Abstract
Background
Iron (Fe) status of neonates born to women carrying multiple fetuses might be compromised as a consequence of the high prevalence of maternal Fe deficiency and anemia coupled with an increased risk of preterm birth. This study aimed to characterize and identify determinants of anemia in this neonatal population.
Methods
Umbilical cord blood obtained from 183 neonates was utilized to assess hemoglobin (Hb), ferritin (SF), soluble transferrin receptor (sTfR), hepcidin, serum Fe, erythropoietin, folate, vitamin B-12, C-reactive protein, and interleukin-6. Associations with maternal Fe status were explored.
Results
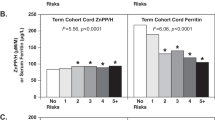
Cord Hb or SF did not change significantly as a function of gestational age at birth (25–38 wks). Neonates born to women who were obese prior to pregnancy or smoked cigarettes during pregnancy had a 4–5-fold greater odds of anemia at birth. Cord sTfR was the strongest indicator of cord Hb (P < 0.0001), and it was significantly associated with maternal sTfR at mid-gestation (P = 0.01) and delivery (P = 0.002). Cord Fe indicators were significantly associated with cord hepcidin, but not maternal hepcidin.
Conclusion
Screening for Fe status in neonates born to women carrying multiple fetuses is warranted, especially for those born to smokers or to women who are obese at entry into pregnancy.
Similar content being viewed by others
Introduction
Multiple births currently account for nearly 3.5% of all births in the US.1 The health of neonates born to women carrying multiple fetuses is of concern as this group alone is responsible for 15% of all preterm births (PTB) and 20% of all low birth weight (LBW) infants born in the US.2 To date, little attention has been placed on the unique nutritional concerns of this population. Iron (Fe) in particular merits attention, given its role in early brain growth and function.3 Maternal anemia also significantly increases risk of LBW and PTB.4, 5 Evidence suggests that neonatal Fe status may be compromised as a consequence of maternal Fe deficiency (ID).6, 7
Fetal Fe accretion increases nearly 10-fold from 0.8 mg/day in the 1st trimester to roughly 7.5 mg/day during the 3rd trimester.8 Little is known about the ability of the pregnant gravida to modify Fe partitioning in order to supply multiple fetuses with sufficient Fe at birth. As PTB is prevalent among women with multiple gestations and most Fe is accrued over late pregnancy, early delivery may predispose these neonates to suboptimal Fe stores at birth. A growing literature emphasizes the unique Fe partitioning that occurs in utero to allow Fe to be prioritized for erythropoiesis at the cost of fetal brain and cardiac Fe requirements.7, 9
Few studies have examined the prevalence of anemia in neonates born to women carrying multiple fetuses. The latest American Academy of Pediatrics (AAP) publication on ID and Fe deficiency anemia (IDA) among infants 0–3 years of age highlighted an increased risk of anemia in preterm and small-for-gestational age (SGA) infants but did not mention multiples as a group at higher risk.10 The last published American College of Obstetricians and Gynecologists (ACOG) practice bulletin on anemia in pregnancy did not identify women carrying multiple fetuses as an at-risk obstetric population and made no additional Fe intake recommendations for this group.11 More data in this higher risk population are needed.
We recently reported an increased risk of maternal anemia and ID in a large cohort of women with multiple gestations.12 Given the known associations between maternal and neonatal Fe status, the high prevalence of PTB among multiples, and the increased risk of poor neonatal Fe stores due to PTB, the goal of this study was to characterize neonatal Fe status at birth and identify significant determinants of ID and anemia in newborns born to women carrying multiples fetuses. Because anemia is the last stage of Fe depletion, additional normative data on Fe status in vulnerable groups are needed in relation to gestational age (GA) at birth and maternal Fe status across gestation.
