Abstract
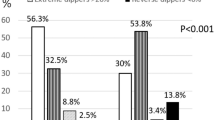
Although vascular and autonomic nervous system have been involved in the regulation of morning surge in blood pressure (MBPS), data on clinical correlates of MBPS in diabetic population are scarce, in particular with regard to diabetic complications. This study was aimed at investigating predictors and correlates of MBPS in diabetes. In a cross-sectional study including 167 patients with diabetes (age 58.5 ± 11.1 years, duration 15.9 ± 12.1 years), clinical variables, diabetic and neuropathic complications, and MBPS (using 24-h ambulatory blood pressure monitoring) were measured. The upper quartile of MBPS (>30.5 mmHg) was associated with higher values of waist circumference (P = 0.027), triglycerides (P = 0.021), and Michigan Diabetic Neuropathy Score (P = 0.042), with lower HDL cholesterol (P = 0.030), and with the presence of cardiovascular autonomic neuropathy (CAN) (P = 0.016) and peripheral vascular disease (PVD) (P < 0.0001). In a logistic regression analysis, PVD (odds ratio: 10.2, P = 0.001), CAN (odds ratio: 6.09, P = 0.016), and diastolic blood pressure (BP) (odds ratio: 1.06, P = 0.022) predicted MBPS upper quartile (r2 = 0.20, P = 0.0005). In a multiple regression analysis, PVD (P = 0.002) and diastolic BP (P = 0.003) were the only determinants of MBPS (r2 = 0.20). MBPS upper quartile was associated with BP dipping (systolic BP day–night reduction > 10%) (P = 0.012), and MBPS was positively related to systolic (rho = 0.41, P < 0.0001) and diastolic BP day–night reduction. In conclusion, metabolic syndrome stigmata, diastolic BP, CAN and PVD are the main predictors of MBPS in the diabetic population. Excessive MBPS and nondipping are not concurrent 24-h BP alterations. Autonomic dysfunction might exert an exacerbating effect on MBPS phenomenon.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Spallone V. Blood pressure variability and autonomic dysfunction. Curr Diab Rep. 2018;18:137.
Kario K. Prognosis in relation to blood pressure variability: pro side of the argument. Hypertension. 2015;65:1163–9.
Li Y, Thijs L, Hansen TW, Hansen TW, Kikuya M, Boggia J, et al. Prognostic value of the morning blood pressure surge in 5645 subjects from 8 populations. Hypertension. 2010;55:1040–8.
Sheppard JP, Hodgkinson J, Riley R, Martin U, Bayliss S, McManus RJ. Prognostic significance of the morning blood pressure surge in clinical practice: a systematic review. Am J Hypertens. 2015;28:30–41.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–6.
Kario K. New insight of morning blood pressure surge into the triggers of cardiovascular disease-synergistic resonance of blood pressure variability. Am J Hypertens. 2016;29:14–6.
Sogunuru GP, Kario K, Shin J, Chen CH, Buranakitjaroen P, Chia YC, et al. Morning surge in blood pressure and blood pressure variability in Asia: Evidence and statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2019;21:324–34.
Hermida RC, Ayala DE, Mojón A, Fernández JR. Sleep-time blood pressure as a therapeutic target for cardiovascular risk reduction in type 2 diabetes. Am J Hypertens. 2012;25:325–34.
Hoshide S, Kario K, de la Sierra A, Bilo G, Schillaci G, Banegas JR, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study. Hypertension. 2015;66:750–6.
Head GA, Andrianopoulos N, McGrath BP, Martin CA, Carrington MJ, Lukoshkova EV, et al. Predictors of mean arterial pressure morning rate of rise and power function in subjects undergoing ambulatory blood pressure recording. PLoS ONE. 2014;9:e93186.
Özpelit ME, Özpelit E, Doğan NB, Pekel N, Ozyurtlu F, Yılmaz A, et al. Impact of anxiety level on circadian rhythm of blood pressure in hypertensive patients. Int J Clin Exp Med. 2015;8:16252–8.
Yoda K, Inaba M, Hamamoto K, Yoda M, Tsuda A, Mori K, et al. Association between glycemic control and morning blood pressure surge with vascular endothelial dysfunction in type 2 diabetic patients. Diabetes Care. 2014;37:644–50.
Afsar B, Elsurer R. The relationship between central haemodynamics, morning blood pressure surge, glycemic control and sodium intake in patient with type 2 diabetes mellitus and essential hypertension. Diabetes Res Clin Pr. 2014;104:420–6.
Barbieri M, Rizzo MR, Fava I, Sardu C, Angelico N, Paolisso P, et al. Awaking blood pressure surge and progression to microalbuminuria in type 2 normotensive diabetic patients. J Diabetes Res. 2016;2016:5876792.
Najafi MT, Khaloo P, Alemi H, Jaafarinia A, Blaha MJ, Mirbolouk M, et al. Ambulatory blood pressure monitoring and diabetes complications: Targeting morning blood pressure surge and nocturnal dipping. Med (Baltim). 2018;97:e12185.
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91.
Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med. 2005;6:41–4.
Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33:2285–93.
Petrie A, Sabin C. Medical statistics at a glance. 1st ed. Oxford: Blackwell Science Ltd; 2000.
