Abstract
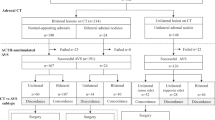
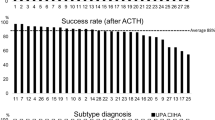
Primary aldosteronism (PA) is mainly treated by mineralocorticoid receptor antagonists or laparoscopic adrenalectomy (LA), but the effectiveness of surgical versus medical treatment in patients with adrenal venous sampling (AVS)-proven unilateral PA is unclear. Fifty-one consecutive patients with AVS-proven PA were enrolled. We compared the therapeutic effects between the surgery group (n = 21) and medication group (n = 30) by evaluating the complete control rate (CCR) of hypertension, blood pressure (BP), and number of antihypertensive drugs after a long-term follow-up (>12 months). The CCR of hypertension was assessed using a multivariate adjusted Cox proportional hazards regression model. After a mean follow-up of 21.18 ± 5.35 months, the CCR was significantly higher in the surgery than medication group (85.7% vs. 13.3%, respectively; p < 0.001). Before adjustment for covariates, the CCR of hypertension in patients who underwent LA was 7.75 times higher than that in patients who underwent medical treatment (95% CI, 2.33–25.78; p = 0.001); significant results were also shown in the adjusted models. Systolic and diastolic BP were also lower in the surgery than medication group (120.3 ± 12.99 vs. 133.54 ± 16.60 and 79.00 ± 7.62 vs. 87.35 ± 12.36 mmHg, respectively; p = 0.01 for both), as was the number of antihypertensive drugs (0.19 ± 0.51 vs. 2.33 ± 0.78, respectively; p < 0.001). The rate of hypokalemia was not significantly different between the two groups (0.0% vs. 13.3%, respectively; p = 0.13). In conclusion, AVS plays an essential role in the subtype diagnosis of PA, and surgical candidates with AVS-proven unilateral PA should be highly suggested to undergo LA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003;16(11 Pt 1):925–30.
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:3266–81.
Young WF, Jr. Minireview: primary aldosteronism-changing concepts in diagnosis and treatment. Endocrinology. 2003;144:2208–13.
Steichen O, Zinzindohoue F, Plouin PF, Amar L. Outcomes of adrenalectomy in patients with unilateral primary aldosteronism: a review. Horm Metab Res. 2012;44:221–7.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, et al. Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med. 2008;168:80–5.
Byrd JB, Turcu AF, Auchus RJ. Primary aldosteronism. Circulation. 2018;138:823–35.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Funder JW. Mineralocorticoid receptor antagonists: emerging roles in cardiovascular medicine. Integr Blood Press Control. 2013;6:129–38.
Harris DA, Au-Yong I, Basnyat PS, Sadler GP, Wheeler MH. Review of surgical management of aldosterone secreting tumours of the adrenal cortex. Eur J Surg Oncol. 2003;29:467–74.
Miyake Y, Tanaka K, Nishikawa T, Naruse M, Takayanagi R, Sasano H, et al. Prognosis of primary aldosteronism in Japan: results from a nationwide epidemiological study. Endocr J. 2014;61:35–40.
Rossi GP, Bolognesi M, Rizzoni D, Seccia TM, Piva A, Porteri E, et al. Vascular remodeling and duration of hypertension predict outcome of adrenalectomy in primary aldosteronism patients. Hypertension. 2008;51:1366–71.
Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension. 2013;62:62–9.
Lin YH, Lin LY, Chen A, Wu XM, Lee JK, Su TC, et al. Adrenalectomy improves increased carotid intima-media thickness and arterial stiffness in patients with aldosterone producing adenoma. Atherosclerosis. 2012;221:154–9.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Arlt W. A detour guide to the Endocrine Society Clinical Practice Guideline on case detection, diagnosis and treatment of patients with primary aldosteronism. Eur J Endocrinol. 2010;162:435–8.
Song Y, Yang S, He W, Hu J, Cheng Q, Wang Y, et al. Confirmatory tests for the diagnosis of primary aldosteronism: a prospective diagnostic accuracy study. Hypertension. 2018;71:118–24.
Cronin C, Igoe D, Duffy MJ, Cunningham SK, McKenna TJ. The overnight dexamethasone test is a worthwhile screening procedure. Clin Endocrinol (Oxf). 1990;33:27–33.
Jain A, Baracco R, Kapur G. Pheochromocytoma and paraganglioma-an update on diagnosis, evaluation, and management. Pediatr Nephrol 2019. [Epub ahead of print].
