Abstract
Objective
To characterize the impact of premedication with and without a paralytic agent on the safety of tracheal intubation (TI) in infants ≤1500 g.
Study design
A prospective observational cohort study between February 2015 and June 2017. The primary outcomes were associations between the use of different premedication regimens with number of TI attempts, TI adverse events (TIAEs), and changes in heart rate.
Results
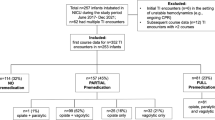
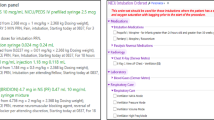
Data were collected on 237 TIs. Median postmenstrual age at intubation was 28 completed weeks and weight was 953 g. Premedication with a paralytic was associated with fewer intubation attempts compared to premedication without a paralytic (p = 0.037). Premedication with a paralytic was associated with fewer TIAEs (p < 0.001) and less bradycardia compared to the other two regimens (p = 0.003) compared to premedication without a paralytic.
Conclusions
Premedication with a paralytic was associated with fewer intubation attempts, fewer TIAEs, and less bradycardia. Premedication with a paralytic may improve intubation safety in VLBWs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Sawyer T, French H, Ades A, Johnston L. Neonatal-perinatal medicine fellow procedural experience and competency determination: results of a national survey. J Perinatol. 2016;36:570–4.
Haubner LY, Barry JS, Johnston LC, Soghier L, Tatum PM, Kessler D, et al. Neonatal intubation performance: room for improvement in tertiary neonatal intensive care units. Resuscitation. 2013;84:1359–64.
Hatch LD, Grubb PH, Lea AS, Walsh WF, Markham MH, Whitney GM, et al. Endotracheal intubation in neonates: a prospective study of adverse safety events in 162 infants. J Pediatr. 2016;168:62–66.e66
Sauer CW, Kong JY, Vaucher YE, Finer N, Proudfoot JA, Boutin MA, et al. Intubation Attempts increase the risk for severe intraventricular hemorrhage in preterm infants—a retrospective cohort study. J Pediatr. 2016;177:108–13.
Wallenstein MB, Birnie KL, Arain YH, Yang W, Yamada NK, Huffman LC, et al. Failed endotracheal intubation and adverse outcomes among extremely low birth weight infants. J Perinatol. 2016;36:112–5.
Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–29.
Sawyer T, Foglia E, Hatch LD, Moussa A, Ades A, Johnston L, et al. Improving neonatal intubation safety: a journey of a thousand miles. J Neonatal Perinat Med. 2017;10:125–31.
Roberts KD, Leone TA, Edwards WH, Rich WD, Finer NN. Premedication for non-emergent neonatal intubations: a randomized, controlled trial comparing atropine and fentanyl to atropine, fentanyl, and mivacurium. Pediatrics. 2006;118:1583–91.
Lemyre B, Cheng R, Gaboury I. Atropine, fentanyl and succinylcholine for non-urgent intubations in newborns. Arch Dis Child Fetal Neonatal Ed. 2009;94:F439–442.
Dempsey EM, Al Hazzani F, Faucher D, Barrington KJ. Facilitation of neonatal endotracheal intubation with mivacurium and fentanyl in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2006;91:F279–282.
Pereira e Silva Y, Gomez RS, Marcatto JeO, Maximo TA, Barbosa RF, Simões e Silva AC. Morphine versus remifentanil for intubating preterm neonates. Arch Dis Child Fetal Neonatal Ed. 2007;92:F293–294.
Ghanta S, Abdel-Latif ME, Lui K, Ravindranathan H, Awad J, Oei J. Propofol compared with the morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics. 2007;119:e1248–1255.
Carbajal R, Eble B, Anand KJ. Premedication for tracheal intubation in neonates: confusion or controversy? Semin Perinatol. 2007;31:309–17.
Le CN, Garey DM, Leone TA, Goodmar JK, Rich W, Finer NN. Impact of premedication on neonatal intubations by pediatric and neonatal trainees. J Perinatol. 2014;34:458–60.
Kumar P, Denson SE, Mancuso TJ, Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125:608–15.
Muniraman HK, Yaari J, Hand I. Premedication use before non-emergent intubation in the newborn infant. Am J Perinatol. 2015;32:821–4.
Duncan HP, Zurick NJ, Wolf AR. Should we reconsider awake neonatal intubation? A review of the evidence and treatment strategies. Paediatr Anaesth. 2001;11:135–45.
Barrington KJ, Finer NN, Etches PC. Succinylcholine and atropine for premedication of the newborn infant before nasotracheal intubation: a randomized, controlled trial. Crit Care Med. 1989;17:1293–6.
Cook-Sather SD, Tulloch HV, Cnaan A, Nicolson SC, Cubina ML, Gallagher PR, et al. A comparison of awake versus paralyzed tracheal intubation for infants with pyloric stenosis. Anesth Analg. 1998;86:945–51.
Barrington KJ, Byrne PJ. Premedication for neonatal intubation. Am J Perinatol. 1998;15:213–6.
Oei J, Hari R, Butha T, Lui K. Facilitation of neonatal nasotracheal intubation with premedication: a randomized controlled trial. J Paediatr Child Health. 2002;38:146–50.
Raju TN, Vidyasagar D, Torres C, Grundy D, Bennett EJ. Intracranial pressure during intubation and anesthesia in infants. J Pediatr. 1980;96:860–2.
Friesen RH, Honda AT, Thieme RE. Changes in anterior fontanel pressure in preterm neonates during tracheal intubation. Anesth Analg. 1987;66:874–8.
Marshall TA, Deeder R, Pai S, Berkowitz GP, Austin TL. Physiologic changes associated with endotracheal intubation in preterm infants. Crit Care Med. 1984;12:501–3.
Kelly MA, Finer NN. Nasotracheal intubation in the neonate: physiologic responses and effects of atropine and pancuronium. J Pediatr. 1984;105:303–9.
Cordero L, Hon EH. Neonatal bradycardia following nasopharyngeal stimulation. J Pediatr. 1971;78:441–7.
Brady JP, Tooley WH. Cardiovascular and respiratory reflexes in the newborn. Pediatr Clin North Am. 1966;13:801–21.
Bowman WC. Non-relaxant properties of neuromuscular blocking drugs. Br J Anaesth. 1982;54:147–60.
Acknowledgements
We would like to thank the neonatal fellows, attendings, nurse practitioners, hospitalists, and physician assistants in the NICUs at the University of Washington Medical Center and Seattle Children’s Hospital for their diligent completion of NEAR4NEOS data collection forms. We would also like to thank Hayley Buffman, Natalie Napolitano, and Akira Nishisaki at Children’s Hospital of Philadelphia for their work with the NEAR4NEOs database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Rights and permissions
About this article
Cite this article
Krick, J., Gray, M., Umoren, R. et al. Premedication with paralysis improves intubation success and decreases adverse events in very low birth weight infants: a prospective cohort study. J Perinatol 38, 681–686 (2018). https://doi.org/10.1038/s41372-018-0082-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0082-2
This article is cited by
-
Association of full premedication on tracheal intubation outcomes in the neonatal intensive care unit: an observational cohort study
Journal of Perinatology (2023)
-
Standardizing premedication for non-emergent neonatal tracheal intubations improves compliance and patient outcomes
Journal of Perinatology (2022)
-
Premedication with neuromuscular blockade and sedation during neonatal intubation is associated with fewer adverse events
Journal of Perinatology (2019)