Abstract
Objective
Identify feeding supports required among infants with neonatal encephalopathy and determine growth trajectories to 3 years.
Study design
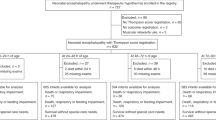
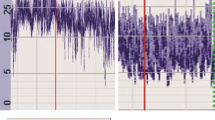
Single-center retrospective cohort study of 120 infants undergoing therapeutic hypothermia. Logistic regression and stratified analyses identified whether clinical factors, EEG-determined encephalopathy severity, and MRI-based brain injury predict feeding supports (nasogastric tube, oral feeding compensations) and growth.
Results
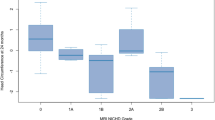
50.8% of infants required feeding supports in the hospital, decreasing to 14% at discharge. Moderate-to-severe encephalopathy and basal ganglia injury predicted feeding support needs. Yet, 35% of mildly encephalopathic infants required gavage tubes. Growth trajectories approximated expected growth of healthy infants.
Conclusion
Infants with neonatal encephalopathy—even if mild—frequently experience feeding difficulties during initial hospitalization. With support, most achieve full oral feeds by discharge and adequate early childhood growth. Clinical factors may help identify infants requiring feeding support, but do not detect all at-risk infants, supporting routine screening of this high-risk population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Jacobs SE, Berg M, Hunt R, Tarnow‐Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013;2013:CD003311.
de Vries LS, Jongmans MJ. Long-term outcome after neonatal hypoxic-ischaemic encephalopathy. Arch Dis Child - Fetal Neonatal Ed. 2010;95:F220–4.
Berseth CL, McCoy HH. Birth Asphyxia alters neonatal intestinal motility in term neonates. Pediatrics. 1992;90:669–73.
Martinez-Biarge M, Diez-Sebastian J, Wusthoff CJ, Lawrence S, Aloysius A, Rutherford MA, et al. Feeding and communication impairments in infants with central grey matter lesions following perinatal hypoxic-ischaemic injury. Eur J Paediatr Neurol. 2012;16:688–96.
Quattrocchi CC, Longo D, Delfino LN, Cilio MR, Piersigilli F, Capua MD, et al. Dorsal brain stem syndrome: MR imaging location of brain stem tegmental lesions in neonates with oral motor dysfunction. AJNR Am J Neuroradiol. 2010;31:1438–42.
Dodrill P, Gosa MM. Pediatric dysphagia: physiology, assessment, and management. Annal Nutr Metab. 2015;66:24–31.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic–ischemic encephalopathy. N Engl J Med. 2005;353:1574–84.
Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, et al. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:692-700.
Takle M, Conaway M, Burnsed J. Electroencephalogram background predicts time to full oral feedings in hypoxic-ischemic encephalopathy. Am J Perinatol. 2022;39:1678−81.
Thornton KM, Dai H, Septer S, Petrikin JE. Effects of whole body therapeutic hypothermia on gastrointestinal morbidity and feeding tolerance in infants with hypoxic ischemic encephalopathy. Raju TNK, editor. Int J Pediatr. 2014;2014:643689.
Tsuda K, Mukai T, Iwata S, Shibasaki J, Tokuhisa T, Ioroi T, et al. Therapeutic hypothermia for neonatal encephalopathy: a report from the first 3 years of the Baby Cooling Registry of Japan. Sci Rep. 2017;7:39508.
Bhagat I, Agarwal P, Sarkar A, Dechert R, Altinok D, Chouthai N. Does severity of brain injury on magnetic resonance imaging predict short-term outcome in neonates who received therapeutic hypothermia? Am J Perinatol. 2023;40:666−71.
Alburaki W, Scringer-Wilkes M, Dawoud F, Oliver N, Lind J, Zein H, et al. Feeding during therapeutic hypothermia is safe and may improve outcomes in newborns with perinatal asphyxia. J Matern Fetal Neonatal Med. 2022;35:9440–4.
