Abstract
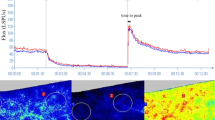
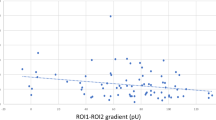
Primary aldosteronism (PA) is associated with considerably higher cardiovascular risk and increased prevalence of organ damage compared to essential hypertension (EH). Laser speckle contrast imaging (LSCI) has emerged as a novel non-invasive tool to assess of skin microcirculation. Our aim was to evaluate skin microvascular function (SMF) using LSCI coupled with post-occlusive reactive hyperemia (PORH) in a group of PA patients (PAs) compared to patients with EH (EHs) and normotensive controls (NTs). We enrolled PAs, age- and gender-matched with EHs and NTs. All participants underwent SMF assessment by LSCI with PORH. We enrolled 109 participants including 29 PAs, 47 EHs, and 33 NTs. SMF was significantly impaired in PAs, including peak time (p < 0.001) and base to peak flux (p < 0.001) compared to NTs and EHs. Among PAs, plasma aldosterone showed a positive correlation with occlusion flux (p = 0.005). Our study shows for the first time that PAs present impaired SMF as assessed with LSCI coupled with PORH, not only compared to NTs but also compared to EHs with similar blood pressure profile. Further studies are needed to investigate the clinical impact of such alterations in terms of pathophysiology and cardiovascular risk prediction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006;48:2293–300.
Hannemann A, Bidlingmaier M, Friedrich N, Manolopoulou J, Spyroglou A, Völzke H, et al. Screening for primary aldosteronism in hypertensive subjects: results from two German epidemiological studies. Eur J Endocrinol. 2012;167:7–15.
Ohno Y, Sone M, Inagaki N, Yamasaki T, Ogawa O, Takeda Y, et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism a multicenter study in Japan. Hypertension. 2018;71:530–7.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
Hung CS, Sung SH, Liao CW, Pan CT, Chang CC, Chen ZW, et al. Aldosterone induces vascular damage: A wave reflection analysis study. Hypertension 2019;74:623–9.
Gkaliagkousi E, Anyfanti P, Triantafyllou A, Gavriilaki E, Nikolaidou B, Lazaridis A, et al. Aldosterone as a mediator of microvascular and macrovascular damage in a population of normotensive to early-stage hypertensive individuals. J Am Soc Hypertens. 2018;12:50–7.
Chen ZW, Tsai CH, Pan CT, Chou CH, Liao CW, Hung CS, et al. Endothelial dysfunction in primary aldosteronism. Int J Mol Sci. 2019;20:1–25.
Rizzoni D, Paiardi S, Rodella L, Porteri E, De Ciuceis C, Rezzani R, et al. Changes in extracellular matrix in subcutaneous small resistance arteries of patients with primary aldosteronism. J Clin Endocrinol Metab. 2006;91:2638–42.
Rossi GP, Bolognesi M, Rizzoni D, Seccia TM, Piva A, Porteri E, et al. Vascular remodeling and duration of hypertension predict outcome of adrenalectomy in primary aldosteronism patients. Hypertension. 2008;51:1366–71.
Taddei S, Virdis A, Mattei P, Salvetti A. Vasodilation to acetylcholine in primary and secondary forms of human hypertension. Hypertension. 1993;21:929–33.
Holowatz LA, Thompson-torgerson CS, Kenney WL. The human cutaneous circulation as a model of generalized microvascular function. J Appl Physio. 2008;105:370–2.
Coulon P, Constans J, Gosse P. Impairment of skin blood flow during post-occlusive reactive hyperhemy assessed by laser Doppler flowmetry correlates with renal resistive index. J Hum Hypertens. 2012;26:56–63.
IJzerman RG, de Jongh RT, Beijk MAM, van Weissenbruch MM, Delemarre-van de Waal HA, Serné EH, et al. Individuals at increased coronary heart disease risk are characterized by an impaired microvascular function in skin. Eur J Clin Invest. 2003;33:536–42.
Mahé G, Humeau-Heurtier A, Durand S, Leftheriotis G, Abraham P. Assessment of skin microvascular function and dysfunction with laser speckle contrast imaging. Circ Cardiovasc Imaging. 2012;5:155–63.
Humeau-heurtier A, Abraham P, Durand S, Mah G. Excellent inter- and intra-observer reproducibility of microvascular tests using laser speckle contrast imaging. Clin Hemorheol Microcirc. 2014;58:439–46.