Subjects and methods
Participants
Women (≥19 years) carrying twins, triplets, or quadruplets were recruited between 2011 and 2014 from Strong Memorial Hospital and Highland Hospital at the University of Rochester, in Rochester, NY. Exclusion criteria included HIV infection, pre-existing diabetes, malabsorption diseases, hemoglobinopathies, or other medical problems known to affect Fe homeostasis. The clinical trial registry number is NCT01582802. This study was approved by the Institutional Review Boards of the University of Rochester and Cornell University. Data on Fe status12 and determinants of umbilical cord coiling13 in these women have been published.
All women were prescribed standard prenatal supplements containing between 27 and 90 mg of Fe. GA was determined as previously described.12 Maternal pre-pregnancy body mass index (ppBMI) was characterized as underweight ( < 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), or obese (30–34.9 kg/m2).14 Birth weight, GA at birth, delivery mode, and Apgar scores were abstracted from medical records. Delayed cord clamping was not a standard practice for multiple gestations at the time this study was implemented. Neonates were categorized as preterm (<37 wks) or early term (37–39 wks).15 Growth rate at birth was assessed using the Fenton growth charts and birth weight <10th percentile was defined as SGA.16, 17 Discordant growth between siblings was evaluated by subtracting the smaller from the larger neonatal weight and then dividing by the larger weight. Discordant growth was defined as a difference in birth weight between twin, triplet, or quadruplet siblings >15 or 25%.18
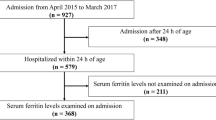
A total of 186 neonates (64 sets of twins, 18 sets of triplets, and 1 set of quadruplets) born to 83 women (aged 30.3 ± 5.1 years) were recruited. There were no significant differences in baseline maternal characteristics between the entire cohort of 83 women and the two sub-groups of participants that provided blood samples during pregnancy and/or at delivery.12 Three cases of neonatal mortality occurred resulting in a final study population of 183 neonates (53% were female). Umbilical cord blood samples were not collected from 39 neonates at birth due to emergency delivery conditions.
Cord blood collection and biochemical analyses
Cord hemoglobin (Hb) was measured at the Strong Memorial Hospital clinical laboratory using Cell-Dyn 4000 system (Abbott, Santa Clara, CA). Neonatal anemia was defined as a cord Hb < 13 g/dL using published reference data.19 Cord serum ferritin (SF) and soluble transferrin receptor (sTfR) were analyzed using ELISAs (Ramco, Stafford, TX) with the intra- and inter-assay coefficients of variation 7.9% and 4.7% for SF, respectively, and 5.9% and 2.1% for sTfR, respectively. Cord hepcidin was assessed using a hepcidin-25 enzyme immunoassay (Bachem, Torrance, CA). Hepcidin concentrations ≤ 0.39 ng/mL were categorized as undetectable and assigned a value of 0.195 ng/mL. Serum Fe was measured using graphite furnace atomic absorption spectrophotometry (Perkin Elmer AAnalyst 800). A National Bureau of Standards reference control of bovine liver serum (Standard Reference Material 1577c) was used as a control.
Cord C-reactive protein (CRP) was measured using a Quantikine ELISA kit with the intra- and inter-assay coefficients of variation 5.5% and 6.5%, respectively. Interleukin-6 (IL-6) was measured using a high sensitivity Quantikine ELISA kit (R&D System, MN) with the intra- and inter-assay coefficients of variation 7.4% and 7.7%, respectively. CRP values < 0.078 mg/L and IL-6 values < 0.156 ng/mL were below the assay limit of detection and were assigned values of 0.039 mg/L and 0.078 ng/mL, respectively. Erythropoietin (EPO), folate, and vitamin B-12 were analyzed using a Siemens Immulite® 2000 immunoassay system. Insufficiency was defined when folate concentrations were <6.8 nmol/L or vitamin B-12 concentrations were <146 pmol/L.20 Maternal Fe and inflammation indicators were collected at scheduled prenatal visits and were obtained on average at 24.4 ± 5.4 wks of gestation. Maternal and cord blood samples were also obtained at delivery (35.3 ± 2.3 wks). Biochemical measures in these samples were analyzed as detailed.12 All Fe status indicators and inflammatory markers were assayed in duplicate. For folate and vitamin B-12, only 15% of the samples were assayed in duplicate.