Beltempo M, Wintermark P, Mohammad K, Jabbour E, Afifi J, Shivananda S, et al. Variations in practices and outcomes of neonates with hypoxic ischemic encephalopathy treated with therapeutic hypothermia across tertiary NICUs in Canada. J Perinatol. 2022;42:898–906.
Markus M, Giannakis S, Ruhfus M, Stein A, Heep A, Plagemann T, et al. Fluid supply and feeding practices in cooled asphyxiated newborns. Children. 2021;8:899.
Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, et al. Pediatric feeding disorder: consensus definition and conceptual framework. J Pediatr Gastroenterol Nutr. 2019;68:124–9.
Walsh BH, El-Shibiny H, Munster C, Yang E, Inder TE, El-Dib M. Differences in standardized neonatal encephalopathy exam criteria may impact therapeutic hypothermia eligibility. Pediatr Res. 2022;92:791–8.
Garvey AA, El-Shibiny H, Yang E, Inder TE, El-Dib M. Differences between early and late MRI in infants with neonatal encephalopathy following therapeutic hypothermia. Pediatr Res. 2023;94:1011–7.
Szakmar E, Meunier H, El-Dib M, Yang E, Inder TE. Interobserver reliability of an MR imaging scoring system in infants with hypoxic-ischemic encephalopathy. Am J Neuroradiol. 2021;42:969–74.
Weeke LC, Groenendaal F, Mudigonda K, Blennow M, Lequin MH, Meiners LC, et al. A novel magnetic resonance imaging score predicts neurodevelopmental outcome after perinatal asphyxia and therapeutic hypothermia. J Pediatrics. 2018;192:33–40.e2.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatri. 2006;95:76–85.
World Health Organization. WHO child growth standards: head circumference-for-age, arm circumference-for-age, triceps skinfold-for-age and subscapular skinfold-for-age: methods and development [Internet]. Geneva: WHO; 2007 [cited 2022 Mar 8]. Available from: https://www.who.int/publications-detail-redirect/9789241547185.
Azzopardi D, Strohm B, Linsell L, Hobson A, Juszczak E, Kurinczuk JJ, et al. Implementation and conduct of therapeutic hypothermia for perinatal asphyxial encephalopathy in the UK – analysis of national data. PLOS ONE. 2012;7:e38504.
Scherer J, Whybra-Trümpler C, Mildenberger E. [Results of the hypothermia registry of the University Hospital Dresden from 2010-2017. Application of hypothermia therapy in newborns in Germany]. Z Geburtshilfe Neonatol. 2020;224:367–73.
Gupta S, Bapuraj JR, Carlson G, Trumpower E, Dechert RE, Sarkar S. Predicting the need for home gavage or g-tube feeds in asphyxiated neonates treated with therapeutic hypothermia. J Perinatol. 2018;38:728–33.
Rao R, Mietzsch U, DiGeronimo R, Hamrick SE, Dizon MLV, Lee KS, et al. Utilization of therapeutic hypothermia and neurological injury in neonates with mild hypoxic-ischemic encephalopathy: a report from children’s hospital neonatal consortium. Am J Perinatol. 2022;39:319–28.
Yieh L, Lee H, Lu T, Song A, Gong CL, Wu TW, et al. Neonates with mild hypoxic-ischaemic encephalopathy receiving supportive care versus therapeutic hypothermia in California. Arch Dis Child Fetal Neonatal Ed. 2022;107:324–8.
Oliveira V, Singhvi DP, Montaldo P, Lally PJ, Mendoza J, Manerkar S, et al. Therapeutic hypothermia in mild neonatal encephalopathy: a national survey of practice in the UK. Arch Dis Child Fetal Neonatal Ed. 2018;103:F388–90.
Krüger E, Kritzinger A, Pottas L. Oropharyngeal dysphagia in breastfeeding neonates with hypoxic-ischemic encephalopathy on therapeutic hypothermia. Breastfeed Med. 2019;14:718–23.
Medoff Cooper B, Holditch-Davis D, Verklan MT, Fraser-Askin D, Lamp J, Santa-Donato A, et al. Newborn clinical outcomes of the AWHONN late preterm infant research-based practice project. J Obstet Gynecol Neonatal Nurs. 2012;41:774–85.
