Abstract
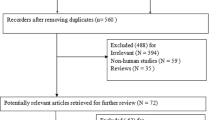
To investigate if there is evidence for a ‘legacy effect’ for blood pressure (BP) lowering treatment, that is, worse health outcomes from not initiating drug treatment at a systolic BP threshold of 140 mmHg in middle-age adults. We systematically reviewed studies comparing the effects of delayed BP treatment (placebo/untreated during the trial or no previous treatment at trial entry) vs. early treatment (actively treated during the trial or previous BP treatment at trial entry) on mortality in the short term (5-year in-trial period) and long term (≥10 years in total period). The data were pooled using Peto ORs. A subgroup analysis by 10-year Framingham risk score was performed. Three studies (ALLHAT, Oslo and PREVEND-IT) involving 4746 participants were included. The results were heavily influenced by the ALLHAT trial. We found no significant difference in all-cause mortality between ‘delayed BP’ and ‘early treatment’ in the short-term OR 0.95 (95% CI 0.68–1.32) or long-term OR 0.90 (95% CI 0.78–1.04), with similar results for mortality from cardiovascular disease (CVD). The effects of delayed BP lowering treatment on long-term all-cause and CVD mortality did not vary with baseline risk of CVD. The review showed no clinically adverse ‘legacy effect’ on mortality or major CVD event from not treating middle-aged adults at a systolic BP threshold of 140 mmHg or over. The results were consistent for all CVD risk subgroups. Although these studies are non-randomised post-hoc analyses, they may allay concerns that early treatment of elevated systolic BP is necessary to prevent CVD events in primary prevention populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265:3255–64.
Staessen JA, Fagard R, Thijs L, Celis H, Arabidze GG, Birkenhäger WH, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. Lancet. 1997;350:757–64.
Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012;8:CD006742.
Johan S, Hisatomi A, Rod J, Fiona T, Kazem R, John C, et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann Intern Med. 2015;162:184–91.
DREAM Trial Investigators. Effect of ramipril on the incidence of diabetes. N Engl J Med. 2006;355:1551–62.
Management Committee. The Australian therapeutic trial in mild hypertension. The Lancet. 1980;315:1261–7.
Bao HCL, Monique B, Doust J, Reid MC, Nelson MR. Effectiveness of blood pressure-lowering drug treatment by levels of absolute risk: post hoc analysis of the Australian national blood pressure study. BMJ Open. 2018;8:e017723.
NAVIGATOR Study Group. Effect of valsartan on the incidence of diabetes and cardiovascular events. N Engl J Med. 2010;362:1477–90.
Helgeland A. Treatment of mild hypertension: a five year controlled drug trial: the Oslo study. Am J Med. 1980;69:725–32.
Asselbergs Folkert W, Diercks Gilles FH, Hillege Hans L, van Boven AdJ, Janssen Wilbert MT, Voors Adriaan A, et al. Effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria. Circulation. 2004;110:2809–16.
Neaton James D, Grimm Richard H, Prineas Ronald J, Stamler J, Grandits Greg A, Elmer Patricia J, et al. Treatment of mild hypertension study: final results. JAMA. 1993;270:713–24.
Kostis WJ, Thijs L, Richart T, Kostis JB, Staessen JA. Persistence of mortality reduction after the end of randomized therapy in clinical trials of blood pressure-lowering medications. Hypertension. 2010;56:1060–8.
Hirakawa Y, Arima H, Rodgers A, Woodward M, Chalmers J. Cumulative in-trial and post-trial effects of blood pressure and lipid lowering: systematic review and meta-analysis. J Hypertens. 2017;35:905–13.
Ho CLB, Sanders S, Doust J, Breslin M, Reid CM, Nelson MR. Legacy effect of delayed blood pressure-lowering pharmacotherapy in middle-aged individuals stratified by absolute cardiovascular disease risk: protocol for a systematic review. JMIR Res Protoc. 2017;6:e177.
Lefebvre C, Manheimer E, Glanville J. The Cochrane highly sensitive search strategies for identifying randomized trials in MEDLINE. Cochrane Handbook for Systematic Reviews of Interventions, 2011;4.
Musini VM, Gueyffier F, Puil L, Salzwedel DM, Wright JM. Pharmacotherapy for hypertension in adults aged 18 to 59 years. Cochrane Database Syst Rev. 2017;8.
Hoes AW, Grobbee DE, Lubsen J. Does drug treatment improve survival? Reconciling the trials in mild-to-moderate hypertension. J Hypertens. 1995;13:805–11.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919
Sterne JAC, Higgins JPT, Elbers RG, Reeves BC and The Development Group for ROBINS-I. Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I): detailed guidance, updated 12 October 2016; 20 April 2019. http://www.riskofbias.info.