Statistical analysis
Normality of distributions for each continuous study measure was tested using the Shapiro–Wilk test and means were calculated using a random-effects model to control for non-independence of multiple siblings. Non-normally distributed data were logarithmic transformed and the geometric means were calculated. Maternal characteristics between the twins and triplets/quadruplets groups were compared using a two-tailed t-test. The χ2 test of independence was used for analyses involving categorical variables. Because neonates born to the same mother are not independent, neonatal characteristics between twins and triplets/quadruplets groups were compared using a mixed model with random effects. The same mixed model was used between siblings to evaluate possible associations between cord and maternal Fe status indicators, and the Bonferroni test (P < 0.002) was used to correct for multiple comparisons. A generalized linear mixed model was applied to control for the dependence of Fe status between siblings and to identify significant determinants of neonatal anemia. Potential confounders, including gestational weight gain (GWG), gestational age, and birth weight, were included in all models as covariates. The neonatal sample size was sufficient to detect correlations on the order of 0.15–0.20, with an alpha level of 0.05. All statistical analyses were performed using JMP 12.0 (SAS Institute Inc, Cary, NC).
Results
Maternal and neonatal characteristics
Maternal (n = 83) and neonatal (n = 183) characteristics are presented in Table 1. Compared to women carrying twins, as expected, women carrying higher order multiples (triplets and quadruplets) had a significantly higher incidence of preterm/very preterm delivery, cesarean section, and neonatal discordant growth. Significantly fewer African-American women delivered triplets and only one of them conceived using ARTs. Based on self-reported pre-pregnancy weight, 20% of women were overweight (n = 17/83) and 33% (n = 27/83) were obese. Compared to twins, the triplets/quadruplet group had a significantly lower mean birth weight (P = 0.0002).
In these 183 neonates, nearly 70% of neonates were born prematurely (<37 wks) and the remainder were born early term (37–38 wks). A quarter of the PTBs observed (n = 31/124) were due to premature rupture of membranes and the remaining 36% of PTB’s (n = 44/124) were due to other pregnancy related complications including preeclampsia, HELLP, fetal death, intrauterine growth restriction, and peripartum cardiomyopathy, complications that can occur in multiple births. The majority of neonates studied (74%) were delivered by cesarean section. Twin to twin transfusion syndrome was found in a set of monochorionic, and a set of dichorionic twins and in both instances was successfully treated by laser surgery early in pregnancy. Neonatal birth weight averaged 2206.5 ± 571.5 g, 71% of neonates (n = 130/183) were LBW and among these, 13% (n = 17/130) were very LBW (<1500 g). In this group of neonates, 22% were born SGA.
Neonatal anemia, and cord Fe status and inflammation at birth
Neonatal anemia, Fe status, and inflammatory markers are presented in Table 2. Anemia was found in 14% (n = 22/153) of neonates at birth. No significant difference in the prevalence of anemia was found between the preterm and early-term neonates [16% (n = 16/102) vs. 12% (n = 6/51), P = 0.3] and Hb was not significantly associated with GA at birth in this cohort (across the range of 25–38 wks of gestation). The prevalence of anemia did not significantly differ between LBW and normal-weight neonates [14% (n = 15/110) vs. 16% (n = 7/43), P = 0.7]. Mean cord Hb in our study population was compared to normative cord Hb data matched for GA using published data from 24,416 singletons (GA from 20–42 wks) (Fig. 1).21 Mean cord Hb concentrations in our neonates fell below the mean expected for singletons at all GA, and Hb began to further diverge from the mean at ~31 wks.
