Abstract
Objective
Estimate the causal effect of sex on outcomes in the neonatal intensive care unit (NICU) among very low birth weight (VLBW) infants.
Study design
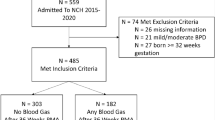
Retrospective cohort study using Vermont Oxford Network data to compare NICU outcomes for VLBW males versus females. Odds ratios (OR) for outcomes that differed significantly by sex were computed using standard unweighted analysis and inverse probability weighted (IPW) analysis to correct for selection bias.
Results
Using standard analysis, males were significantly more likely to die before discharge and experience six other adverse outcomes. From IPW analysis, male sex caused a 56% increase in the odds of death before discharge (OR = 1.56, 95% confidence interval: 1.18–1.94). Standard unweighted results were significantly biased towards increased risk of adverse outcomes for males (p = 0.005) compared to IPW results for which three outcomes were no longer significantly associated with male sex.
Conclusion
Standard statistical methods generally overestimate the casual effect of sex among VLBW infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Study data was obtained from, and all data definitions were governed by the Vermont Oxford Network (VON). The dataset analyzed for the current study is not publicly available due to IRB and VON policies that strictly protect the data as privileged and confidential, but the corresponding author will make every effort to accommodate reasonable requests for information about the study data.
References
Wyllie J. Sex differences in infant mortality. Can Public Health J. 1933;24:177–85.
Naeye RL, Burt LS, Wright DL, Blanc WA, Tatter D. Neonatal mortality, the male disadvantage. Pediatrics. 1971;48:902–6.
Kent AL, Wright IM, Abdel-Latif ME, New South Wales and Australian Capital Territory Neonatal Intensive Care Units Audit Group. Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics. 2012;129:124–31.
Jones HP, Karuri S, Cronin CMG, Ohlsson A, Pelioski A, Synnes A, et al. Actuarial survival of a large Canadian cohort of preterm infants. BMC Pediatr. 2005;5:40.
Serenius F, Ewald U, Farooqi A, Holmgren PÅ, Håkansson S, Sedin G. Short-term outcome after active perinatal management at 23-25 weeks of gestation. A study from two Swedish tertiary care centres. Part 2: infant survival. Acta Paediatr. 2004;93:1081–9.
Brothwood M, Wolke D, Gamsu H, Benson J, Cooper D. Prognosis of the very low birth weight baby in relation to gender. Arch Dis Child. 1986;61:559–64.
Vu HD, Dickinson C, Kandasamy Y. Sex differences in mortality for premature and low birth weight neonates: a systematic review. Am J Perinatol. 2018;35:707–15.
Binet ME, Bujold E, Lefebvre F, Tremblay Y, Piedboeuf B, for the Canadian Neonatal Network. Role of gender in morbidity and mortality of extremely premature neonates. Am J Perinatol. 2012;29:159–66.
Cuestas E, Bas J, Pautasso J. Sex differences in intraventricular hemorrhage rates among very low birth weight newborns. Gend Med. 2009;6:376–82.
Deulofeut R, Dudell G, Sola A. Treatment-by-gender effect when aiming to avoid hyperoxia in preterm infants in the NICU. Acta Paediatr. 2007;96:990–4.
Peelen MJ, Kazemier BM, Ravelli AC, De Groot CJM, Van Der Post JAM, Mol BWJ, et al. Impact of fetal gender on the risk of preterm birth, a national cohort study. Acta Obstet Gynecol Scand. 2016;95:1034–41.
O’Driscoll D, McGovern M, Greene CM, Molloy EJ. Gender disparities in neonatal outcomes. Acta Paediatr. 2018;107:1494–9.
Stevenson DK, Verter J, Fanaro AA, Oh W, Ehrenkranz RA, Shankaran S, et al. Sex differences in outcomes of very low birth weight infants: the newborn male disadvantage. Arch Dis Child Fetal Neonatal Ed. 2000;83:F182–185.
Garfinkle J, Yoon EW, Alvaro R, Nwaesei C, Claveau M, Lee SK. Trends in sex-specific differences in outcomes in extreme preterms: progress or natural barriers? Arch Dis Child Fetal Neonatal Ed. 2020;105:158–63.
Hernán MA, Robins JM. Causal Inference: What If. Chapman & Hall/CRC: Boca Raton, 2020.
Seri I, Evans J. Limits of viability: definition of the gray zone. J Perinatol. 2008;28:S4–S8.
Spiegler J, Schlaud M, König I, Teig N, Hubert M, Herting E, Göpel W, and the German Neonatal Network. Very low birth weight infants after discharge: what do parents describe? Early Hum Dev. 2013;89:343–7.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82.
Yu Q, Li B, Statistical Methods for Mediation, Confounding, and Moderation Analysis using R and SAS. Chapman & Hall/CRC: Boca Raton, 2022.
Campbell DM, MacGillivray I, Carr-Hill R, Samphier M. Fetal sex and pre-eclampsia in primigravidae. Br J Obstet Gynaecol. 1983;90:26–27.
McGregor JA, Leff M, Orleans M, Baron A. Fetal gender differences in preterm birth: findings in a North American cohort. Am J Perinatol 1992;9:43–48.
Cooperstock M, Campbell J. Excess males in preterm birth: interactions with GA, race, and multiple birth. Obstet Gynecol. 1996;88:189–93.
Astolfi P, Zonta LA. Risks of preterm delivery and association with maternal age, birth order, and fetal gender. Hum Reprod. 1999;14:2891–4.
Zeitlin J, Saurel-Cubizolles MJ, De Mouzon J, Rivera L, Ancel PY, Blondle B, et al. Fetal sex and preterm birth: are males at greater risk? Hum Reprod. 2002;17:2762–8.
