Abstract
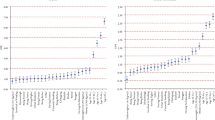
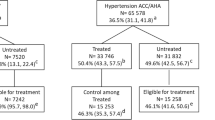
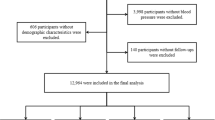
We analyzed the Bangladesh Demographic and Health Survey 2011 data to examine absolute differences in hypertension prevalence according to the hypertension definition of the “2017 American College of Cardiology/American Heart Association (2017 ACC/AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults” and “Seventh Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7)” 2003 guidelines. Among 7839 participants ≥35 years, the JNC7 and 2017 ACC/AHA classified 25.7% (95% confidence interval (CI): 24.5–27.0%) and 48.0% (95% CI: 46.4–49.7%) people hypertensive, respectively. The JNC7 prevalence was 19.4% (95% CI: 18.0-21.0%) among males and 31.9% (95% CI: 30.1-33.6%) among females. The prevalence was 41.4% (95% CI: 39.4-43.5%) among males and 54.5% (95% CI: 52.4-56.4%) among females as per the 2017 ACC/AHA guideline. From JNC7 to 2017 ACC/AHA, the overall difference in prevalence was 22.3% (95% CI: 19.8–24.8%). Males and females had similar differences, 22.0% (95% CI: 18.3–25.7%) and 22.6% (95% CI: 19.4–26.0%), respectively. As per the 2017 ACC/AHA guideline, >50% prevalence was observed among people with body mass index ≥25 kg/m2, college-level education, co-morbid diabetes, richest wealth quintile, females, age ≥55 years, urban residence, or living in Khulna, Rangpur or Dhaka divisions; the absolute difference was >20% in most categories. We found a substantial increase in the prevalence of hypertension due to change in blood pressure thresholds as per the 2017 ACC/AHA guideline. We recommend conducting more comprehensive population-based studies to estimate the recent burden of hypertension in Bangladesh. Future studies should estimate similar prevalence in other countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55.
Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62:18–26.
Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014;43:116–28.
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2:634–47.
National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. Bangladesh Demographic and Health Survey 2011. 2013.
World Health Organization. Non-communicable disease risk factor survey Bangladesh 2010. Dhaka: WHO; 2011.
National Institute of Population Research and Training (NIPORT), Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2014. 2016.
Chalmers J, et al. 1999 World Health Organization - International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Committee. J Hypertens. 1999;17:151–83.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
Whelton PK, Carey RM, Aronow WS, Casey DEJ, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017:HYP.0000000000000065.
Lewington S,Clarke R,Qizilbash N,Peto R,Collins R,Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383:1899–911.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–6.
Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT,Jr, et al. Potential U.S. Population Impact of the 2017 American College of Cardiology/American Heart Association High Blood Pressure Guideline. Circulation 2017:137. https://doi.org/10.1161/CIRCULATIONAHA.117.032582.
Bangladesh Bureau of Statistics. Bangladesh Population and Housing Census. 2011.
Jolliffe IT, Cadima J. Principal component analysis: a review and recent developments. Philos Trans A Math Phys Eng Sci. 2016;374:20150202.
Filmer D, Pritchett LH. Estimating wealth effects without expenditure data--or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32.
Stata Corporation. Stata Statistical Software. Release 14.0. College Station, TX: StataCorp LP: Stata Corporation; 2015.
Khera R, Lu Y, Saxena A, Nasir K, Krumholz HM. The impact of 2017 ACC/AHA Guidelines on the prevalence of hypertension and eligibility for anti-hypertensive therapy in the United States and China. bioRxiv. 2017:218859. https://doi.org/10.1101/218859.
Mahajan R. Joint National Committee 8 report: How it differ from JNC 7. Int J Appl Basic Med Res. 2014;4:61–62.
Seedat Y. Hypertension in developing nations in sub-Saharan Africa. J Hum Hypertens. 2000;14:739.
Fuentes R, Ilmaniemi N, Laurikainen E, Tuomilehto J, Nissinen A. Hypertension in developing economies: a review of population‐based studies carried out from 1980 to 1998. J Hypertens. 2000;18:521–9.
Chockalingam A, Campbell NR, Fodor JG. Worldwide epidemic of hypertension. Can J Cardiol. 2006;22:553–5.
Deuboue Tchialeu RI, Yaya S, Labonte R. Health systems readiness to manage the hypertension epidemic in primary health care facilities in the Western Cape, South Africa: a study protocol. JMIR Res Protoc. 2016;5:e35.
Campbell NR, Niebylski ML, World Hypertension League Executive. Prevention and control of hypertension: developing a global agenda. Curr Opin Cardiol. 2014;29:324–30.
Biswas T, Pervin S, Tanim MIA, Niessen L, Islam A. Bangladesh policy on prevention and control of non-communicable diseases: a policy analysis. BMC Public Health. 2017;17:582-017-4494-2.
World Health Organization (WHO). About 9 Voluntary Targets. 2017. http://www.who.int/nmh/ncd-tools/definition-targets/en/. Accessed 26 Feb 2017.
Marquez-Contreras E, de la Figuera Von Wichmann M, Aguilera de la Fuente MT, Garrido Garcia J. The influence of correct blood pressure measurement on the diagnostic decisions in hypertensive patients. MEDIDA study. Med Clin. 2008;131:321–5.
Harshfield E, Chowdhury R, Harhay MN, Bergquist H, Harhay MO. Association of hypertension and hyperglycaemia with socioeconomic contexts in resource-poor settings: the Bangladesh Demographic and Health Survey. Int J Epidemiol. 2015;44:1625–36.
Acknowledgements
We thank the ICF International, Rockville, Maryland, USA for giving us the permission to use the data for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kibria, G.A., Swasey, K., Choudhury, A. et al. The new 2017 ACC/AHA guideline for classification of hypertension: changes in prevalence of hypertension among adults in Bangladesh. J Hum Hypertens 32, 608–616 (2018). https://doi.org/10.1038/s41371-018-0080-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0080-z
This article is cited by
-
Prevalence and associated factors of hypertension among South African adults: findings from the Demographic and Health Survey 2016
Journal of Public Health (2023)
-
Prevalence of high blood pressure under 2017 ACC/AHA guidelines: a systematic review and meta-analysis
Journal of Human Hypertension (2021)
-
The impact of 2017 ACC/AHA guideline on the prevalence of hypertension in Australia
Journal of Human Hypertension (2021)
-
Prevalence of and factors associated with hypertension according to JNC 7 and ACC/AHA 2017 guidelines in Bangladesh
Scientific Reports (2021)
-
Prevalence and Risk Factors of Hypertension Among Young Adults in Albania
High Blood Pressure & Cardiovascular Prevention (2021)