Abstract
Objectives
The objective of this study is to describe clinical and ultrasound changes in a cohort of premature newborns with post-hemorrhagic ventricular dilation (PHVD), and to correlate these changes with outcome.
Study Design
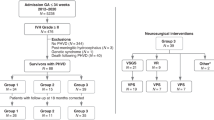
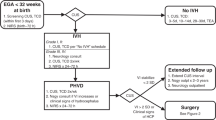
Premature newborns <29 weeks gestational age (GA) and ≤ 1,500 g birth weight with intraventricular hemorrhage were retrospectively reviewed. Clinical signs and cranial ultrasound (CUS) findings between time after birth and time before first cerebrospinal fluid temporizing intervention were compared with GA-equivalent newborns without interventions. White matter injury was assessed on brain magnetic resonance imaging.
Results
Between 2011 and 2014, 64 newborns met inclusion criteria; 23% had PHVD. The growth rates of the ventricles on CUS and the head circumference (HC) were higher in newborns with PHVD (p < 0.01 and p = 0.04, respectively) and correlated inversely with white matter injury (p = 0.006 and p < 0.001, respectively).
Conclusion
Progression of PHVD in premature newborns as demonstrated by CUS and the HC correlated with outcome. Consistent measurement of these simple parameters will allow for much needed treatment comparisons, to define optimal protocols that decrease the risk of cerebral palsy in extremely preterm populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Winter S, Autry A, Boyle C, Yeargin-Allsopp M. Trends in the prevalence of cerebral palsy in a population-based study. Pediatrics. 2002;110(6):1220–5.
Pakula AT, Van Naarden Braun K, Yeargin-Allsopp M. Cerebral palsy: classification and epidemiology. Phys Med Rehabil Clin N Am. 2009;20(3):425–52.
Dyet LE, Kennea N, Counsell SJ, Maalouf EF, Ajayi-Obe M, Duggan PJ, et al. Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics. 2006;118(2):536–48.
Fletcher JM, Landry SH, Bohan TP, Davidson KC, Brookshire BL, Lachar D, et al. Effects of intraventricular hemorrhage and hydrocephalus on the long-term neurobehavioral development of preterm very-low-birthweight infants. Dev Med Child Neurol. 1997;39(9):596–606.
Brouwer A, Groenendaal F, van Haastert IL, Rademaker K, Hanlo P, de Vries L. Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr. 2008;152(5):648–54.
Shankaran S, Koepke T, Woldt E, Bedard MP, Dajani R, Eisenbrey AB, et al. Outcome after posthemorrhagic ventriculomegaly in comparison with mild hemorrhage without ventriculomegaly. J Pediatr. 1989;114(1):109–14.
Klebermass-Schrehof K, Rona Z, Waldhor T, Czaba C, Beke A, Weninger M, et al. Can neurophysiological assessment improve timing of intervention in posthaemorrhagic ventricular dilatation? Arch Dis Child Fetal Neonatal Ed. 2013;98(4):2012–302323.
Olischar M, Klebermass K, Hengl B, Hunt RW, Waldhoer T, Pollak A, et al. Cerebrospinal fluid drainage in posthaemorrhagic ventricular dilatation leads to improvement in amplitude-integrated electroencephalographic activity. Acta Paediatr. 2009;98(6):1002–9.
Riva-Cambrin J, Shannon CN, Holubkov R, Whitehead WE, Kulkarni AV, Drake J, et al. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J Neurosurg Pediatr. 2012;9(5):473–81.
Brouwer MJ, de Vries LS, Groenendaal F, Koopman C, Pistorius LR, Mulder EJ, et al. New reference values for the neonatal cerebral ventricles. Radiology. 2012;262(1):224–33.
Davies MW, Swaminathan M, Chuang SL, Betheras FR. Reference ranges for the linear dimensions of the intracranial ventricles in preterm neonates. Arch Dis Child Fetal Neonatal Ed. 2000;82(3):F218–23.
Levene MI. Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child. 1981;56(12):900–4.
Zamora C, Tekes A, Alqahtani E, Kalayci OT, Northington F, Huisman TA. Variability of resistive indices in the anterior cerebral artery during fontanel compression in preterm and term neonates measured by transcranial duplex sonography. J Perinatol. 2014;34(4):306–10.
Hill A, Volpe JJ. Decrease in pulsatile flow in the anterior cerebral arteries in infantile hydrocephalus. Pediatrics. 1982;69(1):4–7.
Papile LA, Burstein J, Burstein R, Koffler H, Koops BL, Johnson JD. Posthemorrhagic hydrocephalus in low-birth-weight infants: treatment by serial lumbar punctures. J Pediatr. 1980;97(2):273–7.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Ment LR, Bada HS, Barnes P, Grant PE, Hirtz D, Papile LA, et al. Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2002;58(12):1726–38.
