Abstract
Background
children who undergo CPB operations are at an elevated risk of infection due to immunosuppression. This study aims to investigate the association between lymphopenia following CPB and early postoperative infection in children.
Methods
A retrospective analysis including 41 children under 2 years old underwent CPB. Among them, 9 subjects had an early postoperative infection, and 32 subjects were period-matched without infection. Inflammatory cytokines, serum CRP and PCT values were measured in plasma, additionally, circulating total leucocyte and lymphocyte subpopulations were counted.
Results
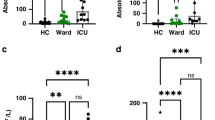
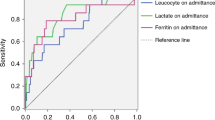
Infected subjects exhibited significantly higher levels of inflammatory cytokines, including IL-6, IL-8, IL-10, IL-1β and TNF-α, than non-infected subjects after CPB. Additionally, lower absolute number of lymphocyte and their subpopulations CD3+ T cells, CD4+ T-helper cells and CD8+cytotoxic T-cells, were observed in infected subjects. The impairment of T-cells Immune was found to be associated with higher levels of inflammatory cytokines IL-10. The ROC demonstrated that the absolute number of CD3+ T-cells <1934/ul, CD4+ T helper cells <1203/ul and CD8+cytotoxic T-cells <327/ul were associated with early postoperative infection.
Conclusion
Higher levels of inflammatory cytokines resulted in T-cells lymphopenia after CPB, which significantly increasing the risk of postoperative infection in infants and young children.
Impact
-
Infection complications after cardiopulmonary bypass (CPB) in pediatric CHD patients are serious issues, identifing the infection from after CPB remains a challenging.
-
CPB can release numerous inflammatory cytokines associated with T cells lymphopenia, which increases the risk of postoperative infection after surgery.
-
Monitoring T cells lymphopenia maybe more beneficial to predict early postoperative infection than C-reactive protein and procalcitonin.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Fowler, V. G. et al. Clinical predictors of major infections after cardiac surgery. Circulation 112, I358–I365 (2005).
Grisaru‐Soen, G. et al. Nosocomial infections in pediatric cardiovascular surgery patients: a 4‐ year survey. Pediatr. Crit. Care Med 10, 202–206 (2009).
Taylor, R. S. & Shekerdemian, L. S. Avoidance of hospital‐acquired infections in pediatric cardiac surgical patients. Pediatr. Crit. Care Med 17, S279–S286 (2016).
Wang Y. C., Wu H. Y., Luo C. Y., Lin T. W. Cardiopulmonary bypass time predicts early postoperative enterobacteriaceas bloodstream infection. Ann Thorac Surg. 107, 1333–1341 (2019).
Bronicki, R. A. & Hall, M. Cardiopulmonary bypass-induced inflammatory response: pathophysiology and treatment. Pediatr. Crit. Care Med. 17, S272–S278. (2016).
Ward, N. S., Casserly, B. & Ayala, A. The compensatory anti-inflammatory response syndrome (CARS) in critically ill patients. Clin. Chest Med. 29, 617–625 (2008).
Liu, C. H., Huang, Z. H., Huang, S. C. & Jou, T. S. Endocytosis of peroxiredoxin 1 links sterile inflammation to immunoparalysis in pediatric patients following cardiopulmonary bypass. Redox Biol. 46, 102086 (2021).
Habermehl, P. et al. Changes in lymphocyte subsets after cardiac surgery in children. Eur. J. Pediatr. 162, 15–21 (2003).
Engelman, R. R. et al. The Society of Thoracic Surgeons practice guideline series: Antibiotic prophylaxis in cardiac surgery, part II: Antibiotic choice. Ann. Thorac. Surg. 83, 1569–1576 (2007).
Warren, O. J. et al. The inflammatory response to cardiopulmonary bypass: Part 1—Mechanisms of pathogenesis. J. Cardiothorac. Vasc. Anesth. 23, 223–231 (2009).
Li, Y. P. et al. The compromised inflammatory response to bacterial components after pediatric cardiac surgery is associated with cardiopulmonary bypass–suppressed Toll-like receptor signal transduction pathways. J. Crit. Care 29, 312.e7–13 (2014).
Suleiman, M. S., Zacharowski, K. & Angelina, G. D. Inflammatory response and cardioprotection during open heart surgery; the importance of anaesthetics. Br. J. Pharm. 153, 21–33. 2 (2008).
Laffey, J. G., Boylan, J. F. & Cheng, D. C. The systemic inflammatory response to cardiac surgery: implications for the anesthesi- ologist. Anesthesiology 97, 215–252 (2002).
Tárnok, A. & Schneider, P. Pediatric cardiac surgery with cardiopulmonary bypass: pathways contributing to transient systemic immune suppression. Shock 16, 24–32 (2001).
Martin, M. D., Badovinac, V. P. & Griffith, T. S. CD4 T. Cell responses and the sepsis induced immunoparalysis state. Front Immunol. 11, 1364 (2020).
Allen, M. L. et al. Early postoperative monocyte deactivation predicts systemic inflammation and prolonged stay in pediatric cardiac intensive care. Crit. Care Med. 30, 1140–1145 (2002).
Cornell, T. T. et al. Clinical implications and molecular mechanisms of immunoparalysis after cardiopulmonary bypass. J. Thorac. Cardiovasc. Surg. 143, 1160–1166 (2012).
Allen, M. L. et al. Interleukin-10 and its role in clinical immunoparalysis following pediatric cardiac surgery. Crit. Care Med 34, 2658–2665 (2006).
Claeys, R. et al. Plasma procalcitonin and C-reactive protein in acute septic shock: Clinical and biological correlates. Crit. Care Med 30, 757–776 (2002).
McMaster, P. et al. Procalcitonin versus C-reactive protein and immature-to-total neutrophil ratio as markers of infection after cardiopulmonary bypass in children. Pediatr. Crit. Care Med 10, 217–221 (2009).
Silvetti, S. et al. Procalcitonin and early postoperative infection after pediatric cardiopulmonary bypass surgery. J. Cardiothorac. Vasc. Anesth. 35, 3688–3693 (2021 Dec).
Levy, I. et al. Nosocomial infections after cardiac surgery in infants and children: incidence and risk factors. J. Hosp. Infect. 53, 111–116 (2003).
Frazier, W. J. & Hall, M. W. Immunoparalysis and adverse outcomes from critical illness. Pediatr. Clin. 55, 647–668 (2008).
Acknowledgements
We thank all the members at the Department of pediatric cardiology, Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine for supporting.
Funding
This work was supported by Xinhua Hospital&Shanghai Jiao Tong University Joint Project (Grant number: 21XJMR04).
Author information
Authors and Affiliations
Contributions
W.L. was involved in gathering data, formal analysis and writing original draft, J.H. conceived the study and revised manuscript, H.W., W.S. and J.X. supported gathering data, ongxuan Peng and W.L. contributed to analyzing and interpreting data, Y.L., K.B. and S.C. revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
This work was approved by the Xinhua Hospital Ethics Committee (approval number: XHEC-QT-2021-042). All procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975. Informed consent was not required in the present study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, WJ., Peng, YX., Zhao, LQ. et al. T-cell lymphopenia is associated with an increased infecting risk in children after cardiopulmonary bypass. Pediatr Res 95, 227–232 (2024). https://doi.org/10.1038/s41390-023-02765-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02765-1