Mean cord Hb of multiple birth neonates (solid blue line) was compared to published reference ranges in 24,416 singletons born between 22 and 42 wks of gestation (solid black line).21 The Hb curve (adjusted for the non-independence of the multiple siblings) in our population tended to fall below the normative curve, and a marked reduction was evident at 34 wks of gestation. Source: Adapted from Jopling et al.21
Similar to findings for Hb, using a mixed model with random effects, no significant differences in cord SF, EPO, serum Fe, IL-6, or CRP were evident between the preterm and early-term neonates. In addition, GA had no significant association with cord SF, serum Fe, IL-6, or CRP across the GA at birth in this cohort. Using the same statistical method, cord sTfR (β = 0.04, SE = 0.02, P = 0.02, n = 144), EPO (β = 0.10, SE = 0.03, P = 0.001, n = 138), and hepcidin (β = 0.11, SE = 0.05, P = 0.05, n = 144) were significantly associated with GA at birth. Preterm neonates (33.2 ± 2.4 wks of gestation) had significantly lower cord hepcidin (14.8 ng/mL, n = 92 vs. 20.8 ng/mL, n = 50, P = 0.03) compared to early-term neonates (37.5 ± 0.5 wks gestation) after controlling for the non-independence of multiple birth siblings.
Because discordant growth was common in these neonates, to further evaluate the degree to which variable birth weight might have influenced observed associations between GA and Fe status, all Fe status indicators were expressed on a per kg of body weight basis and potential associations with GA were reexamined. Cord sTfR/kg birth weight (β = −0.05, SE = 0.02, P = 0.002, n = 144) and serum Fe/kg birth weight (β = −0.11, SE = 0.02, P < 0.0001, n = 140) were negatively associated with GA at birth such that significantly higher concentrations of these indicators/kg birth weight were evident in neonates born at an earlier GA. All other Fe status indicators did not significantly vary across the window of 25–38 wks when expressed on a per kg basis.
Hepcidin was detectable at birth (37.5 ± 0.7 wks) in all but 2 of the neonates studied. Both of these 2 neonates were non-anemic and they were born at 37 wks or 35 wks of gestation. Deficiencies of vitamin B-12 or folate were not evident in any of the neonates studied, and all neonates had detectable IL-6 at birth (25–38 wks) with values ranging from 0.46 to 40.24 pg/mL. In contrast, 69% of neonates (n = 93/134) had undetectable cord CRP. In neonates with detectable cord CRP (n = 41), a significant positive association was found between cord CRP and cord IL-6 (β = 0.48, SE = 0.10, P < 0.0001, n = 39).
Predictors of neonatal anemia at birth
Neonates born to women who were obese before entering pregnancy had more than a 4-fold greater odds of having anemia at birth compared to neonates born to normal-weight women (odds ratio (OR) = 4.1 [95% confidence interval (CI): 1.3, 15.6], P = 0.02) using a mixed model with random effects and adjusting for birth weight and GWG. Using the same method, neonates born to women who smoked during pregnancy (n = 12) had a nearly 5-fold greater odds of having anemia compared to neonates born to non-smokers (OR = 4.5 [95% CI: 1.1 17.3], p = 0.03). When the OR examining the impact of smoking on anemia was evaluated after adjusting for birth weight and GWG, the impact of smoking during pregnancy on anemia was reduced and only approached significance (OR = 4.2, [95% CI: 0.97, 16.6], P = 0.07) (Table 3). Prevalence of anemia did not significantly differ as a function of race (14% in Caucasian vs. 16% in African-American neonates, P = 0.6). Cord Hb was positively associated with Apgar scores at both 1 and 5 min (β = 0.26, SE = 0.09, P = 0.005, n = 154; β = 0.48, SE = 0.15, P = 0.002, n = 154, respectively) after adjusting for GA and birth weight.
Correlations between cord Hb and other cord Fe indicators
Significant associations were found between Hb and all cord Fe status indicators evaluated except for serum Fe and EPO after correcting for multiple comparisons using a Bonferroni test (P < 0.002). Cord SF, sTfR, EPO, and hepcidin were also significantly correlated (Table 4). Cord sTfR exhibited the strongest correlation with Hb, and alone captured 41% of the total variance in Hb, followed by hepcidin, which explained 37% of the total variance in Hb. A significant inverse association was evident between Hb and SF (β = −1.1, SE = 0.23, P < 0.0001, n = 126), a finding that remained significant after adjusting for GA and birth weight. Anemia did not occur in neonates with SF under the 10th percentile (40.8 μg/L), but was present in 21% (n = 3/14) of neonates whose SF was greater than the 90th percentile (250.7 μg/L). Cord IL-6 and CRP did not significantly differ between neonates whose cord SF concentrations were either <10th or >90th percentiles.
