Abstract
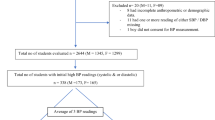
The prevalence of childhood hypertension is recognized as an important parameter of cardiovascular risk in adults. This retrospective study aimed to ascertain the prevalence and risk factors for hypertension from birth through childhood as of 2014. Stratified cluster sampling was used to select 17,007 participants (5971 with biochemical indexes available) aged 6–12 years on two avenues per region in urban, suburban, and rural areas. The prevalence of hypertension was 12.55%; children with obesity combined with rural residence, low family income, birth weight (<3000 g) (BWP25) or >10 months of breastfeeding had a significantly elevated prevalence of hypertension (37.06%, 30.41%, 30.04%, and 30.84%, respectively). Obesity and heart rate were the significant anthropometric determinants; gestational hypertension, BWP25 and >10 months of breastfeeding were the significant perinatal determinants; rural residence was the significant socioeconomic determinant; fasting blood glucose, triglycerides, and low-density lipoprotein cholesterol were the significant serum biochemical determinants; and red blood cell counts and platelet counts were the significant haematological determinants of childhood hypertension. The adjusted R2 values were 14.45% and 24.88% in the full models excluding and including serum indexes, respectively. We observed a notable prevalence of hypertension in a large paediatric sample. Obesity, high heart rate, BWP25, >10 months of breastfeeding, low family income, rural residence, abnormal lipid metabolism, and abnormal blood counts were associated with an increased risk of hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Zhang YX, Wang SR. Comparison of blood pressure levels among children and adolescents with different body mass index and waist circumference: study in a large sample in Shandong, China. Eur J Nutr. 2014;53:627–34.
Moyer VA. Force USPST. Screening for primary hypertension in children and adolescents: U.S. preventive services task force recommendation statement. Ann Intern Med. 2013;159:613–9.
Chen XL, Wang YF. Tracking of blood pressure from childhood to adulthood—a systematic review and meta-regression analysis. Circulation. 2008;117:3171–80.
Koskinen J, Juonala M, Dwyer T, Venn A, Petkeviciene J, Ceponiene I, et al. Utility of different blood pressure measurement components in childhood to predict adult carotid intima-media thickness. Hypertension. 2019;73:335–41.
Zhang YX, Zhao JS, Chu ZH. Children and adolescents with low body mass index but large waist circumference remain high risk of elevated blood pressure. Int J Cardiol. 2016;215:23–5.
Karatzi K, Moschonis G, Botelli S, Androutsos O, Chrousos GP, Lionis C, et al. Physical activity and sedentary behavior thresholds for identifying childhood hypertension and its phenotypes: The Healthy Growth Study. J Am Soc Hypertens. 2018;12:714–22.
He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48:861–9.
Xiao P, Huang T, Yan Y, Zhao X, Li H, Mi J. Performance of gender- and age-specific cut-points versus NCEP pediatric cutpoints in dyslipidemia screening among Chinese children. Atherosclerosis. 2018;280:37–44.
Sharma AK, Metzger DL, Rodd CJ. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 2018;172:557–65.
Liang X, Chen M, Qu P, Hao G, Huang Y, Chen J, et al. The association of vitamin A and vitamin D with hypertension in Children: a case-control study. Int J Hypertens. 2018;2018:9295147.
Li G, Zhang YY, Zhu ZW, Du J. Association between mean platelet volume and hypertension incidence. Hypertens Res. 2017;40:779–84.
Batista TR, Figueiredo RC, Rios DRA. Platelets volume indexes and cardiovascular risk factors. Rev da Associacao Med Brasileira. 2018;64:554–9.
Safar ME, Levy BI, Struijker-Boudier H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation. 2003;107:2864–9.
Liang X, Su S, Hao G, Snieder H, Treiber F, Kapuku G et al. Determinants of pulse wave velocity trajectories from youth to young adulthood: the Georgia Stress and Heart Study. J Hypertens 2018.
Butte NF, Watson KB, Ridley K, Zakeri IF, McMurray RG, Pfeiffer KA, et al. A youth compendium of physical activities: activity codes and metabolic intensities. Med Sci Sports Exerc. 2018;50:246–56.
Fan Hui, YY-k MJ. Updating blood pressure references for Chinese children aged 3-17 years. Chin J Hypertens. 2017;05:8.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127–e248.2017.
Duncombe SL, Voss C, Harris KC. Oscillometric and auscultatory blood pressure measurement methods in children: a systematic review and meta-analysis. J Hypertens. 2017;35:213–24.
Division of Nutrition PA, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Using the CDC BMI-for-age Growth Charts to Assess Growth in the United States Among Children and Teens Aged 2 Years to 20 Years. Available from: http://www.cdc.gov/growthcharts/clinical_charts.htm.
Ebrahimi H, Emamian MH, Hashemi H, Fotouhi A. Prevalence of prehypertension and hypertension and its risk factors in Iranian school children: a population-based study. J Hypertens. 2018;36:1816–24.
Rao G. Diagnosis, epidemiology, and management of hypertension in children. Pediatrics. 2016;138:e20153616.
Falkner B. Recent clinical and translational advances in pediatric hypertension. Hypertension. 2015;65:926–31.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
Lai C, Hu Y, He D, Liang L, Xiong F, Liu G, et al. U-shaped relationship between birth weight and childhood blood pressure in China. BMC Pediatr. 2019;19:264.