Higgins JPT, Sterne JAC, Savović J, Page MJ, Hróbjartsson A, Boutron I, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. 2016;10:29–31.
Nelson MR, Chowdhury EK, Doust J, Reid CM, Wing LM. Ten-year legacy effects of baseline blood pressure ‘treatment naivety’ in the second Australian national blood pressure study. J Hypertens. 2015;33:2331–7.
Brockhaus AC, Bender R, Skipka G. The Peto odds ratio viewed as a new effect measure. Stat Med. 2014;33:4861–74.
Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A. Much ado about nothing: a comparison of the performance of meta‐analytical methods with rare events. Stat Med. 2007;26:53–77.
IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25
Efthimiou O. Practical guide to the meta-analysis of rare events. Evid Based Ment Health. 2018;21:72–6.
Kuss O. Statistical methods for meta‐analyses including information from studies without any events—add nothing to nothing and succeed nevertheless. Stat Med. 2015;34:1097–116.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
National Vascular Disease Prevention Alliance. Guidelines for the management of absolute cardiovascular disease risk. National Vascular Disease Prevention Alliance. 2012.
Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506–25.
The Cochrane Collaboration. Review Manager (RevMan) [Computer program], Version 5.3. Copenhagen: The Nordic Cochrane Centre; 2014.
United States Public Health Hospitals Cooperative Study Group. Morbidity and mortality in mild essential hypertension. Circ Res. 1972;30:110–21.
Smith WM. Treatment of mild hypertension: results of a ten-year intervention trial. Circ Res. 1977;40 Suppl 1:I98–105.
The Allhat Officers and Coordinators for the Allhat Collaborative Research Group. Majoroutcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calciumchannel blocker vs diuretic: the antihypertensive and lipid-loweringtreatment to prevent heart attack trial (ALLHAT). JAMA. 2020;288:2981–97.
Leren P, Helgeland A. Coronary heart disease and treatment of hypertension some Oslo study data. Am J Med. 1986;80:3–6.
Holme I, Kjeldsen SE. Long-term survival in the randomized trial of drug treatment in mild to moderate hypertension of the Oslo study 1972-3. Eur J Intern Med. 2015;26:123–6. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/814/CN-01051814/frame.html.
Brouwers Frank P, Asselbergs Folkert W, Hillege Hans L, de Boer Rudolf A, Gansevoort Ron T, van Veldhuisen Dirk J, et al. Long-term effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria: ten years of follow-up of prevention of renal and vascular end-stage disease intervention trial (PREVEND IT). Am Heart J. 2011;161:1171–8.
Gueyffier F, Froment A, Gouton M. New meta-analysis of treatment trials of hypertension: improving the estimate of therapeutic benefit. J Hum Hypertens. 1996;10:1–8.
Patel Alpesh B, Kostis John B, Wilson Alan C, Shea Michael L, Pressel Sara L, Davis Barry R. Long-term fatal outcomes in subjects with stroke or transient ischemic attack: fourteen-year follow-up of the systolic hypertension in the elderly program. Stroke. 2008;39:1084–9.
Kostis JB, Cabrera J, Cheng JQ, Cosgrove NM, Deng Y, Pressel SL, et al. Association between chlorthalidone treatment of systolic hypertension and long-term survival. JAMA. 2011;306:2588–93.
Staessen JA, Thijsisq L, Fagard R, Celis H, Birkenhäger WH, Bulpitt CJ, et al. Effects of immediate versus delayed antihypertensive therapy on outcome in the systolic hypertension in Europe trial. J Hypertens. 2004;22:847–57.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315–81.
Acknowledgements
The researchers gratefully acknowledge the RACGP Foundation and Therapeutic Guidelines Ltd for their support of this project. We thank Dr Toshiaki Ohkuma and Prof. John Chalmers for their kind support on the enquiries related to ADVANCE and ADVANCE-ON study. We thank Mark Jones (Biostatistician, Centre for Research in Evidence Based Practice, Bond University) for his advice on statistical issues. No other funding was received from National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); or other granting bodies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
CLBH is a Ph.D. candidate at Menzies Institute for Medical Research, she has received a Ph.D. scholarship from Merle Weaver Postgraduate Scholarship. MRN has served on advisory boards for Sanofi and Bayer in the last 3 years. For the remaining authors none were declared.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ho, C.L.B., Sanders, S., Breslin, M. et al. Legacy effect of delayed blood pressure lowering drug treatment in middle-aged adults with mildly elevated blood pressure: systematic review and meta-analysis. J Hum Hypertens 34, 261–270 (2020). https://doi.org/10.1038/s41371-020-0323-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0323-7