Abstract
Background
To characterize neurodevelopmental abnormalities in children up to 36 months of age with congenital Zika virus exposure.
Methods
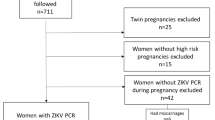
From the U.S. Zika Pregnancy and Infant Registry, a national surveillance system to monitor pregnancies with laboratory evidence of Zika virus infection, pregnancy outcomes and presence of Zika associated birth defects (ZBD) were reported among infants with available information. Neurologic sequelae and developmental delay were reported among children with ≥1 follow-up exam after 14 days of age or with ≥1 visit with development reported, respectively.
Results
Among 2248 infants, 10.1% were born preterm, and 10.5% were small-for-gestational age. Overall, 122 (5.4%) had any ZBD; 91.8% of infants had brain abnormalities or microcephaly, 23.0% had eye abnormalities, and 14.8% had both. Of 1881 children ≥1 follow-up exam reported, neurologic sequelae were more common among children with ZBD (44.6%) vs. without ZBD (1.5%). Of children with ≥1 visit with development reported, 46.8% (51/109) of children with ZBD and 7.4% (129/1739) of children without ZBD had confirmed or possible developmental delay.
Conclusion
Understanding the prevalence of developmental delays and healthcare needs of children with congenital Zika virus exposure can inform health systems and planning to ensure services are available for affected families.
Impact
-
We characterize pregnancy and infant outcomes and describe neurodevelopmental abnormalities up to 36 months of age by presence of Zika associated birth defects (ZBD).
-
Neurologic sequelae and developmental delays were common among children with ZBD.
-
Children with ZBD had increased frequency of neurologic sequelae and developmental delay compared to children without ZBD.
-
Longitudinal follow-up of infants with Zika virus exposure in utero is important to characterize neurodevelopmental delay not apparent in early infancy, but logistically challenging in surveillance models.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
These data are collected under relevant provisions of the Public Health Service Act and are protected at CDC by an Assurance of Confidentiality (Section 308(d) of the Public Health Service Act, 42 U.S.C. §242 m(d)) (https://www.cdc.gov/od/science/integrity/confidentiality/), which prohibits use or disclosure of any identifiable or potentially identifiable information collected under the Assurance for purposes other than those set out in the Assurance. Requests for access will be considered on a case-by-case basis, and inquiries should be directed to setnet@cdc.gov.
References
Wheeler, A. C. Development of infants with congenital Zika syndrome: What do we know and what can we expect? Pediatrics 141, S154–s60 (2018).
Reynolds, M. R. et al. Vital signs: Update on Zika virus-associated birth defects and evaluation of all U.S. infants with congenital Zika virus exposure—U.S. Zika pregnancy registry, 2016. MMWR Morb. Mortal. Wkly. Rep. 66, 366–73 (2017).
Honein, M. A. et al. Birth defects among fetuses and infants of US women with evidence of possible Zika virus infection during pregnancy. JAMA 317, 59–68 (2017).
Rice, M. E. et al. Vital signs: Zika-associated birth defects and neurodevelopmental abnormalities possibly associated with congenital Zika virus infection—U.S. territories and freely associated states, 2018. MMWR Morb. Mortal. Wkly. Rep. 67, 858–67 (2018).
Alves, L. V., Paredes, C. E., Silva, G. C., Mello, J. G. & Alves, J. G. Neurodevelopment of 24 children born in Brazil with congenital Zika syndrome in 2015: a case series study. BMJ Open 8, e021304 (2018).
Faical, A. V. et al. Neurodevelopmental delay in normocephalic children with in utero exposure to Zika virus. BMJ Paediatr. Open 3, e000486 (2019).
Lopes Moreira, M. E. et al. Neurodevelopment in infants exposed to Zika virus in utero. N. Engl. J. Med 379, 2377–2379 (2018).
Stringer, E. M. et al. Neurodevelopmental outcomes of children following in utero exposure to Zika in Nicaragua. Clin. Infect. Dis. 72, e146–e53 (2021).
Mercado-Reyes, M. et al. Pregnancy, birth, infant, and early childhood neurodevelopmental outcomes among a cohort of women with symptoms of Zika virus disease during pregnancy in three surveillance sites, project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016–2018. Trop. Med. Infect. Dis. 6, 183 (2021).
Marbán-Castro, E. V. G. L. et al. Neurodevelopment in normocephalic children exposed to Zika virus in utero with no observable defects at birth: A systematic review with meta-analysis. Int J. Environ. Res Public Health 19, 7319 (2022).
Mulkey, S. B. et al. Neurodevelopmental abnormalities in children with in utero Zika virus exposure without congenital Zika syndrome. JAMA Pediatr. 174, 269–276 (2020).
Nielsen-Saines, K. et al. Delayed childhood neurodevelopment and neurosensory alterations in the second year of life in a prospective cohort of ZIKV-exposed children. Nat. Med. 25, 1213–1217 (2019).
Roth, N. M. et al. Zika-associated birth defects reported in pregnancies with laboratory evidence of confirmed or possible Zika virus infection—U.S. Zika pregnancy and infant registry, December 1, 2015-March 31, 2018. MMWR Morb. Mortal. Wkly. report. 71, 73–79 (2022).
Villar, J. et al. International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st). International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 384, 857–868 (2014).
Paixao, E. S. et al. Mortality from congenital Zika syndrome—nationwide cohort study in Brazil. N. Engl. J. Med 386, 757–67 (2022).