Correlations between maternal and cord iron status
Cord sTfR was significantly positively associated with maternal sTfR at 24.4 ± 5.4 wks (β = 0.25, SE = 0.09, P = 0.01, n = 128) and at delivery (34.6 ± 2.8 wks) (β = 0.25, SE = 0.08, P = 0.002, n = 120). At delivery, positive associations were also found between cord Hb and maternal Hb (β = 0.37, SE = 0.16, P = 0.02, n = 153) and hepcidin (β = 0.22, SE = 0.08, P = 0.008, n = 118). However, while cord and maternal hepcidin were correlated, only cord hepcidin was significantly correlated with umbilical cord Fe status indicators, including Hb (β = −0.83, SE = 0.17, P < 0.0001, n = 126), SF (β = 0.53, SE = 0.05, P < 0.0001, n = 144), sTfR (β = −0.23, SE = 0.03, P < 0.0001, n = 144), and EPO (β = −0.35, SE = 0.06, P < 0.0001, n = 138). Associations between maternal hepcidin and cord Fe status only approached significance for cord SF (β = 0.13, SE = 0.06, P = 0.06, n = 118) and cord sTfR (β = −0.08, SE = 0.04, P = 0.054, n = 118).
Discussion
To our knowledge, this is the largest study to explore Fe status in neonates born to women with multiple gestations and to evaluate temporal changes in neonatal Fe status in neonates born between 25 and 38 wks of gestation. Of note, anemia was present in 14% of neonates studied. Neonates born to obese women and women who smoked during pregnancy had significantly greater odds of anemia at birth. Hepcidin was detectable at birth in nearly all neonates born between 25 and 38 wks of gestation. Cord hepcidin, but not maternal hepcidin, was significantly associated with multiple umbilical cord Fe status indicators suggesting that the neonate independently regulated its Fe status.
At birth, anemia was evident in 14% of neonates studied. There are no national data on anemia prevalence in singleton newborns for direct comparison as NHANES data did not enroll those under 1 year of age.22 Compared to reference cord Hb data from 24,416 singleton neonates (22–42 wks of gestation),21 our Hb curve diverged from the reference curve at ~31 wks of gestation, and a marked reduction was evident by 34 wks of gestation. This likely reflects an inability of placental transport to keep pace with the rapid fetal growth of multiple fetuses,23 as the fetal growth trajectory in multiple pregnancies is also known to diverge from the singleton reference curve between 30 and 32 wks of gestation.24, 25
The AAP highlighted PTB as a risk factor for neonatal anemia.10 In our population, preterm neonates did not have an increased risk of anemia compared to early-term neonates, however because we had a power of only 79%, we were not sufficiently powered to evaluate possible differences in anemia between these two groups. Moreover, a longer duration in utero did not result in a significant accumulation of Fe stores or Hb, although body Fe continued to accumulate as each Fe indicator remained constant across gestation when expressed on a per kg of body weight basis. This finding differs from data in preterm singletons where many studies have found a higher risk of anemia and lower Fe status in preterm singleton newborns.26, 27 The lack of an impact of gestational age on fetal Fe accumulation may be a consequence of the increased Fe required to endow multiple fetuses, which may limit optimal Fe accumulation across late gestation.
Risk of anemia was 4-fold higher in neonates born to women who were obese before pregnancy. The adverse effect of maternal ppBMI on neonatal anemia was evident only in women whose ppBMI exceeded 30 kg/m2; no differences in hematological measures were noted in neonates born to women who were overweight (25–30 kg/m2) at entry into pregnancy. Data on maternal obesity and neonatal Fe status are limited and often contradictory. We previously found that adolescents (n = 230) in higher ppBMI categories gave birth to neonates with significantly higher cord Hb,28 but these unexpected findings may be due to biological immaturity of the adolescent as animal models have suggested that maternal–fetal nutrient partitioning differs among adolescents compared to adults.29, 30 In primarily adult populations, studies in 316 US gravida31 and 1613 pregnant Chinese women,32 found adverse effects of maternal obesity on neonatal Fe stores. Further studies are needed to understand the impact of maternal obesity on neonatal Fe status in some, but not all, populations.