Betz MJ, Degenhart C, Fischer E, Pallauf A, Brand V, Linsenmaier U, et al. Adrenal vein sampling using rapid cortisol assays in primary aldosteronism is useful in centers with low success rates. Eur J Endocrinol. 2011;165:301–6.
Wang F, Liu J, Zhang R, Bai Y, Li C, Li B, et al. CT and MRI of adrenal gland pathologies. Quant Imaging Med Surg. 2018;8:853–75.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165:710–8.
Young WF, Jr. Diagnosis and treatment of primary aldosteronism: practical clinical perspectives. J Intern Med. 2018;285:126–48.
Deinum J, Riksen NP, Lenders JW. Pharmacological treatment of aldosterone excess. Pharm Ther. 2015;154:120–33.
Yang YK, Zhang Y, Meng X, Yang KQ, Jiang XJ, Wu HY, et al. Clinical characteristics and treatment of renal artery fibromuscular dysplasia with percutaneous transluminal angioplasty: a long-term follow-up study. Clin Res Cardiol. 2016;105:930–7.
Dekkers T, Prejbisz A, Kool LJS, Groenewoud H, Velema M, Spiering W, et al. Adrenal vein sampling versus CT scan to determine treatment in primary aldosteronism: an outcome-based randomised diagnostic trial. Lancet Diabetes Endocrinol. 2016;4:739–46.
Wachtel H, Cerullo I, Bartlett EK, Kelz RR, Cohen DL, Karakousis GC, et al. Long-term blood pressure control in patients undergoing adrenalectomy for primary hyperaldosteronism. Surgery. 2014;156:1394–402.
Zhang X, Zhu Z, Xu T, Shen Z. Factors affecting complete hypertension cure after adrenalectomy for aldosterone-producing adenoma: outcomes in a large series. Urol Int. 2013;90:430–4.
Sawka AM, Young WF, Thompson GB, Grant CS, Farley DR, Leibson C, et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001;135:258–61.
Benham JL, Eldoma M, Khokhar B, Roberts DJ, Rabi DM, Kline GA. Proportion of patients with hypertension resolution following adrenalectomy for primary aldosteronism: a systematic review and meta-analysis. J Clin Hypertens (Greenwich). 2016;18:1205–12.
Zhou Y, Zhang M, Ke S, Liu L. Hypertension outcomes of adrenalectomy in patients with primary aldosteronism: a systematic review and meta-analysis. BMC Endocr Disord. 2017;17:61.
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Katabami T, Fukuda H, Tsukiyama H, Tanaka Y, Takeda Y, Kurihara I, et al. Clinical and biochemical outcomes after adrenalectomy and medical treatment in patients with unilateral primary aldosteronism. J Hypertens. 2019;37:1513–20.
Hannon MJ, Sze WC, Carpenter R, Parvanta L, Matson M, Sahdev A, et al. Clinical outcomes following unilateral adrenalectomy in patients with primary aldosteronism. QJM. 2017;110:277–81.
Tagawa M, Ghosn M, Wachtel H, Fraker D, Townsend RR, Trerotola S, et al. Lateralization index but not contralateral suppression at adrenal vein sampling predicts improvement in blood pressure after adrenalectomy for primary aldosteronism. J Hum Hypertens. 2017;31:444–9.
Loh WJ, Lim DST, Loh LM, Kek PC. Factors associated with resolution of hypertension after adrenalectomy in patients with primary aldosteronism. Endocrinol Metab (Seoul). 2018;33:355–63.
Aronova A, Gordon BL, Finnerty BM, Zarnegar R, Fahey TJ 3rd. Aldosteronoma resolution score predicts long-term resolution of hypertension. Surgery. 2014;156:1387–92.
Zarnegar R, Young WF Jr., Lee J, Sweet MP, Kebebew E, Farley DR, et al. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg. 2008;247:511–8.
Acknowledgements
This work was supported by the National Key Research and Development Plan of China [grant number 2016YFC1300100], the CAMS Innovation Fund for Medical Science [grant number 2016-I2M-1-002], and the PUMC Youth Fund [grant number 2017-XHQN07].
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41371_2019_241_MOESM1_ESM.docx
Supplementary Table 1. Changes in blood pressure and serum potassium level at follow-up in surgery group and medication group
Rights and permissions
About this article
Cite this article
Meng, X., Ma, WJ., Jiang, XJ. et al. Long-term blood pressure outcomes of patients with adrenal venous sampling-proven unilateral primary aldosteronism. J Hum Hypertens 34, 440–447 (2020). https://doi.org/10.1038/s41371-019-0241-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0241-8