Abstract
Background
The obesity paradox suggests that individuals with obesity may have a survival advantage against specific critical illnesses, including sepsis. However, whether this paradox occurs at younger ages remains unclear. Therefore, we aimed to investigate whether obesity could improve survival in younger adult patients with sepsis.
Methods
We used clinical data sourced from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Patients with Sequential Organ Failure Assessment score ≥2 and suspected infection at the time of ICU admission were identified as having sepsis, following the Sepsis-3 definition. Individuals were classified into the obesity (BMI ≥30 kg/m²) and non-obesity (BMI <30 kg/m²) groups. Patients aged <50 and ≥50 years were categorized as younger adult patients and older patients, respectively.
Results
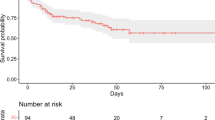
Of 73,181 patients in the MIMIC-IV ICU database, 18,120 satisfied the inclusion criteria: 2642 aged <50 years and 15,478 aged ≥50 years. The Kaplan–Meier curve showed that obesity was not associated with an improved mortality rate among younger adult patients with sepsis (log-rank test: P = 0.197), while obesity exhibited a survival benefit in older patients with sepsis (log-rank test: P < 0.001). After propensity score matching, in-hospital mortality did not differ significantly between the obesity and non-obesity groups (13.3% vs. 12.2%; P = 0.457) in the younger adult patients with sepsis. Multivariate logistic regression analysis revealed that BMI was not an independent risk factor for in-hospital mortality in younger adult patients with sepsis (underweight: adjusted odds ratio [aOR] 1.72, P = 0.076; overweight: aOR 0.88, P = 0.437; obesity: aOR 0.93, P = 0.677; and severe obesity: aOR 1.22, P = 0.580, with normal weight as the reference).
Conclusion
Contrary to findings regarding older patients with sepsis, our findings suggest that the obesity paradox does not apply to younger adult patients with sepsis.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The dataset analyzed in the current study is available on the MIMIC-IV website (https://physionet.org/content/mimiciv/2.2/).
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Liu V, Escobar GJ, Greene JD, Soule J, Whippy A, Angus DC, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. Jama. 2014;312:90–2.
Torio CM, Moore BJ. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2013. In. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US), Rockville (MD), 2006.
Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet. 2020;395:200–11.
Ramón-Arbués E, Martínez-Abadía B, Gracia-Tabuenca T, Yuste-Gran C, Pellicer-García B, Juárez-Vela R, et al. Prevalence of overweight/obesity and its association with diabetes, hypertension, dyslipidemia and metabolic syndrome: a cross-sectional study of a sample of workers in Aragón, Spain. Nutr Hosp. 2019;36:51–9.
Gomis R, Artola S, Conthe P, Vidal J, Casamor R, Font B. Prevalence of type 2 diabetes mellitus in overweight or obese outpatients in Spain. OBEDIA Study. Med Clin (Barc). 2014;142:485–92.
Zhang L, Zhang WH, Zhang L, Wang PY. Prevalence of overweight/obesity and its associations with hypertension, diabetes, dyslipidemia, and metabolic syndrome: a survey in the suburban area of Beijing, 2007. Obes Facts. 2011;4:284–9.
Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207:928–34.
Sun X, Yan AF, Shi Z, Zhao B, Yan N, Li K, et al. Health consequences of obesity and projected future obesity health burden in China. Obes (Silver Spring). 2022;30:1724–51.
Wang HE, Griffin R, Judd S, Shapiro NI, Safford MM. Obesity and risk of sepsis: a population-based cohort study. Obes (Silver Spring). 2013;21:E762–9.
Kaplan JM, Nowell M, Lahni P, Shen H, Shanmukhappa SK, Zingarelli B. Obesity enhances sepsis-induced liver inflammation and injury in mice. Obes (Silver Spring). 2016;24:1480–8.
Vachharajani V, Russell JM, Scott KL, Conrad S, Stokes KY, Tallam L, et al. Obesity exacerbates sepsis-induced inflammation and microvascular dysfunction in mouse brain. Microcirculation. 2005;12:183–94.
Petronilho F, Giustina AD, Nascimento DZ, Zarbato GF, Vieira AA, Florentino D, et al. Obesity exacerbates sepsis-induced oxidative damage in organs. Inflammation. 2016;39:2062–71.
Kuperman EF, Showalter JW, Lehman EB, Leib AE, Kraschnewski JL. The impact of obesity on sepsis mortality: a retrospective review. BMC Infect Dis. 2013;13:377.
Sakr Y, Alhussami I, Nanchal R, Wunderink RG, Pellis T, Wittebole X, et al. Being overweight is associated with greater survival in ICU patients: results from the intensive care over nations audit. Crit Care Med. 2015;43:2623–32.
Pepper DJ, Demirkale CY, Sun J, Rhee C, Fram D, Eichacker P, et al. Does obesity protect against death in sepsis? A retrospective cohort study of 55,038 adult patients. Crit Care Med. 2019;47:643–50.
Wang S, Liu X, Chen Q, Liu C, Huang C, Fang X. The role of increased body mass index in outcomes of sepsis: a systematic review and meta-analysis. BMC Anesthesiol. 2017;17:118.
Yeo HJ, Kim TH, Jang JH, Jeon K, Oh DK, Park MH, et al. Obesity paradox and functional outcomes in sepsis: a multicenter prospective study. Crit Care Med. 2023;51:742–52.
Ahima RS. Adipose tissue as an endocrine organ. Obes (Silver Spring). 2006;14:242s–9s.
