Abstract
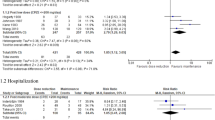
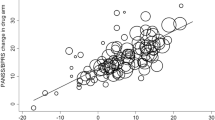
The response to antipsychotic treatment in schizophrenia appears to vary, and as such it has been proposed that different subtypes of schizophrenia exist, defined by treatment-response. This has not been formally examined using meta-analysis. Randomised controlled trials comparing placebo and antipsychotics in acute treatment of schizophrenia listed in PubMed, EMBASE and PsycINFO from inception until 30 November 2018 were examined. Relative variability of symptomatic improvement in antipsychotic-treated individuals compared to placebo-treated individuals was quantified using coefficient of variation ratio (CVR). Mean difference in symptom change was quantified using Hedges’ g. In addition, individual patient data from two clinical trials was examined in terms of both the distribution of total symptom change, and the variability of individual symptoms and symptom factors. In total, 11,006 articles were identified. Sixty six met inclusion criteria, reporting on 17,202 patients. Compared with placebo, antipsychotic-treated patients demonstrated greater total symptom improvement (g = 0.47, p < 0.001) and reduced variability in symptomatic improvement for total (CVR = 0.86, p < 0.001), positive (CVR = 0.89, p < 0.001), and negative symptoms (CVR = 0.86, p = 0.001). Lower variability in antipsychotic-response relative to placebo was associated with studies published earlier (z = 3.98, p < 0.001), younger patients (z = 3.07, p = 0.002), higher dose treatments (z = −2.62, p = 0.009), and greater mean-difference in symptom-change (z = −5.70, p < 0.001). In the individual patient dataset (N = 522 patients), antipsychotic treated patients did not show significantly increased variability for any individual symptom, and there was no evidence of a bimodal distribution of response. Compared to placebo, antipsychotic treatment shows greater improvement and lower variability of change in total, positive and negative symptoms. This is contrary to the hypothesis that there is a subtype of antipsychotic non-responsive schizophrenia. Instead our findings, provide evidence for a relatively homogeneous effect of antipsychotic treatment in improving symptoms of schizophrenia.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Howes O, Murray R. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;6736:1–11.
Leucht S, Cipriani A, Spineli L, Mavridis D, Örey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 2013;6736:1–12.
Kaar SJ, Natesan, S., McCutcheon R, Howes OD. Antipsychotics: mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacol. 2019;107704.
Agid O, Arenovich T, Sajeev G, Zipursky RB, Kapur S, Foussias G, et al. An algorithm-based approach to first-episode schizophrenia: response rates over 3 prospective antipsychotic trials with a retrospective data analysis. J Clin Psychiatry. 2011;72:1439–44.
Marques TR, Arenovich T, Agid O, Sajeev G, Muthén B, Chen L, et al. The different trajectories of antipsychotic response: antipsychotics versus placebo. Psychol Med. 2011;41:1481–8.
Lally J, Ajnakina O, Di Forti M, Trotta A, Demjaha A, Kolliakou A, et al. Two distinct patterns of treatment resistance: clinical predictors of treatment resistance in first-episode schizophrenia spectrum psychoses. Psychol Med. 2016;46:3231–40.
Demjaha A, Lappin JM, Stahl D, Patel MX, MacCabe JH, Howes OD, et al. Antipsychotic treatment resistance in first-episode psychosis: prevalence, subtypes and predictors. Psychol Med. 2017;47:1981–89.
Howes OD, McCutcheon R, Agid O, de Bartolomeis A, van Beveren NJ, Birnbaum ML, et al. Treatment-Resistant Schizophrenia: Treatment Response and Resistance in Psychosis (TRRIP) Working Group Consensus Guidelines on Diagnosis and Terminology. Am J Psychiatry. 2017;174:216–29.