Mi JWT, Meng L, Zhu G, Han S, Zhong Y, et al. Development of blood pressure reference standards for Chinese children and adolecents (in Chinese). Chin J Evid Based Pediatr. 2010;5:10.
Sharma AK, Metzger DL, Rodd CJ. Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr. 2018;172:557–65.
Nobre LN, Lessa AD. Influence of breastfeeding in the first months of life on blood pressure levels of preschool children. J de Pediatr. 2016;92:588–94.
Kuhle S, Maguire B, Ata N, MacInnis N, Dodds L. Birth weight for gestational age, anthropometric measures, and cardiovascular disease markers in children. J Pediatrics. 2017;182:99–106.
Johnsson IW, Haglund B, Ahlsson F, Gustafsson J. A high birth weight is associated with increased risk of type 2 diabetes and obesity. Pediatr Obes. 2015;10:77–83.
Rich-Edwards JW, Stampfer MJ, Manson JE, Rosner B, Hu FB, Michels KB, et al. Breastfeeding during infancy and the risk of cardiovascular disease in adulthood. Epidemiology. 2004;15:550–6.
Briend A. [Complementary feeding: current recommendations]. Med Trop. 2009;69:298–302.
Clark KM, Li M, Zhu B, Liang F, Shao J, Zhang Y, et al. Breastfeeding, mixed, or formula feeding at 9 months of age and the prevalence of iron deficiency and iron deficiency anemia in two cohorts of infants in China. J Pediatr. 2017;181:56–61.
Alsnes IV, Vatten LJ, Fraser A, Bjorngaard JH, Rich-Edwards J, Romundstad PR, et al. Hypertension in Pregnancy and Offspring Cardiovascular Risk in Young Adulthood: Prospective and Sibling Studies in the HUNT Study (Nord-Trondelag Health Study) in Norway. Hypertension. 2017;69:591–8.
Ip P, Ho FK, So HK, Chan DF, Ho M, Tso W, et al. Socioeconomic gradient in childhood obesity and hypertension: a multilevel population-based study in a Chinese Community. PloS ONE. 2016;11:e0156945.
Leng B, Jin YN, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J hypertension. 2015;33:221–9.
Almasian Kia A, Rezapour A, Khosravi A, Afzali Abarghouei V. Socioeconomic inequality in malnutrition in under-5 children in Iran: evidence from the multiple indicator demographic and health survey, 2010. J Prev Med Public Health. 2017;50:201–9.
Ikeda N, Fuse K, Nishi N. Changes in the effects of living with no siblings or living with grandparents on overweight and obesity in children: results from a national cohort study in Japan. PloS ONE. 2017;12:e0175726.
Lee CJ, Lim NK, Kim HC, Ihm SH, Lee HY, Park HY, et al. Impaired fasting glucose and impaired glucose tolerance do not predict hypertension: a community cohort study. Am J Hypertens. 2015;28:493–500.
Sinnott M, Kinsley BT, Jackson AD, Walsh C, O’Grady T, Nolan JJ, et al. Fasting plasma glucose as initial screening for diabetes and prediabetes in irish adults: the diabetes mellitus and vascular health initiative (DMVhi). PloS ONE. 2015;10:e0122704.
Mozos I. Mechanisms linking red blood cell disorders and cardiovascular diseases. BioMed Res Int. 2015;2015:682054.
Marketou M, Patrianakos A, Parthenakis F, Zacharis E, Arfanakis D, Kochiadakis G, et al. Systemic blood pressure profile in hypertensive patients with low hemoglobin concentrations. Int J Cardiol. 2010;142:95–6.
Purisch SE, Gyamfi-Bannerman C. Epidemiology of preterm birth. Semin Perinatol. 2017;41:387–91.
Acknowledgements
The authors would like to acknowledge the laboratory support of the Ministry of Education Key Laboratory of Child Development and Disorders and all the staff members of the ten elementary schools in the three regions.
Funding
This study was supported by the Education Commission of Chongqing Municipality (KJQN201900443), the National Natural Science Foundation of China (81502826), the China Postdoctoral Science Foundation (2014M562289) and the Chongqing PostDoctoral Research Funded Projects (Xm2014129).
Author information
Authors and Affiliations
Contributions
XHL and XL conceived and designed the experiments; JPX and YTL performed the experiments; YTL analysed the data; XHL wrote the paper; and all authors critically reviewed and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, X., Xiao, L., Luo, Y. et al. Prevalence and risk factors of childhood hypertension from birth through childhood: a retrospective cohort study. J Hum Hypertens 34, 151–164 (2020). https://doi.org/10.1038/s41371-019-0282-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0282-z
This article is cited by
-
The burden of diabetes and hypertension on healthy life expectancy in Bangladesh
Scientific Reports (2024)
-
The associations between hematological parameters and the incidence of prehypertension and hypertension in children and adolescents: a prospective cohort study
Hypertension Research (2023)
-
Interactions among maternal smoking, breastfeeding, and offspring genetic factors on the risk of adult-onset hypertension
BMC Medicine (2022)
-
The association of quality of life and personality characteristics with adolescent metabolic syndrome: a cohort study
Health and Quality of Life Outcomes (2021)
-
The relationship between socioeconomic status and childhood overweight/obesity is linked through paternal obesity and dietary intake: a cross-sectional study in Chongqing, China
Environmental Health and Preventive Medicine (2021)