Risk of neonatal anemia was higher in multiple birth neonates whose mothers smoked during pregnancy. Although studies have found cigarette smoking to be negatively associated with neonatal ferritin, transferrin, and total body Fe,33, 34 few data are available on maternal cigarette smoking and risk of neonatal anemia. Because cigarette smoking is a modifiable risk factor, its adverse effects on neonatal anemia in women carrying multiples should be highlighted especially as it is also known to be a risk factor for PTB, LBW, fetal growth restriction and infant death,35 outcomes that already occur at increased rates in multiple birth neonates.
To date, data on associations between cord and maternal hepcidin have been mixed.36,37,38 In our study, cord hepcidin was significantly associated with maternal hepcidin at delivery, but only cord hepcidin was correlated with cord Fe status, and this hormone alone captured nearly 37% of the total variance in cord Hb. These data suggest that the fetus independently regulates its Fe status, a finding consistent with other data from full-term singleton neonates.36, 37
In these multiple birth neonates, the majority of cord Fe status indicators evaluated exhibited the expected associations with cord Hb based on existing associations published in term or preterm singletons.37, 39 Among the indicators evaluated, cord sTfR was the strongest determinant of cord Hb, and alone captured 41% of the total variance in cord Hb. Given the association between cord sTfR and maternal sTfR at mid-gestation, maternal sTfR may be a useful predictor of low cord Hb at birth. Unlike observations made in older infants and adults, a significant inverse association was found between cord SF and Hb. Nearly 1/4 of neonates with the highest SF had anemia, whereas anemia was not found in infants below the 10th percentile of the SF distribution. The lack of anemic neonates in the low SF group could be explained by a preferential use of Fe in support of erythropoiesis. However, the increased risk of anemia in neonates with elevated SF was unexpected and was not driven by folate or vitamin B12 deficiencies or by inflammation as assessed using IL-6 or CRP. Since multiple birth neonates are a high-risk study population, additional normative data are needed in term, singleton neonates to determine whether this is a consequence of other factor or unique to our higher risk neonatal cohort.
This study has several limitations. There are few normative data on Fe status in neonates to use for comparison purposes. Moreover, multiple assays are available for the Fe indicators evaluated and most are not standardized, limiting comparisons between studies. Secondly, we did not measure erythroferrone as there were no validated human assays for this hormone at the time the study was undertaken. This hormone is known to be stimulated by EPO and mediate hepcidin suppression.40 Although we studied a relatively large cohort of multiple birth neonates, our sample size was reduced when analyses were stratified, lowering power to detect significant associations. Finally, although IL-6 and CRP are two standardly utilized inflammatory markers, the presence of inflammation could not be ruled out and normative cord blood data on these markers are limited.
In conclusion, neonates born to women carrying multiple fetuses had a greater risk of anemia than has been reported among term singletons. Hepcidin was present at birth, in nearly all neonates, was significantly associated with the cord Fe status highlighting the ability of the fetus to regulate its Fe status in response to its intrauterine Fe environment. Increased time in utero from 25 to 38 wks did not reduce the risk of anemia in multiple birth neonates or lead to an increase in Fe status for the majority of Fe status indicators evaluated. Multiple birth neonates born to women who were obese prior to pregnancy, or to those that smoked during pregnancy had a significantly higher risk of anemia at birth. Additional screening practices for Fe status at birth are warranted in these groups. Given the higher risk of anemia noted, further studies are needed to identify maternal interventions that best support fetal Fe requirements in this higher risk neonatal population.