Howes OD, Kapur S. A neurobiological hypothesis for the classification of schizophrenia: Type a (hyperdopaminergic) and type b (normodopaminergic). Br J Psychiatry. 2014;205:1–3.
Crow TJ. The two-syndrome concept: origins and current status. Schizophr Bull. 1985;11:471–88.
Senn S. Statistical pitfalls of personalized medicine. Nature. 2018;563:619–21.
Nakagawa S, Poulin R, Mengersen K, Reinhold K, Engqvist L, Lagisz M, et al. Meta-analysis of variation: ecological and evolutionary applications and beyond. Methods Ecol Evol. 2015;6:143–52.
Brugger SP, Howes OD. Heterogeneity and homogeneity of regional brain structure in schizophrenia. JAMA Psychiatry. 2017;74:1104.
Pillinger T, Osimo EF, Brugger S, Mondelli V, Mccutcheon RA, Howes OD. A meta-analysis of immune parameters, variability, and assessment of modal distribution in psychosis and test of the immune subgroup hypothesis. 2018;1–14. https://doi.org/10.1093/schbul/sby160.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–34.
Leucht S, Leucht C, Huhn M, Chaimani A, Mavridis D, Helfer B, et al. Sixty years of placebo-controlled antipsychotic drug trials in acute schizophrenia: systematic review, bayesian meta-analysis, and meta-regression of efficacy predictors. Am J Psychiatry. 2017;174:927–42.
Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261.
Overall JE. Gorham DoR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10:799–812.
Andreasen NC. Scale for the assessment of negative symptoms. Iowa City: University of Iowa; 1984.
Andreasen NC. Scale for the assessment of positive symptoms. Iowa City: University of Iowa; 1984.
Higgins JP, Green S Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons, 2008. https://doi.org/10.1002/9780470712184.ch5.
Leucht S, Samara M, Heres S, Davis JM. Dose equivalents for antipsychotic drugs: the ddd method: Table 1. Schizophr Bull. 2016;42:S90–S94.
Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry Clin Neurosci. 2015;69:440–7.
Eisler Z, Bartos I, Kertész J. Fluctuation scaling in complex systems: Taylor’s law and beyond. Adv Phys. 2008;57:89–142.
Marder S, Meibach R. Risperidone in the treatment of schizophrenia. Am J Psychiatry. 1994;151:825–35.
Chouinard G, Jones B, Remington G, Bloom D, Addington D, Macewan GW, et al. A Canadian multicenter placebo-controlled study of fixed doses of risperidone and haloperidol in the treatment of chronic schizophrenic patients. J Clin Psychopharmacol. 1993;13:25–40.
Marder SR, Davis JM, Chouinard G. The effects of risperidone on the five dimensions of schizophrenia derived by factor analysis: combined results of the North American trials. J Clin Psychiatry. 1997;58:538–46.
Hartigan J, Hartigan P. The dip test of unimodality. Ann Stat. 1985;13:70–84.
Viechtbauer W. Conducting meta-analyses in R with the metafor Package. J Stat Softw. 2010;36:1–48.
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
Vijverberg SJH, Farzan N, Slob EMA, Neerincx AH, Maitland-van der Zee AH. Treatment response heterogeneity in asthma: the role of genetic variation. Expert Rev Respir Med. 2018;12:55–65.
Cantrell RA, Alatorre CI, Davis EJ, Zarotsky V, Le Nestour E, Carter GC, et al. A review of treatment response in type 2 diabetes: Assessing the role of patient heterogeneity. Diabetes, Obes Metab. 2010;12:845–57.
Schork NJ. Personalized medicine: Time for one-person trials. Nature. 2015;520:609–11.
Marwick KFM, Stevenson AJ, Davies C, Lawrie SM. Application of n-of-1 treatment trials in schizophrenia: Systematic review. Br J Psychiatry. 2018;213:398–403.
