Abstract
Objective
Prompted by an acute increase in necrotizing enterocolitis (NEC) rates, we aimed to decrease the rate of stage 2 or greater NEC in infants born at <1500 grams or <30 weeks gestational age from 19.5% to less than 9.7% (a 50% reduction) within 18 months, without adversely affecting central line-associated bloodstream infection (CLABSI) rates.
Study design
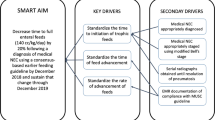
We utilized Define, Measure, Analyze, Improve, and Control (DMAIC) as our improvement model. Informed by our key driver diagram and root cause analyses, six Plan-Do-Study-Act cycles were completed.
Results
147 infants in the QI initiative had a median gestational age of 28.1 weeks and a median birthweight of 1070 grams. NEC rates decreased from the QI baseline of 19.5% to 6% (p = 0.03). Oral care administration increased, and maximal gavage tube dwell time decreased.
Conclusion
NEC rates decreased during this QI initiative through a combination of multidisciplinary interventions aimed at reducing dysbiosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sharma R, Hudak ML. A clinical perspective of necrotizing enterocolitis: past, present, and future. Clin Perinatol. 2013;40:27–51.
Neu J. Necrotizing enterocolitis. Pediatr Clin North Am. 1996;43:409–32.
Mowitz ME, Dukhovny D, Zupancic JAF. The cost of necrotizing enterocolitis in premature infants. Semin Fetal Neonatal Med. 2018;23:416–9.
Bazacliu C, Neu J. Necrotizing enterocolitis: long term complications. Curr Pediatr Rev. 2019;15:115–24.
Rose AT, Patel RM. A critical analysis of risk factors for necrotizing enterocolitis. Semin Fetal Neonatal Med. 2018;23:374–9.
Cacho NT, Parker LA, Neu J. Necrotizing enterocolitis and human milk feeding. Clin Perinatol. 2017;44:49–67.
Xiong T, Maheshwari A, Neu J, Ei-Saie A, Pammi M. An overview of systematic reviews of randomized-controlled trials for preventing necrotizing enterocolitis in preterm infants. Neonatology. 2020;117:46–56.
Denning NL, Prince JM. Neonatal intestinal dysbiosis in necrotizing enterocolitis. Mol Med. 2018;24:4.
Pammi M, Cope J, Tarr PI, Warner BB, Morrow AL, Mai V, et al. Intestinal dysbiosis in preterm infants preceding necrotizing enterocolitis: a systematic review and meta-analysis. Microbiome. 2017;5:31.
Bazacliu C, Neu J. Pathophysiology of necrotizing enterocolitis: an update. Curr Pediatr Rev. 2019;15:68–87.
Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 1990;336:1519–23.
Sullivan S, Schanler RJ, Kim JH, Patel AL, Trawöger R, Kiechl-Kohlendorfer U, et al. An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatrics. 2010;156:562–7.
Morgan RL, Preidis GA, Kashyap PC, Weizman AV, Sadeghirad B. Probiotics reduce mortality and morbidity in preterm, low-birth-weight infants: a systematic review and network meta-analysis of randomized trials. Gastroenterology. 2020;159:467–80.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sánchez PJ, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66.
Greenwood C, Morrow AL, Lagomarcino AJ, Altaye M, Taft DH, Yu Z, et al. Early empiric antibiotic use in preterm infants is associated with lower bacterial diversity and higher relative abundance of Enterobacter. J Pediatr. 2014;165:23–29.
Romaine A, Ye D, Ao Z, Fang F, Johnson O, Blake T, et al. Safety of histamine-2 receptor blockers in hospitalized VLBW infants. Early Hum Dev. 2016;99:27–30.
Ma A, Yang J, Li Y, Zhang X, Kang Y. Oropharyngeal colostrum therapy reduces the incidence of ventilator-associated pneumonia in very low birth weight infants: a systematic review and meta-analysis. Pediatr Res. 2021;89:54–62.
Garofalo NA, Caplan MS. Oropharyngeal mother’s milk: state of the science and influence on necrotizing enterocolitis. Clin Perinatol. 2019;46:77–88.
Patel AL, Trivedi S, Bhandari NP, Ruf A, Scala CM, Witowitch G, et al. Reducing necrotizing enterocolitis in very low birth weight infants using quality-improvement methods. J Perinatol. 2014;34:850–7.
Yee WH, Soraisham AS, Shah VS, Aziz K, Yoon W, Lee SK. Incidence and timing of presentation of necrotizing enterocolitis in preterm infants. Pediatrics. 2012;129:e298–e304.
Battersby C, Santhalingam T, Costeloe K, Modi N. Incidence of neonatal necrotising enterocolitis in high-income countries: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2018;103:F182–9.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33:179–201.
Moreno-Fernandez J, Sánchez-Martínez B, Serrano-López L, Martín-Álvarez E, Diaz-Castro J, Peña-Caballero M, et al. Enhancement of immune response mediated by oropharyngeal colostrum administration in preterm neonates. Pediatr Allergy Immunol. 2019;30:234–41.
Quigley M, Embleton ND, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2019;7:1465–858.