Hillenbrand A, Xu P, Zhou S, Blatz A, Weiss M, Hafner S, et al. Circulating adipokine levels and prognostic value in septic patients. J Inflamm (Lond). 2016;13:30.
Niedziela J, Hudzik B, Niedziela N, Gąsior M, Gierlotka M, Wasilewski J, et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol. 2014;29:801–12.
Martin GS, Mannino DM, Moss M. The effect of age on the development and outcome of adult sepsis. Crit Care Med. 2006;34:15–21.
Abbate LM, Perman SM, Clambey ET, Van Pelt RE, Ginde AA. Age modifies the association between obesity and mortality in individuals hospitalized with severe sepsis. J Am Geriatr Soc. 2016;64:882–3.
Michels EHA, Butler JM, Reijnders TDY, Cremer OL, Scicluna BP, Uhel F, et al. Association between age and the host response in critically ill patients with sepsis. Crit Care. 2022;26:385.
Johnson AEW, Bulgarelli L, Shen L, Gayles A, Shammout A, Horng S, et al. MIMIC-IV, a freely accessible electronic health record dataset. Sci Data. 2023;10:1.
Johnson A, Bulgarelli L, Pollard T, Horng S, Celi LA, Mark R. MIMIC-IV (version 2.2). PhysioNet. https://doi.org/10.13026/6mm1-ek67 (2023).
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Bai L, Huang J, Wang D, Zhu D, Zhao Q, Li T, et al. Association of body mass index with mortality of sepsis or septic shock: an updated meta-analysis. J Intensive Care. 2023;11:27.
Saini A, Al-Shanti N, Stewart CE. Waste management - cytokines, growth factors and cachexia. Cytokine Growth Factor Rev. 2006;17:475–86.
Hasselgren PO, Fischer JE. The ubiquitin-proteasome pathway: review of a novel intracellular mechanism of muscle protein breakdown during sepsis and other catabolic conditions. Ann Surg. 1997;225:307–16.
Pepper DJ, Sun J, Welsh J, Cui X, Suffredini AF, Eichacker PQ. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: a systematic review and meta-analysis. Crit Care. 2016;20:181.
Karampela I, Christodoulatos GS, Dalamaga M. The role of adipose tissue and adipokines in sepsis: inflammatory and metabolic considerations, and the obesity paradox. Curr Obes Rep. 2019;8:434–57.
Hajri T, Gharib M, Kaul S, Karpeh MS Jr. Association between adipokines and critical illness outcomes. J Trauma Acute Care Surg. 2017;83:507–19.
Siegl D, Annecke T, Johnson BL III, Schlag C, Martignoni A, Huber N, et al. Obesity-induced hyperleptinemia improves survival and immune response in a murine model of sepsis. Anesthesiology 2014;121:98–114.
Robinson J, Swift-Scanlan T, Salyer J. Obesity and 1-year mortality in adults after sepsis: a systematic review. Biol Res Nurs. 2020;22:103–13.
Jagan N, Morrow LE, Walters RW, Plambeck RW, Wallen TJ, Patel TM, et al. Sepsis and the obesity paradox: size matters in more than one way. Crit Care Med. 2020;48:e776–e82.
Hainer V, Aldhoon-Hainerová I. Obesity paradox does exist. Diabetes Care. 2013;36:S276–81.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontology Ser A. 2006;61:1059–64.
De Lorenzo A, Pellegrini M, Gualtieri P, Itani L, El Ghoch M, Di Renzo L. The risk of sarcopenia among adults with normal-weight obesity in a nutritional management setting. Nutrients. 2022;14:5295.
Roberts S, Collins P, Rattray M. Identifying and managing malnutrition, frailty and sarcopenia in the community: a narrative review. Nutrients. 2021;13:2316.
Kim JW, Kim R, Choi H, Lee SJ, Bae GU. Understanding of sarcopenia: from definition to therapeutic strategies. Arch Pharm Res. 2021;44:876–89.
Cannataro R, Carbone L, Petro JL, Cione E, Vargas S, Angulo H, et al. Sarcopenia: etiology, nutritional approaches, and miRNAs. Int J Mol Sci. 2021;22:9724.
Yuan S, Larsson SC. Epidemiology of sarcopenia: prevalence, risk factors, and consequences. Metabolism. 2023;144:155533.
Faulkner JA, Larkin LM, Claflin DR, Brooks SV. Age-related changes in the structure and function of skeletal muscles. Clin Exp Pharm Physiol. 2007;34:1091–6.
Senior HE, Henwood TR, Beller EM, Mitchell GK, Keogh JW. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 2015;82:418–23.
Wannamethee SG, Atkins JL. Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. Proc Nutr Soc. 2015;74:405–12.
Nikolich-Žugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol. 2018;19:10–9.
Martín S, Pérez A, Aldecoa C. Sepsis and immunosenescence in the elderly patient: a review. Front Med (Lausanne). 2017;4:20.
Acknowledgements
We appreciate the Medical Illustration & Design (MID) team, a member of Medical Research Support Services of Yonsei University College of Medicine, for their excellent support with medical illustration.
Author information
Authors and Affiliations
Contributions
KJH and PSH conceived the idea for the study. LY contributed to data curation, formal analysis, investigation, visualization, and original draft writing. AJY, JSJ, KNS, CJY, YJ, and KJH contributed to supervision. All authors contributed to the review and editing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Institutional Review Board of the Beth Israel Deaconess Medical Center approved the study and waived the requirement for informed consent (IRB Protocol #2001P001699).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, Y., Ahn, S., Han, M. et al. The obesity paradox in younger adult patients with sepsis: analysis of the MIMIC-IV database. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01523-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41366-024-01523-5