western blot experiments; Y.Z. performed staining experiments; R.-F.T. assisted in the performance of pig and monkey surgeries; L.W. collected clinical human liver and serum samples; X.-L.M., Z.H. and Z.-G.S. helped design the project and edited the manuscript; and H.L. designed experiments, wrote the manuscript and supervised the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–22 & Supplementary Tables 1–6 (PDF 7699 kb)
Life Sciences Reporting Summary
Life Sciences Reporting Summary (PDF 164 kb)
Rights and permissions
About this article
Cite this article
Zhang, XJ., Cheng, X., Yan, ZZ. et al. An ALOX12–12-HETE–GPR31 signaling axis is a key mediator of hepatic ischemia–reperfusion injury. Nat Med 24, 73–83 (2018). https://doi.org/10.1038/nm.4451
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4451
This article is cited by
-
Dynamic changes in the mouse hepatic lipidome following warm ischemia reperfusion injury
Scientific Reports (2024)
-
Yin/Yang associated differential responses to Psoralea corylifolia Linn. In rat models: an integrated metabolomics and transcriptomics study
Chinese Medicine (2023)
-
Interplay Between Inflammatory-immune and Interleukin-17 Signalings Plays a Cardinal Role on Liver Ischemia-reperfusion Injury—Synergic Effect of IL-17Ab, Tacrolimus and ADMSCs on Rescuing the Liver Damage
Stem Cell Reviews and Reports (2023)
-
Effects of toxicants on endoplasmic reticulum stress and hepatic cell fate determination
Toxicological Research (2023)
-
LINE-1 promotes tumorigenicity and exacerbates tumor progression via stimulating metabolism reprogramming in non-small cell lung cancer
Molecular Cancer (2022)