References
Hamilton, B., Marin, J. A., Osterman, J. K., Curtin, S. C. & Mathews, T. J. Births: final data for 2014. Natl Vital. Stat. Rep. 64, 1–63 (2015).
Goodnight, W. & Newman, R. Optimal nutrition for improved twin pregnancy outcome. Obstet. Gynecol. 114, 1121–1134 (2009).
Siddappa, A. et al. Iron deficiency alters auditory recognition memory in newborn infants of diabetic mothers. Pediatr. Res. 55, 1034–1041 (2004).
Murphy, J., O’Riordan, J., Newcombe, R. G., Coles, E. C. & Pearson, J. F. Relation of haemoglobin levels in first and second trimester to outcome of pregnancy. Lancet 1, 992–995 (1986).
Singal, P. N., Tyagl, M., Kumar, A., Dash, D. & Shankar, R. Fetal growth in maternal anemia. J. Trop. Pediatr. 43, 89–92 (1997).
Allen, L. Anemia and iron deficiency: effects on pregnancy outcome. Am. J. Clin. Nutr. 71, 1280s–1284ss (2000).
Rao, R. & Georgieff, M. K. Iron in fetal and neonatal nutrition. Semin. Fetal Neonatal Med. 12, 54–63 (2007).
Bothwell, T. Iron requirements in pregnancy and strategies to meet them. Am. J. Clin. Nutr. 72, 257S–264SS (2000).
Zamora, T., Guiang, S. F., Widness, J. A. & Georgieff, M. K. Iron is prioritized to red blood cells over the brain in phlebotomized anemic newborn lambs. Transl. Investig. 79, 922–928 (2016).
Baker, R. & Greer, F. R. Diagnosis and prevention of iron deficiency and iron deficiency anemia in infants and young children (0-3 years of age). Pediatrics 104, 119 (2010).
American Congress of Obstetricians and Gynecologists. Practice bulletin number 95—anemia in pregnancy. Obstetr. Gynecol. 112, 201–207 (2008).
Ru, Y. et al. Iron deficiency and anemia are prevalent in women with multiple gestations. Am. J. Clin. Nutr. 104, 1052–1060 (2016).
Steinl G., et al. Umbilical cord coiling in high-risk pregnancies: association with determinants of adverse birth outcomes and irons status. Pediatr. Dev. Pathol. 2018 :1093526618770318. doi: 10.1177/1093526618770318 (2017)
Institute of Medicine. Weight Gain During Pregnancy: Reexamining the Guidelines (National Academy of Sciences Press, Washington, DC, 2009).
The American Congress of Obestetricians and Gynecologists. Definition of term pregnancy. Committee Opinion No. 579. Obstet. Gynecol. 122, 1139–1140 (2013).
Lubchenco, L., Hansman, C., Dressler, M. & Boyd, E. Intrauterine growth as estimated from liverborn birth-weight data at 24 to 42 weeks of gestation. Pedatrics 32, 793–800 (1963).
Fenton, T. & Kim, J. H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 13, 1–3 (2013).
Miller, J., Chauhan, S. P. & Abuhamad, A. Z. Discordant twins: diagnosis, evaluation and management. Am. J. Obstet. Gynecol. 206, 10–20 (2012).
Orkin, S. et al. Nathan and Oski’s Hematology of Infancy and Childhood 7th edn, 33–53 (Sauders Elsevier, Philadelphia, PA, 2009).
Pfeiffer, C., Caudill, S. P., Gunter, E. W., Osterloh, J. & Sampson, E. J. Biochemical indicators of B vitamin status in the US population after folic acid fortification: results from the National Health and Nutrition Examination Survey 1999-2000. Am. J. Clin. Nutr. 82, 442–450 (2005).
Jopling, J., Henry, E., Wiedmeier, S. E. & Christensen, R. D. Reference ranges for hematocrit and blood hemoglobin concentration during the neonatal period: data from a multihospital health care system. Pediatrics 123, e333–e337 (2009).
Centers for Disease Control and Prevention. Iron deficiency—United States, 1999-2000. Morb. Mortal. Wkly. Rep. 51, 897–899 (2002).