Laptook AR. Therapeutic hypothermia for preterm infants with hypoxic-ischemic encephalopathy: how do we move forward? J Pediatr. 2017;183:8–9.
Sarkar SS, Gupta S, Bapuraj JR, Dechert RE, Sarkar S. Brainstem hypoxic–ischemic lesions on MRI in infants treated with therapeutic cooling: effects on the length of stay and mortality. J Perinatol. 2021;41:512–8.
Gale C, Longford NT, Jeyakumaran D, Ougham K, Battersby C, Ojha S, et al. Feeding during neonatal therapeutic hypothermia, assessed using routinely collected National Neonatal Research Database data: a retrospective, UK population-based cohort study. Lancet Child Adolesc Health. 2021;5:408.
Chang LL, Wynn JL, Pacella MJ, Rossignol CC, Banadera F, Alviedo N, et al. Enteral feeding as an adjunct to hypothermia in neonates with hypoxic-ischemic encephalopathy. Neonatology. 2018;113:347–52.
Gale C, Jeyakumaran D, Battersby C, Ougham K, Ojha S, Culshaw L, et al. Nutritional management in newborn babies receiving therapeutic hypothermia: two retrospective observational studies using propensity score matching. Health Technol Assess. 2021;25:1–106.
Thyagarajan B, Tillqvist E, Baral V, Hallberg B, Vollmer B, Blennow M. Minimal enteral nutrition during neonatal hypothermia treatment for perinatal hypoxic-ischaemic encephalopathy is safe and feasible. Acta Paediatr. 2015;104:146–51.
Hazeldine B, Thyagarajan B, Grant M, Chakkarapani E. Survey of nutritional practices during therapeutic hypothermia for hypoxic-ischaemic encephalopathy. BMJ Paediatr Open. 2017;1:e000022.
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med. 2009;361:1349–58.
Azzopardi D, Strohm B, Marlow N, Brocklehurst P, Deierl A, Eddama O, et al. Effects of hypothermia for perinatal asphyxia on childhood outcomes. N Engl J Med. 2014;371:140–9.
Gardiner J, Wagh D, McMichael J, Hakeem M, Rao S. Outcomes of hypoxic ischaemic encephalopathy treated with therapeutic hypothermia using cool gel packs – Experience from Western Australia. Eur J Paediatr Neurol. 2014;18:391–8.
Maastrup R, Hansen BM, Kronborg H, Bojesen SN, Hallum K, Frandsen A, et al. Breastfeeding progression in preterm infants is influenced by factors in infants, mothers and clinical practice: the results of a national cohort study with high breastfeeding initiation rates. (Clifford T, editor) PLoS ONE. 2014;9:e108208.
Sachdev HP, Mehrotra S. Predictors of exclusive breastfeeding in early infancy: operational implications. Indian Pediatr. 1995;32:1287–96.
Buxton KE, Gielen AC, Faden RR, Brown CH, Paige DM, Chwalow AJ. Women intending to breastfeed: predictors of early infant feeding experiences. Am J Prev Med. 1991;7:101–6.
Azad MB, Vehling L, Chan D, Klopp A, Nickel NC, McGavock JM, et al. Infant feeding and weight gain: separating breast milk from breastfeeding and formula from food. Pediatrics. 2018;142:e20181092.
Funding
Jennifer Prial received funding from the Brigham and Women’s Hospital Division of Newborn Medicine Undergraduate Summer Student Research program.
Author information
Authors and Affiliations
Contributions
KAB conceptualized and designed the study; JP, HE-S, ME, ES, CE, JB, and KAB contributed to data acquisition; JP, HE-S, and KAB analyzed the data; JP and KAB drafted the original manuscript; and all authors interpreted the results, provided critical review of the manuscript draft and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prial, J., El-Shibiny, H., El-Dib, M. et al. Growth trajectories and need for oral feeding support among infants with neonatal encephalopathy treated with therapeutic hypothermia. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01983-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01983-7