Olson, S. M. et al. Updated baseline prevalence of birth defects potentially related to Zika virus infection. Birth Defects Res. 111, 938–40 (2019).
Adebanjo, T. et al. Update: Interim guidance for the diagnosis, evaluation, and management of infants with possible congenital Zika virus infection—United States, October 2017. MMWR Morb. Mortal. Wkly. Rep. 66, 1089–99 (2017).
Hoyert, D. L. & Gregory, E. C. W. Cause-of-death data from the fetal death file, 2015–2017. Natl. Vital-. Stat. Rep. 69, 1–20 (2020).
Hoen, B. et al. Pregnancy outcomes after ZIKV infection in French territories in the Americas. N. Engl. J. Med 378, 985–94 (2018).
Martin J. A., Hamilton B. E., Osterman M. J. K. Births in the United States, 2020. NCHS Data Brief. 2021; 1–8.
Martin J. A., Hamilton B. E., Osterman M. J. K. Births in the United States, 2015. NCHS Data Brief. 2016; (no 258): 1–8.
Martin J. A., Hamilton B. E., Osterman M. J. K. Births in the United States, 2016. NCHS Data Brief. 2017; (no 287): 1–8.
Martin J. A., Hamilton B. E., Osterman M. J. K. Births in the United States, 2017. NCHS Data Brief. 2018; (no 318): 1–8.
Martin J. A., Hamilton B. E., Osterman M. J. K. Births in the United States, 2018. NCHS Data Brief. 2019; (no 346): 1–8.
Cooper, H. J. M. et al. Maternal Zika virus infection. Obstet. Gynecol. 134, 1197–204 (2019).
Satterfield-Nash, A. et al. Health and development at age 19–24 months of 19 children who were born with microcephaly and laboratory evidence of congenital Zika virus infection during the 2015 Zika virus outbreak—Brazil, 2017. MMWR Morb. Mortal. Wkly. Rep. 66, 1347–1351 (2017).
Daza, M. et al. Clinical and neurodevelopmental outcomes based on brain imaging studies in a Colombian cohort of children with probable antenatal Zika virus exposure. Birth Defects Res. 113, 1299–312 (2021).
Bergman, K., Forestieri, N. E., Di Bona, V. L., Grosse, S. D. & Moore, C. A. Medicaid healthcare expenditures for infants with birth defects potentially related to Zika virus infection in North Carolina, 2011–2016. Birth Defects Res. 114, 80–89 (2022).
Black L. I., Vahratian A. & Hoffman H. J. Communication disorders and use of intervention services among children aged 3–17 years: United States, 2012. NCHS Data Brief. 2015; (205): 1-8.
CDC. Learn the Signs. Act Early. 2021 [updated February 18, 2021]. Available from: https://www.cdc.gov/ncbddd/actearly/index.html.
Lipkin, P. H. et al. Trends in pediatricians’ developmental screening: Pediatrics 145, 2002–2016 (2020).
Funding
CDC provided funding support and technical assistance to all U.S. states, territories, and freely associated states that reported cases to the U.S. Zika Pregnancy and Infant Registry (USZPIR) through the Epidemiology and Laboratory Capacity for Prevention and Control of Emerging Infectious Diseases (ELC) cooperative agreement (https://www.cdc.gov/ncezid/dpei/epidemiology-laboratory-capacity.html) and to selected jurisdictions through the Zika Local Health Department Initiative (https://www.cdc.gov/pregnancy/zika/research/lhdi.html).
Author information
Authors and Affiliations
Contributions
V.N., K.W., D.C., N.R., M.R., C.C., V.T. conceptualized the study; K.W., V.T., took responsibility for the integrity of the study; M.R., A.A., E.L., A.E., S.S., S.S., N.L., M.A., P.L., S.K., S.B., L.L., K.S., M.G., R.B., S.K., U.H., A.L., M.C., T.W., J.T., N.M., N.A.B., C.S., J.F., S.H., A.N., L.I., S.A., E.P., E.S., D.R., M.M., B.S., E.L., L.D., D.C., P.R., E.F., M.M., K.S., A.C., V.L., S.B., L.O., L.C., L.R. coauthors conducted the data collection, data quality checks, are reported data to CDC; S.G.C., C.A.M., K.W., N.R., K.A., S.B., R.D., C.B. participated in the clinical review to determine whether pregnancies met surveillance case definition; V.N., D.C., N.R. conducted the data analysis and replication; V.N., D.C., K.W., N.R., S.B., V.T. participated in drafting the manuscript; all authors contributed to reviewing and revising the manuscript’s content and approving the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
All authors have no conflicts of interest to disclose. The findings and conclusions in this article are those of the authors and do not necessarily represent the views or opinions of the California Department of Public Health or the California Health and Human Services Agency nor the official position of the Centers for Disease Control and Prevention.
Patient consent
Patient consent was not required as this activity was conducted as part of public health surveillance and deemed not research at CDC, thus exempt from IRB review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations
Supplementary Information
Rights and permissions
About this article
Cite this article
Neelam, V., Woodworth, K.R., Chang, D.J. et al. Outcomes up to age 36 months after congenital Zika virus infection—U.S. states. Pediatr Res 95, 558–565 (2024). https://doi.org/10.1038/s41390-023-02787-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02787-9
This article is cited by
-
Trends in prenatal and pediatric viral infections, and the impact of climate change
Pediatric Research (2024)