Sandovici, I., Hoelle, K., Angiolini, E. & Constancia, M. Placental adaptations to the maternal–fetal environment: implications for fetal growth and developmental programming. Reprod. Biomed. Online 25, 68–89 (2012).
Socol, M. L., Tamura, R. K., Sabbangha, R. E., Chen, T. & Vaisrub, N. Diminished biparietal diameter and abdominal circumference growth in twins. Obstet. Gynecol. 64, 235–238 (1984).
Hall, J. G. Twinning. Lancet 362, 735–743 (2003).
Lackmann, G., Schnieder, C. & Bohner, J. Gestational age-dependent reference values for iron and selected proteins of iron metabolism in serum of premature human neonates. Biol. Neonate 74, 208–213 (1998).
Halliday, H., Lappin, T. R. & McClure, G. Iron status of the preterm infant during the first year of life. Biol. Neonate 45, 228–235 (1984).
Cao, C. et al. Prepregnancy body mass index and gestational weight gain have no negative impact on maternal or neonatal iron status. Reprod. Sci. 23, 613–622 (2016).
Wallace, J. M. Nutrient partitioning during pregnancy: adverse gestational outcome in overnourished adolescent dams. Proc. Nutr. Soc. 59, 107–117 (2000).
Wallace, J. M., Aitken, R. P. & Cheyne, M. A. Nutrient partitioning and fetal growth in rapidly growing adolescent ewes. J. Reprod. Fertil. 107, 183–190 (1996).
Philips, A. et al. Neonatal iron status is impaired by maternal obesity and excessive weight gain during pregnancy. J. Perinatol. 34, 513–518 (2014).
Jones, A. et al. Maternal obesity during pregnancy is negatively associated with maternal and neonatal iron status. Eur. J. Clin. Nutr. 70, 918–924 (2016).
Pateva, I. et al. Effect of maternal cigarette smoking on newborn iron stores. Clin. Res Trials 1, 4–7 (2015).
Chelchowska, M. et al. The effect of tobacco smoking during pregnancy on concentration of pro-hepcidin and some parameters of iron metabolism in matched-maternal cord pairs. Przegl Lek. 65, 474–478 (2008).
Tong, V. et al. Trends in smoking before, during, and after pregnancy—pregnancy risk assessment monitoring system, United States, 40 sites, 2000-2010. Morb. Mortal. Wkly. Rep. 62, 1–19 (2013).
Rehu, M. et al. Maternal serum hepcidin is low at term and independent of cord blood iron status. Eur. J. Haematol. 85, 345–352 (2010).
Lee, S. et al. Prevalence of anemia and associations between neonatal iron status hepcidin, and maternal iron status among neonates born to pregnant adolescents. Pediatr. Res 79, 42–48 (2016).
Kulik-Rechberger, B., Kosciesza, A., Szponar, E. & Domosud, J. Hepcidin and iron status in pregnant women and full-term newborns in first days of life. Ginekol. Pol. 87, 288–292 (2016).
Siddappa, A., Rao, R., Long, J. D., Widness, J. A. & Georgieff, M. K. The assessment of newborn iron stores at births: a review of the literature and standards for ferritin concentrations. Neonatology 92, 73–82 (2007).
Kautz, L. et al. Erythroferrone contributes to hepcidin suppression and iron overload in a mouse model of β-thalassemia. Blood 126, 2031–2037 (2015).
Acknowledgements
This study was funded by the Gerber Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ru, Y., Pressman, E.K., Guillet, R. et al. Predictors of anemia and iron status at birth in neonates born to women carrying multiple fetuses. Pediatr Res 84, 199–204 (2018). https://doi.org/10.1038/s41390-018-0044-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-018-0044-6
This article is cited by
-
Control variables of serum ferritin concentrations in hospitalized newborn infants: an observational study
Scientific Reports (2023)
-
Prevalence and associated factors of anemia among full-term newborn babies at University of Gondar comprehensive specialized hospital, Northwest Ethiopia: a cross-sectional study
Italian Journal of Pediatrics (2020)