Abstract
Objective
To explore associations between epidural administration to mothers in labor with neurodevelopmental outcomes at 3 years corrected age in preterm infants born <29 weeks gestational age.
Study design
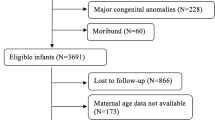
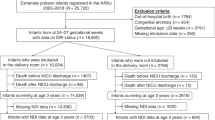
Infants born <29 weeks gestational age between 2006 and 2012 were included. Our primary outcome was a composite of death or neurodevelopmental impairment at 3 years corrected age. Infants were divided into those whose mothers did or did not receive epidural analgesia in labor. Univariable and multivariable regression was used for analysis.
Results
There were 548 infants in the no epidural analgesia group and 121 in the epidural analgesia group. The adjusted odds ratio (95%CI) of neurodevelopmental impairment or death in the epidural group was 1.25 (0.82–1.93). Propensity score-matched results were 1.32 (0.79–2.22).
Conclusion
Preterm infants born <29 weeks gestational age to mothers who received epidural analgesia during labor were not associated with poor neurodevelopmental outcomes at 3 years corrected age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
In accordance with the Alberta Health Services Data Disclosure Agreement, we are not able to provide or make the data available for any purpose to a third party without the prior written consent of Alberta Health Services, Calgary, Alberta. Custom generated R Studio code used for data analysis is available upon reasonable request to the authors.
References
Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N. United States state-level variation in the use of neuraxial analgesia during labor for pregnant women. JAMA Netw Open. 2018;1:e186567.
Seijmonsbergen-Schermers AE, van den Akker T, Rydahl E, Beeckman K, Bogaerts A, Binfa L, et al. Variations in use of childbirth interventions in 13 high-income countries: a multinational cross-sectional study. PLoS Med. 2020;17:e1003103.
Halliday L, Nelson SM, Kearns RJ. Epidural analgesia in labor: A narrative review. Int J Gynaecol Obstet. 2022;159:356–64.
Moola S. Chapter 4: Care during labour and birth. In: Public Health Agency of Canada. Family-Centred Maternity and Newborn Care: National Guidelines. Ottawa, ON, Canada: PHAC; 2018.
ACOG Practice Bulletin No. 209 Summary: Obstetric Analgesia and Anesthesia. Obstet Gynecol 2019; 133: 595-7.
Golub MS. Labor analgesia and infant brain development. Pharm Biochem Behav. 1996;55:619–28.
Qiu C, Lin JC, Shi JM, Chow T, Desai VN, Nguyen VT, et al. Association between epidural analgesia during labor and risk of autism spectrum disorders in offspring. JAMA Pediatr. 2020;174:1168–75.
Krol JW, Stanirowski PJ, Mazanowska N, Majewska A, Wielgos M, Bomba-Opon D. Is there an association between the use of epidural analgesia during labor and the development of autism spectrum disorder in the offspring?-A Review of the Literature. Int J Environ Res Public Health. 2022;19:7202.
Zhang L, Graham JH, Feng W, Lewis MW, Zhang X, Kirchner HL. No association of labor epidural analgesia with cerebral palsy in children. J Anesth. 2016;30:1008–13. https://doi.org/10.1007/s00540-016-2244-8.
Kearns RJ, Shaw M, Gromski PS, Iliodromiti S, Lawlor DA, Nelson SM. Association of epidural analgesia in women in labor with neonatal and childhood outcomes in a population cohort. JAMA Netw Open. 2021;4:e2131683.
Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Wilson-Costello D, et al. Poor predictive validity of the Bayley Scales of Infant development for cognitive function of extremely low birth weight children at school age. Pediatrics. 2005;116:333–41.
Marlow N, Wolke D, Bracewell MA, Samara M, Group EPS. Neurologic and developmental disability at six years of age after extremely preterm birth. N. Engl J Med. 2005;352:9–19.
Robertson CM, Watt MJ, Dinu IA. Outcomes for the extremely premature infant: what is new? And where are we going? Pediatr Neurol. 2009;40:189–96.
Schmidt B, Anderson PJ, Doyle LW, Dewey D, Grunau RE, Asztalos E, et al. Survival without disability to age 5 years after neonatal caffeine therapy for apnea of prematurity. JAMA. 2012;307:275–82.
Anim-Somuah M, Smyth R, Howell C. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev. 2005;19:CD000331.
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805–35.
Wechsler D. WPPSI-III. Wechsler preschool and primary scale of intelligence-third edition (WPPSI-III). The Psychological Corporation: San Antonio, TX, USA; 2002.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988;82:527–32.
International Committee for the Classification of Retinopathy of Prematurity. The international classification of retinopathy of prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92:529–34.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013;13:59.
Moser JJ, Archer DP, Walker AM, Rice TK, Dewey D, Lodha AK, et al. Association of sedation and anesthesia on cognitive outcomes in very premature infants: a retrospective observational study. Can J Anesth. 2023;70:56–68.
van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–94.
Buuren S V, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
Ho DE, Imai K, King G, Stuart EA. Nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42:1–28.
David H, Rosen M. Perinatal mortality after epidural analgesia. Anaesthesia. 1976;31:1054–9.
Jia L, Cao H, Guo Y, Shen Y, Zhang X, Feng Z, et al. Evaluation of epidural analgesia use during labor and infection in full-term neonates delivered vaginally. JAMA Netw Open. 2021;4:e2123757.
Mori Y, Toyama S, Sato M, Yamashita Y, Suzuki Y, Sago H. Influence of preterm labour epidural analgesia on neonatal and maternal outcomes: a single-centre retrospective study. Br J Anaesth. 2021;127:e154–6.
Sharma SK, Rogers BB, Alexander JM, McIntire DD, Leveno KJ. A randomized trial of the effects of antibiotic prophylaxis on epidural-related fever in labor. Anesth Analg. 2014;118:604–10.
Silverman MA, Konnikova L, Gerber JS. Impact of antibiotics on necrotizing enterocolitis and antibiotic-associated diarrhea. Gastroenterol Clin North Am. 2017;46:61–76.
Gelman A. Don’t calculate post-hoc power using observed estimates of effect size. Ann Surg. 2019;269:e9–e01.
Gelman A. Comment on “Post-hoc power using observed estimate of effect size is too noisy to be useful. Ann Surg. 2019;270:e64.
Althouse AD. Post hoc power: not empowering, just misleading. J Surg Res. 2021;259:A3–6.
Heckman MG, Davis JM III, Crowson CS. Post hoc power calculation: an inappropriate method for interpreting the findings of a research study. J Rheumatol. 2022;49:867–70.
Funding
Findings were presented in part at the 46th American Academy of Pediatrics, Section of Neonatal-Perinatal Medicine, District 8 Conference, San Diego, California, June 1–4, 2023.
Author information
Authors and Affiliations
Contributions
Mr. Arijit Lodha drafted the initial version of the manuscript and was involved in the critical review and revision of the manuscript. Dr. J J Moser, Dr. A Lodha and Dr. D McAllister conceptualized and designed the study and were involved in the acquisition and interpretation of the data and the critical review and revision of the manuscript. Dr. Walker was involved in data acquisition, statistical analysis and interpretation of the data and the critical review and revision of the manuscript.Ms. Selphee Tang was involved in the acquisition and interpretation of the data and critical review and revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lodha, A., Moser, J.J., Walker, A. et al. Association of epidural analgesia in labor with neurodevelopmental outcomes in premature infants born at <29 weeks of gestational age. J Perinatol 44, 548–553 (2024). https://doi.org/10.1038/s41372-024-01893-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-024-01893-8