Concistrè A, Petramala L, Bonvicini M, Gigante A, Collalti G, Pellicano C, et al. Comparisons of skin microvascular changes in patients with primary aldosteronism and essential hypertension. Hypertens Res. 2020;43:1222–30.
Kishimoto S, Matsumoto T, Oki K, Maruhashi T, Kajikawa M, Matsui S, et al. Microvascular endothelial function is impaired in patients with idiopathic hyperaldosteronism. Hypertens Res. 2018;41:932–8.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2016;101:1889–916.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. J Hypertens. 2018;36:1953–2041.
Roustit M, Cracowski J. Assessment of endothelial and neurovascular function in human skin microcirculation. Trends Pharm Sci. 2013;34:373–84.
Boas DA, Dunn AK. Laser speckle contrast imaging in biomedical optics. J Biomed Opt 2010;15:011109.
Rousseau P, Mahé G, Haj-yassin F, Durand S, Humeau A, Leftheriotis G, et al. Increasing the “ region of interest” and “ time of interest”, both reduce the variability of blood fl ow measurements using laser speckle contrast imaging. Microvasc Res. 2011;82:88–91.
Dipla K, Triantafyllou A, Koletsos N, Papadopoulos S, Sachpekidis V, Vrabas IS, et al. Impaired muscle oxygenation and elevated exercise blood pressure in hypertensive patients: links with vascular stiffness. Hypertension. 2017;70:444–51.
Lazaridis A, Gkaliagkousi E, Koletsos N, Nikolaidou B, Anyfanti P, Dolgyras P, et al. Real time assessment of microcirculation in hypertension using laser speckle contrast analysis. J Hypertens. 2018;36:283–4.
Triantafyllou A, Anyfanti P, Zabulis X, Gavriilaki E, Karamaounas P, Gkaliagkousi E, et al. Accumulation of microvascular target organ damage in newly diagnosed hypertensive patients. J Am Soc Hypertens. 2014;8:542–9.
Savard S, Amar L, Plouin PF, Steichen O. Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension. 2013;62:331–6.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol 2005;45:1243–8.
Stehr CB, Mellado R, Ocaranza MP, Carvajal CA, Mosso L, Becerra E, et al. Increased levels of oxidative stress, subclinical inflammation, and myocardial fibrosis markers in primary aldosteronism patients. J Hypertens. 2010;28:2120–6.
Zhu CJ, Wang QQ, Zhou JL, Liu HZ, Hua F, Yang HZ, et al. The mineralocorticoid receptor-p38MAPK-NFB or ERK-Sp1 signal pathways mediate aldosterone-stimulated inflammatory and profibrotic responses in rat vascular smooth muscle cells. Acta Pharm Sin. 2012;33:873–8.
Koletsos N, Gkaliagkousi E, Lazaridis A, Triantafyllou A, Anyfanti P, Dolgyras P, et al. Skin microvascular dysfunction in systemic lupus erythematosus patients with and without cardiovascular risk factors. Rheumatol (Oxf). 2021;60:2834–41. 18
Cracowski JL, Gaillard-Bigot F, Cracowski C, Sors C, Roustit M, Millet C. Involvement of cytochrome epoxygenase metabolites in cutaneous postocclusive hyperemia in humans. J Appl Physiol. 2013;114:245–51.
Koeppen M, Feil R, Siegl D, Feil S, Hofmann F, Pohl U, et al. cGMP-dependent protein kinase mediates NO-but not acetylcholine-induced dilations in resistance vessels in vivo. Hypertension. 2004;44:952–5.
Grgic I, Kaistha BP, Hoyer J, Köhler R. Endothelial Ca 2+-activated K + channels in normal and impaired EDHF-dilator responses - relevance to cardiovascular pathologies and drug discovery. Br J Pharmacol. 2009;157:509–26.
Dupont JJ, Hill MA, Bender SB, Jaisser F, Jaffe IZ. Aldosterone and vascular mineralocorticoid receptors: regulators of ion channels beyond the kidney. Hypertension. 2014;63:632–7.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gkaliagkousi, E., Lazaridis, A., Anyfanti, P. et al. Assessment of skin microcirculation in primary aldosteronism: impaired microvascular responses compared to essential hypertensives and normotensives. J Hum Hypertens 36, 1066–1071 (2022). https://doi.org/10.1038/s41371-021-00639-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00639-9