Inder TE, Wells SJ, Mogridge NB, Spencer C, Volpe JJ. Defining the nature of the cerebral abnormalities in the premature infant: a qualitative magnetic resonance imaging study. J Pediatr. 2003;143(2):171–9.
Palisano RJ, Copeland WP, Galuppi BE. Performance of physical activities by adolescents with cerebral palsy. Phys Ther. 2007;87(1):77–87.
Fenton TR. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003;3:13.
Limbrick DD Jr., Mathur A, Johnston JM, Munro R, Sagar J, Inder T, et al. Neurosurgical treatment of progressive posthemorrhagic ventricular dilation in preterm infants: a 10-year single-institution study. J Neurosurg Pediatr. 2010;6(3):224–30.
Bassan H, Eshel R, Golan I, Kohelet D, Ben Sira L, Mandel D, et al. Timing of external ventricular drainage and neurodevelopmental outcome in preterm infants with posthemorrhagic hydrocephalus. Eur J Paediatr Neurol. 2012;16(6):662–70.
Willis B, Javalkar V, Vannemreddy P, Caldito G, Matsuyama J, Guthikonda B, et al. Ventricular reservoirs and ventriculoperitoneal shunts for premature infants with posthemorrhagic hydrocephalus: an institutional experience. J Neurosurg Pediatr. 2009;3(2):94–100.
Ellenbogen JR, Waqar M, Pettorini B. Management of post-haemorrhagic hydrocephalus in premature infants. J Clin Neurosci. 2016;31:30–4.
Del Bigio MR, Kanfer JN, Zhang YW. Myelination delay in the cerebral white matter of immature rats with kaolin-induced hydrocephalus is reversible. J Neuropathol Exp Neurol. 1997;56(9):1053–66.
Del Bigio MR, Wilson MJ, Enno T. Chronic hydrocephalus in rats and humans: white matter loss and behavior changes. Ann Neurol. 2003;53(3):337–46.
de Vries LS, Liem KD, van Dijk K, Smit BJ, Sie L, Rademaker KJ, et al. Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in The Netherlands. Acta Paediatr. 2002;91(2):212–7.
Srinivasakumar P, Limbrick D, Munro R, Mercer D, Rao R, Inder T, et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am J Perinatol. 2013;30(3):207–14.
Muller WD, Urlesberger B. Correlation of ventricular size and head circumference after severe intra-periventricular haemorrhage in preterm infants. Childs Nerv Syst. 1992;8(1):33–5.
Ingram MC, Huguenard AL, Miller BA, Chern JJ. Poor correlation between head circumference and cranial ultrasound findings in premature infants with intraventricular hemorrhage. J Neurosurg Pediatr. 2014;14(2):184–9.
Volpe JJ, Pasternak JF, Allan WC. Ventricular dilation preceding rapid head growth following neonatal intracranial hemorrhage. Am J Dis Child. 1977;131(11):1212–5.
Traylor KS, Daugherty R. Patent ductus arteriosus incidentally suspected on a routine intracranial ultrasound for prematurity; confirmed on echocardiogram. Del Med J. 2015;87(1):17–9.
Mazzola CA, Choudhri AF, Auguste KI, Limbrick DD Jr., Rogido M, Mitchell L, et al. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr. 2014;1:8–23.
Anwar M, Kadam S, Hiatt IM, Hegyi T. Serial lumbar punctures in prevention of post-hemorrhagic hydrocephalus in preterm infants. J Pediatr. 1985;107(3):446–50.
Tian AG, Hintz SR, Cohen RS, Edwards MS. Ventricular access devices are safe and effective in the treatment of posthemorrhagic ventricular dilatation prior to shunt placement. Pediatr Neurosurg. 2012;48(1):13–20.
Wellons JC 3rd, Shannon CN, Holubkov R, Riva-Cambrin J, Kulkarni AV, Limbrick DD Jr., et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J Neurosurg Pediatr. 2017;20(1):19–29.
Nagy A, Bognar L, Pataki I, Barta Z, Novak L. Ventriculosubgaleal shunt in the treatment of posthemorrhagic and postinfectious hydrocephalus of premature infants. Childs Nerv Syst. 2013;29(3):413–8.
Funding
This work was supported by a grant from the Board of Visitors of Children’s National for the establishment of a Cerebral Palsy Prevention Program.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosures: The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Obeid, R., Chang, T., Bluth, E. et al. The use of clinical examination and cranial ultrasound in the diagnosis and management of post-hemorrhagic ventricular dilation in extremely premature infants. J Perinatol 38, 374–380 (2018). https://doi.org/10.1038/s41372-017-0017-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-017-0017-3
This article is cited by
-
Epidemiology of post-hemorrhagic ventricular dilatation in very preterm infants
Journal of Perinatology (2022)