Ingemarsson I. Gender aspects of preterm birth. Br J Obstet Gynaecol. 2003;110:34e8.
Di Renzo GC, Rosati A, Sarti RD, Cruciani L, Cutuli AM. Does fetal sex affect pregnancy outcome? Gend Med. 2007;4:19–30.
Cooper R, Power C. Sex differences in the associations between birthweight and lipid levels in middle-age: findings from the 1958 British birth cohort. Atherosclerosis. 2008;200:141–9.
Lao TT, Sahota DS, Suen SS, Law LW, Law TY. The impact of fetal gender on preterm birth in a southern Chinese population. J Matern Fetal Neonatal Med. 2011;24:1440–3.
Aibar L, Puertas A, Valverde M, Carrillo MP, Montoya F. Fetal sex and perinatal outcomes. J Perinat Med. 2012;40:271–6.
Yamakita M, Sato M, Suzuki K, Ando D, Yamagata Z. Sex differences in birthweight and physical activity in Japanese schoolchildren. J Epidemiol. 2018;28:331–5.
Stark MJ, Clifton VL, Wright IM. Sex-specific differences in peripheral microvascular blood flow in preterm infants. Pediatr Res. 2008;63:415–9.
Townsel CD, Emmer SF, Campbell WA, Hussain N. Gender differences in respiratory morbidity and mortality of preterm neonates. Front Pediatr. 2017;5:6.
Meakin AS, Cuffe J, Darby J, Morrison JL, Clifton VL. Let’s talk about placental sex, baby: understanding mechanisms that drive female- and male-specific fetal growth and developmental outcomes. Int J Mol Sci. 2021;22:6386.
Inkster AM, Fernández-Boyano I, Robinson WP. Sex differences are here to stay: relevance to prenatal care. J Clin Med. 2021;10:3000.
Bhaumik U, Aitken I, Kawachi I, Ringer S, Orav J, Lieberman E. Narrowing of sex differences in infant mortality in Massachusetts. J Perinatol. 2004;24:94–99.
Boghossian NS, Geraci M, Edwards EM, Horbar JD. Sex differences in mortality and morbidity of infants born at less than 30 weeks’ gestation. J Pediatr. 2018;142:e20182352.
Fröhlich M, Tissen-Diabaté T, Bührer C, Roll S. Sex-specific long-term trends in length of hospital stay, postmenstrual age at discharge, and survival in very low birthweight infants. Neonatology. 2021;118:416–24.
Lingappan K, Jiang W, Wang L, Moorthy B. Sex-specific differences in neonatal hyperoxic lung injury. Am J Physiol Lung Cell Mol Physiol. 2014;311:L481–493.
Namba F, Ogawa R, Ito M, Watanabe T, Dennery PA, Tamura M. Sex-related differences in long-term pulmonary outcomes of neonatal hyperoxia in mice. Exp Lung Res. 2016;42:57–65.
Bennet L, Galinsky R, Draghi V, Lear CA, Davidson JO, Unsworth CP, et al. Time and sex dependent effects of magnesium sulphate on post-asphyxial seizures in preterm fetal sheep. J Physiol. 2018;596:6079–92.
Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. National Institute of Child Health and Human Development Neonatal Research Network. intensive care for extreme prematurity–moving beyond GA. N Engl J Med. 2008;358:1672–81.
Ohlsson A, Roberts RS, Schmidt B, Davis P, Moddeman D, Saigal S. Male/female differences in indomethacin effects in preterm infants. J Pediatr. 2005;147:860–2.
Baud O, Maury L, Lebail F, Ramful D, El Moussawi F, Nicaise C, et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): a double-blind, placebo-controlled, multicentre, randomised trial. Lancet. 2016;387:1827–36.
Tottman AC, Oliver CJ, Alsweiler JM, Cormack BE. Do preterm girls need different nutrition to preterm boys? Sex-specific nutrition for the preterm infant. Pediatr Res. 2021;89:313–7.
Bren L. Does sex make a difference? FDA Consum. 2005;39:10–15.
Clayton JA, Collins FS. Policy: NIH to balance sex in cell and animal studies. Nature. 2014;509:282–3.
Rosenbaum PR, Rubin DB. The bias due to incomplete matching. Biometrics. 1985;41:103–16.
Schuster NA, Twisk JWR, ter Riet G, Heymans MW, Rijnhart JJM. Noncollapsibility and its role in quantifying confounding bias in logistic regression. BMC Med Res Methodol. 2021;21:136.
Hernan MA, Clayton D, Keiding N. The Simpson’s paradox unraveled. Int J Epidemiol. 2011;40:780–5.
Daniel R, Zhang J, Farewell D. Making apples from oranges: comparing noncollapsible effect estimators and their standard errors after adjustment for different covariate sets. Biomet J. 2020;63:528–57.
Pang M, Kaufman JS, Platt RW. Studying noncollapsibility of the odds ratio with marginal structural and logistic regression models. Stat Methods Med Res. 2016;25:1925–37.
Janes H, Dominici F, Zeger S. On quantifying the magnitude of confounding. Biostatistics. 2010;11:572–82.
Funding
No funding was received to conduct this study.
Author information
Authors and Affiliations
Contributions
The study was conceived of and conducted solely by JH.
Corresponding author
Ethics declarations
Competing interests
The author declares no competing interests.
Ethics approval and consent to participate
This study was approved by the Baylor College of Medicine Institutional Review Board (IRB, protocol H-51590) with a waiver of consent to participate due to the retrospective design posing minimal risks to subjects. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hagan, J.L. Estimation of the causal effect of sex on neonatal intensive care unit outcomes among very low birth weight infants. J Perinatol (2024). https://doi.org/10.1038/s41372-024-01989-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-024-01989-1