Spallone V. Update on the impact, diagnosis and management of cardiovascular autonomic neuropathy in diabetes: what is defined, what is new, and what is unmet. Diabetes Metab J. 2019;43:3–30.
Marfella R, Siniscalchi M, Portoghese M, Di Filippo C, Ferraraccio F, Schiattarella C, et al. Morning blood pressure surge as a destabilizing factor of atherosclerotic plaque: role of ubiquitin-proteasome activity. Hypertension. 2007;49:784–91.
Pòlonia J, Amado P, Barbosa L, Nazaré J, Silva JA, Bertoquini S, et al. Morning rise, morning surge and daytime variability of blood pressure and cardiovascular target organ damage: a cross-sectional study in 743 subjects. Rev Port Cardiol. 2005;24:65–78.
Lyhne JM, Laugesen E, Høyem P, Cichosz S, Christiansen JS, Knudsen ST, et al. Morning blood pressure surge and target organ damage in newly diagnosed type 2 diabetic patients: a cross sectional study. BMC Endocr Disord. 2015;15:77.
Kario K. Orthostatic hypertension-a new haemodynamic cardiovascular risk factor. Nat Rev Nephrol. 2013;9:726–38.
Hering D, Kucharska W, Kara T, Somers VK, Narkiewicz K. Resting sympathetic outflow does not predict the morning blood pressure surge in hypertension. J Hypertens. 2011;29:2381–6.
Lambert EA, Chatzivlastou K, Schlaich M, Lambert G, Head GA. Morning surge in blood pressure is associated with reactivity of the sympathetic nervous system. Am J Hypertens. 2014;27:783–92.
Eguchi K, Tomizawa H, Ishikawa J, Hoshide S, Pickering TG, Shimada K, et al. Factors associated with baroreflex sensitivity: association with morning blood pressure. Hypertens Res. 2007;30:723–8.
Okada Y, Galbreath MM, Shibata S, Jarvis SS, Bivens TB, Vongpatanasin W, et al. Morning blood pressure surge is associated with arterial stiffness and sympathetic baroreflex sensitivity in hypertensive seniors. Am J Physiol Heart Circ Physiol. 2013;305:H793–802.
Johnson AW, Hissen SL, Macefield VG, Brown R, Taylor CE. Magnitude of morning surge in blood pressure is associated with sympathetic but not cardiac baroreflex sensitivity. Front Neurosci. 2016;10:412.
Sanchez Gelós DF, Otero-Losada ME, Azzato F, Milei J. Morning surge, pulse wave velocity, and autonomic function tests in elderly adults. Blood Press Monit. 2012;17:103–9.
Liatis S, Alexiadou K, Tsiakou A, Makrilakis K, Katsilambros N, Tentolouris N. Cardiac autonomic function correlates with arterial stiffness in the early stage of type 1 diabetes. Exp Diabetes Res. 2011;2011:957901.
Prince CT, Secrest AM, Mackey RH, Arena VC, Kingsley LA, Orchard TJ. Cardiovascular autonomic neuropathy, HDL cholesterol, and smoking correlate with arterial stiffness markers determined 18 years later in type 1 diabetes. Diabetes Care. 2010;33:652–7.
Cho JS, Ihm SH, Kim CJ, Park MW, Her SH, Park GM, et al. Obstructive sleep apnea using watch-PAT 200 is independently associated with an increase in morning blood pressure surge in never-treated hypertensive patients. J Clin Hypertens (Greenwich). 2015;17:675–81.
Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Ramundo E, Gentile G, et al. Day-night dip and early morning surge in blood pressure in hypertension; prognostic implications. Hypertension. 2012;60:34–42.
FitzGerald L, Ottaviani C, Goldstein IB, Shapiro D. Effects of dipping and psychological traits on morning surge in blood pressure in healthy people. J Hum Hypertens. 2012;26:228–35.
Kario K. Perfect 24-h management of hypertension: clinical relevance and perspectives. J Hum Hypertens. 2017;31:231–43.
Acknowledgements
Part of this study was presented at the 24th Annual Meeting of the Diabetic Neuropathy Study Group of the European Association for the Study of Diabetes (NEURODIAB), 12–14 September 2014, Sopron, Hungary.
Author information
Authors and Affiliations
Contributions
FDG and CD designed the study, researched, extracted, and analysed data and wrote the manuscript; RM, CG, DC, SL, MC contributed to the design, researched data, contributed to the discussion and revised the manuscript. DL contributed to the design and to the discussion and reviewed the manuscript. VS designed and conducted the study, researched and analysed data and wrote the manuscript. All the authors approved the version to be published. VS is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Di Gennaro, F., D’Amato, C., Morganti, R. et al. Morning blood pressure surge is associated with autonomic neuropathy and peripheral vascular disease in patients with diabetes. J Hum Hypertens 34, 495–504 (2020). https://doi.org/10.1038/s41371-019-0270-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0270-3
This article is cited by
-
High dose cholecalciferol supplementation causing morning blood pressure reduction in patients with type 1 diabetes mellitus and cardiovascular autonomic neuropathy
Scientific Reports (2024)
-
Evaluating treatment options for cardiovascular autonomic neuropathy in patients with diabetes mellitus: a systematic review
Diabetology International (2023)