Abstract
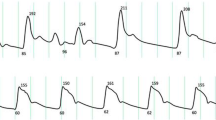
This study was conducted to evaluate whether the impact factor on the accuracy of oscillometric blood pressure (BP) is different between the patients with atrial affiliation (AF) and sinus rhythm (SR). This study included 124 AF patients and 98 SR patients who underwent coronary arteriography. Upper arm oscillometric and intro-aortic BP were simultaneously measured three times, and the averages were recorded as final values, respectively. The difference between oscillometric and intro-aortic BP was recorded as delta BP. For reducing the influence of baseline BP on delta BP, a percentage difference (PD-BP) was calculated with the formula: PD-BP = delta BP/intro-aortic BP × 100%. The oscillometric SBP and DBP levels slightly underestimated intro-aortic BP (by 2.2/1.6 mmHg) in the SR group, but significantly underestimated (by 5.8/4.8 mmHg) in the AF group. Age was negatively correlated with delta SBP and positively with delta DBP in SR patients, but not correlated in AF patients. Otherwise, ventricular rate (VR) was negatively correlated with delta SBP or delta DBP in AF, which indicated that the accuracy of oscillometric BP declined as the VR increased. With intro-aortic BP as reference, the accuracy of oscillometric BP in AF patients is lower than SR patients. Meanwhile, age may impact the oscillometric BP accuracy in SR patients, but VR may impact that in AF patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
30 July 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41371-021-00526-3
References
Wang Z, Luo Y, Yang S, Zuo M, Pei R, He J, et al. Death burden of high systolic blood pressure in Sichuan Southwest China 1990–2030. BMC Public Health. 2020;20:406.
Seo SM, Chung W-B, Choi IJ, Koh Y-S, Ihm S-H, Kim P-J, et al. Visit-to-visit variability of systolic blood pressure predicts all-cause mortality in patients received percutaneous coronary intervention with drug-eluting stents. Heart Vessels. 2018;33:489–97.
Giuliano T, Emanuele B, Roberta C, Anna M, Beniamino P, Vittoria M, et al. Blood pressure levels at the time of percutaneous coronary revascularization and risk of coronary in-stent restenosis. Am J Hypertens. 2016;29:509–18.
Picone DS, Schultz MG, Otahal P, Aakhus S, Al-Jumaily AM, Black JA, et al. Accuracy of cuff- measured blood pressure: systematic reviews and meta-analyses. J Am Coll Cardiol. 2017;70:572–86.
Kobayashi H, Kinou M, Takazawa K. Correlation between the brachial blood pressure values obtained using the cuff method and the central blood pressure values obtained invasively. Intern Med. 2013;52:1675–80.
Thiebaud RS, Fahs CA, Rossow LM, Loenneke JP, Kim D, Mouser JG, et al. Effects of age on arterial stiffness and central blood pressure after an acute bout of resistance exercise. Eur J Appl Physiol. 2016;116:39–48.
Liu B, Li Q, Qiu P. Comparison between invasive and non-invasive blood pressure in young, middle and old age. Blood Press. 2016;25:155–61.
Picone DS, Schultz MG, Otahal P, Black JA, Bos WJ, Chen CH, et al. Influence of age on upper arm cuff blood pressure measurement. Hypertension. 2020;75:844–50.
Manninger M, Zweiker D, van Hunnik A, Alogna A, Prassl AJ, Schipke J, et al. Arterial hypertension drives arrhythmia progression via specific structural remodeling in a porcine model of atrial fibrillation. Heart Rhythm. 2018;15:1328–36.
Feenstra RK, Allaart CP, Berkelmans GFN, Westerhof BE, Smulders YM. Accuracy of oscillometric blood pressure measurement in atrial fibrillation. Blood Press Monit. 2018;23:59–63.
Pagonas N, Schmidt S, Eysel J, Compton F, Hoffmann C, Seibert F, et al. Impact of atrial fibrillation on the accuracy of oscillometric blood pressure monitoring. Hypertension. 2013;62:579–84.