American Society for Quality. The Define, Measure, Analyze, Improve, Control (DMAIC) Process. [Accessed June 20, 2022]. Available from: https://asq.org/quality-resources/dmaic
Pyzdek T, Keller PA. The Six Sigma Handbook: A Complete Guide for Green Belts, Black Belts, and Managers at All Levels, Third edn. McGraw Hill: New York, NY, 2010.
Michie S, Van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
NeoMed. NeoConnect Feeding Tubes for ENFit Instructions for Use. 2018. [Accessed June 11, 2020]. Available from: https://www.neomedinc.com/wp-content/uploads/2019/06/NeoConnect-Feeding-Tubes-for-ENFit-Instructions-for-Use.pdf
Patel AL, Meier PP, Canvasser J. Strategies to increase the use of mother’s own milk for infants at risk of necrotizing enterocolitis. Pediatr Res. 2020;88:21–24.
Meier PP, Johnson TJ, Patel AL, Rossman B. Evidence-based methods that promote human milk feeding of preterm infants. Clin Perinatol. 2017;44:1–22.
Miracle DJ, Meier PP, Bennett PA. Mothers’ decisions to change from formula to mothers’ milk for very-low-birth-weight infants. J Obstet Gynecol Neonatal Nurs. 2004;33:692–703.
Meier PP, Engstrom JL, Patel AL, Jegier BJ, Bruns NE. Improving the use of human milk during and after the NICU stay. Clin Perinatol. 2010;37:217–45.
Committee on nutrition, Section on breastfeeding, Committee on fetus and newborn, Daniels S, Corkins M, de Ferranti S, et al. Donor Human Milk for the High-Risk Infant: Preparation, Safety, and Usage Options in the United States. Pediatrics. 2017;139:e20163440.
Montgomery DC. Introduction to Statistical Quality Control. John Wiley & Sons, Inc., 2013.
Hurrell E, Kucerova E, Loughlin M, Caubilla-Barron J, Hilton A, Armstrong R, et al. Neonatal enteral feeding tubes as loci for colonisation by members of the Enterobacteriaceae. BMC Infect Dis. 2009;9:146.
van den Akker CHP, van Goudoever JB, Shamir R, Domellöf M, Embleton ND, Hojsak I, et al. Probiotics and preterm infants: a position paper by the European society for paediatric gastroenterology hepatology and nutrition committee on nutrition and the European society for paediatric gastroenterology hepatology and nutrition working group for probiotics and prebiotics. J Pediatr Gastroenterol Nutr. 2020;70:664–80.
Bafeta A, Koh M, Riveros C, Raaud P. Harms reporting in randomized controlled trials of interventions aimed at modifying microbiota. Ann Intern Med. 2018;169:240–7.
Esaiassen E, Cavanagh P, Hjerde E, Simonsen GS, Støen R, Klingenberg C. Bifidobacterium longumSubspeciesinfantisBacteremia in 3 Extremely Preterm Infants Receiving Probiotics. Emerg Infect Dis. 2016;22:1664–6.
Vermeulen MJ, Luijendijk A, Toledo L, Kaam AH, Reiss IKM. Quality of probiotic products for preterm infants: Contamination and missing strains. Acta Paediatrica. 2020;109:276–9.
Poindexter B, Cummings J, Hand I, Adams-Chapman I, Aucott SW, Puopolo KM, et al. Use of probiotics in preterm infants. Pediatrics. 2021;147:e2021051485.
Kaplan HC, Provost LP, Froehle CM, Margolis PA. The Model for Understanding Success in Quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2012;21:13–20.
Larson CE, Larson C, LaFasto FMJ, Fasto FML. Teamwork: What Must Go Right/What Can Go Wrong. SAGE Publications, 1989.
Gray KD, Messina JA, Cortina C, Owens T, Fowler M, Foster M, et al. Probiotic use and safety in the neonatal intensive care unit: a matched cohort study. J Pediatr. 2020;222:59–64.e51.
Javidi D, Wang Z, Rajasekaran S, Hussain N. Temporal and seasonal variations in incidence of stage II and III NEC—a 28-year epidemiologic study from tertiary NICUs in Connecticut, USA. J Perinatol. 2021;41:1100–9.
Acknowledgements
The authors would like to thank Roxanne Torgerson, RN and Angela Giese, RN for their advocacy in promoting QI interventions in the NICU during this project.
Author information
Authors and Affiliations
Contributions
SCM: Conceptualization, methodology, formal analysis, investigation, data curation, visualization, writing- original draft. CMG: Conceptualization, methodology, investigation, writing- review & editing. MM, DLH, BNS, RCS: Methodology, writing- review & editing. MMM and LAS: Methodology, investigation, writing- review & editing. VSS: Project administration, writing- review & editing. JLF: Conceptualization, methodology, formal analysis, supervision, writing- review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mavis, S.C., Gallup, M.C., Meyer, M. et al. A quality improvement initiative to reduce necrotizing enterocolitis in high-risk neonates. J Perinatol 43, 97–102 (2023). https://doi.org/10.1038/s41372-022-01476-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01476-5