Correll CU. From receptor pharmacology to improved outcomes: Individualising the selection, dosing, and switching of antipsychotics. Eur Psychiatry. 2010;25:S12–S21.
Howes O, McCutcheon R, Stone J. Glutamate and dopamine in schizophrenia: an update for the 21 st century. J Psychopharmacol. 2015;29:97–115.
Rutherford BR, Pott E, Tandler JM, Wall MM, Roose SP, Lieberman JA. Placebo response in antipsychotic clinical trials ameta-analysis. JAMA Psychiatry. 2014;71:1409–21.
Agid O, Siu CO, Potkin SG, Kapur S, Watsky E, Vanderburg D, et al. Meta-Regression Analysis of Placebo Response in Antipsychotic Trials, 1970–2010. Am J Psychiatry. 2013;170:1335–44.
Wager TD, Atlas LY. The neuroscience of placebo effects: connecting context, learning and health. Nat Rev Neurosci. 2015;16:403–18.
Kaptchuk TJ, Miller FG. Placebo effects in medicine. N Engl J Med. 2015;373:8–9.
Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: recent advances and current thought. Annu Rev Psychol. 2008;59:565–90.
Petrovic P. Placebo and opioid analgesia- imaging a shared neuronal network. Science. 2002;295:1737–40.
Acknowledgements
RM’s work is supported by a clinical research training fellowship grant from the Wellcome trust (no. 200102/Z/15/Z). OH’s work is supported by Medical Research Council-UK (no. MC-A656-5QD30), Maudsley Charity (no. 666), Brain and Behavior Research Foundation, and Wellcome Trust (no. 094849/Z/10/Z) grants, and the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Contributions
Study conception: RM, TP,YM, OH; Study design: RM, TP, YM, AM, HP, LV, OH; Data searching and extraction: RM, TP, YM, AM, HP, LV; Data analysis: RM Data interpretation: RM, TP, YM, OH; Writing of manuscript: RM, TP, YM, AM, HP, LV, OH.
Corresponding author
Ethics declarations
Conflict of interest
RM, TP, AM, HP and LV declare no financial conflicts of interest. YM has received manuscript fees or speaker’s honoraria from Sumitomo Dainippon Pharma and Yoshitomi Yakuhin, fellowship grants from Japan Society for the Promotion of Science, Astellas Foundation for Research on Metabolic Disorders, Japanese Society of Clinical Neuropsychopharmacology, and Mochida Memorial Foundation for Medical and Pharmaceutical Research, and consultant fees from Bracket within the past three years. ODH has received investigator-initiated research funding from and/or participated in advisory/speaker meetings organised by Astra-Zeneca, Autifony, BMS, Eli Lilly, Heptares, Jansenn, Lundbeck, Lyden-Delta, Otsuka, Servier, Sunovion, Rand and Roche. Neither ODH or his family have been employed by or have holdings/a financial stake in any biomedical company.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
McCutcheon, R.A., Pillinger, T., Mizuno, Y. et al. The efficacy and heterogeneity of antipsychotic response in schizophrenia: A meta-analysis. Mol Psychiatry 26, 1310–1320 (2021). https://doi.org/10.1038/s41380-019-0502-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-019-0502-5
This article is cited by
-
Glutamatergic basis of antipsychotic response in first-episode psychosis: a dual voxel study of the anterior cingulate cortex
Neuropsychopharmacology (2024)
-
Interaction between baseline BMI and baseline disease severity predicts greater improvement in negative symptoms in first-episode schizophrenia
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
Clinical insight among persons with schizophrenia spectrum disorders treated with amisulpride, aripiprazole or olanzapine: a semi-randomised trial
BMC Psychiatry (2023)
-
Transcriptional signatures of the whole-brain voxel-wise resting-state functional network centrality alterations in schizophrenia
Schizophrenia (2023)
-
Neuroimaging biomarkers define neurophysiological subtypes with distinct trajectories in schizophrenia
Nature Mental Health (2023)