Stergiou GS, Kollias A, Destounis A, Tzamouranis D. Automated blood pressure measurement in atrial fibrillation:a systematic review and meta-analysis. J Hypertens. 2012;30:2074–82.
Xie F, Xu J, Xia L-L, Jiang Z, Wu Y, Su H, et al. The impact of atrial fibrillation on accuracy of oscillometric blood pressure measurement: effect of ventricular rate. Hypertens Res. 2020;43:518–24.
Writing Group of 2018 Chinese Guidelines for the Management of Hypertension, Chinese Hypertension League, Chinese Society of Cardiology, Chinese Medical Doctor Association Hypertension Committee, Hypertension Branch of China International Exchange and Promotive Association for Medical and Health Care, Hypertension Branch of Chinese Geriatric Medical Association.Guidelines for the prevention and treatment of hypertension in China (2018 revision). Chin J Cardiovasc Med. 2019;24:24–56.
Dart RA, Alpert B, Quinn D. Effect of mechanical behavior of the brachial artery on blood pressure measurement during cuff inflation and cuff deflation. Blood Press Monit. 2014;19:120.
Luo X, Xiong Q, Xu J, Hong K, Peng Q, Hai S, et al. Differences in heart rate response and recovery after 6-minute walking test between patients with atrial fibrillation and in sinus rhythm. Am J Cardiol. 2018;122:592–6.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Himmelfarb CD, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71:e13–115.
Park JS, Shin JH, Park JB, Choi DJ, Youn HJ, Park CG, et al. Relationship between arterial stiffness and circadian pattern of blood pressure. Medicine. 2019;98:e14953.
Picone DS, Schultz MG, Peng X, Black JA, Dwyer N, Sharman JE, et al. Discovery of new blood pressure phenotypes and relation to accuracy of cuff devices used in daily clinical practice. Hypertension. 2018;71:1239–47.
Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA. Coupled systolic- ventricular and vascular stiffening with age: implications for pressure regulation and cardiac reserve in the elderly. J Am Coll Cardiol. 1998;32:1221–7.
Wang X-X, Shuai W, Hong K, Xu J, Cheng X-S, Su H, et al. How to evaluate BP measurements using the oscillometric method in atrial fibrillation: the value of pulse rate variation. Hypertens Res. 2016;39:588–92.
Stergiou GS, Kyriakoulis KG, Stambolliu E, Destounis A, Karpettas N, Kalogeropoulos P, et al. Blood pressure measurement in atrial fibrillation: review and meta-analysis of evidence on accuracy and clinical relevance. J Hypertens. 2019;37:2430–41.
Clark CE, McDonagh STJ, McManus RJ. Accuracy of automated blood pressure measurements in the presence of atrial fibrillation: systematic review and meta-analysis. J Hum Hypertens. 2019;33:352–64.
Acknowledgements
The authors appreciate all the participants and their relatives in the study and the members of the survey teams in the Second Affiliated Hospital of Nanchang University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Unfortunately, an error occurred in the author affiliations.
Rights and permissions
About this article
Cite this article
Xie, F., Xu, J., Liu, H. et al. Different impact factors for accurate oscillometric blood pressure measurement between sinus rhythm and atrial fibrillation. J Hum Hypertens 35, 785–790 (2021). https://doi.org/10.1038/s41371-021-00512-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00512-9
This article is cited by
-
Accuracy of oscillometric-based blood pressure monitoring devices: impact of pulse volume, arrhythmia, and respiratory artifact
Journal of Human Hypertension (2023)
-
Blood pressure in atrial fibrillation and in sinus rhythm during ambulatory blood pressure monitoring: data from the TEMPLAR project
Hypertension Research (2023)
-
Early vascular ageing phenotypes and urinary targeted metabolomics in children and young adults: the ExAMIN Youth SA and African-PREDICT studies
Amino Acids (2023)
-
24-hour ambulatory blood pressure telemonitoring in patients at risk of atrial fibrillation: results from the TEMPLAR project
Hypertension Research (2022)