Abstract
In the last few years, current evidence has supported the use of point-of-care ultrasound (POCUS) for a number of diagnostic and procedural applications. Considering the valuable information that POCUS can give, we propose a standardized protocol for the management of neonates with a congenital diaphragmatic hernia (CDH-POCUS protocol) in the neonatal intensive care unit. Indeed, POCUS could be a valid tool for the neonatologist through the evaluation of 1) cardiac function and pulmonary hypertension; 2) lung volumes, postoperative pleural effusion or pneumothorax; 3) splanchnic and renal perfusion, malrotations, and/or signs of necrotizing enterocolitis; 4) cerebral perfusion and eventual brain lesions that could contribute to neurodevelopmental impairment. In this article, we discuss the state-of-the-art in neonatal POCUS for which concerns congenital diaphragmatic hernia (CDH), and we provide suggestions to improve its use.
Impact
-
This review shows how point-of-care ultrasound (POCUS) could be a valid tool for managing neonates with congenital diaphragmatic hernia (CDH) after birth.
-
Our manuscript underscores the importance of standardized protocols in neonates with CDH. Beyond the well-known role of echocardiography, ultrasound of lungs, splanchnic organs, and brain can be useful.
-
The use of POCUS should be encouraged to improve ventilation strategies, systemic perfusion, and enteral feeding, and to intercept any early signs related to future neurodevelopmental impairment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Morini, F., Lally, P. A., Lally, K. P. & Bagolan, P. The Congenital Diaphragmatic Hernia Study Group Registry. Eur. J. Pediatr. Surg. 25, 488–496 (2015).
Gupta, V. S. & Harting, M. T. Congenital diaphragmatic hernia-associated pulmonary hypertension. Semin. Perinatol. 44, 151167 (2020).
Singh, Y. et al. International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit. Care. 24, 1–16 (2020).
Montalva, L., Lauriti, G. & Zani, A. Congenital heart disease associated with congenital diaphragmatic hernia: a systematic review on incidence, prenatal diagnosis, management, and outcomes. J. Pediatr. Surg. 54, 909–919 (2019).
Patel, N. et al. Ventricular Dysfunction Is a Critical Determinant of Mortality in Congenital Diaphragmatic Hernia. Am. J. Respir. Crit. Care. Med. 200, 1522–1530 (2019).
Patel, N. & Kipfmueller, F. Cardiac dysfunction in congenital diaphragmatic hernia: Pathophysiology, clinical assessment, and management. Semin. Pediatr. Surg. 26, 154–158 (2017).
Lai, W. W. et al. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 19, 1413–1430 (2006).
Mertens, L. et al. Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Eur. J. Echocardiogr. 12, 715–736 (2011).
Abman, S. H. et al. Pediatric Pulmonary Hypertension: Guidelines From the American Heart Association and American Thoracic Society. Circulation 132, 2037–2099 (2015).
Lakshminrusimha, S. et al. Milrinone in congenital diaphragmatic hernia - a randomized pilot trial: study protocol, review of literature and survey of current practices. Matern. Health, Neonatol. Perinatol. 3, 27 (2017).
Bialkowski, A., Moenkemeyer, F. & Patel, N. Intravenous sildenafil in the management of pulmonary hypertension associated with congenital diaphragmatic hernia. Eur. J. Pediatr. Surg. 25, 171–176 (2015).
Lawrence, K. M. et al. Use of prostaglandin E1 to treat pulmonary hypertension in congenital diaphragmatic hernia. J. Pediatr. Surg. 54, 55–59 (2019).
Capolupo, I. et al. Early vasopressin infusion improves oxygenation in infants with congenital diaphragmatic hernia. Front. Pediatr. 11, 1104728 (2023).
Acker, S. N., Kinsella, J. P., Abman, S. H. & Gien, J. Vasopressin improves hemodynamic status in infants with congenital diaphragmatic hernia. J. Pediatr. 165, 53–58.e1 (2014).
Singh, Y. Echocardiographic Evaluation of Hemodynamics in Neonates and Children. Front. Pediatr. 5, 201 (2017).
Tissot, C., Singh, Y. & Sekarski, N. Echocardiographic Evaluation of Ventricular Function-For the Neonatologist and Pediatric Intensivist. Front. Pediatr. 6, 79 (2018).
Evans, N. & Kluckow, M. Early determinants of right and left ventricular output in ventilated preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 74, F88–F94 (1996).
Rudski, L. G. et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 23, 685–688 (2010).
Koestenberger, M. et al. Systolic right ventricular function in preterm and term neonates: reference values of the tricuspid annular plane systolic excursion (TAPSE) in 258 patients and calculation of Z-score values. Neonatology 100, 85–92 (2011).
Levy, P. T. et al. Right ventricular function in preterm and term neonates: reference values for right ventricle areas and fractional area of change. J. Am. Soc. Echocardiogr. 28, 559–569 (2015).
Patel, N., Mills, J. F. & Cheung, M. M. H. Use of the myocardial performance index to assess right ventricular function in infants with pulmonary hypertension. Pediatr. Cardiol. 30, 133–137 (2009).
More, K., Soni, R. & Gupta, S. The role of bedside functional echocardiography in the assessment and management of pulmonary hypertension. Semin. Fetal Neonatal Med. 27, 101366 (2022).
Bo, B. et al. Ductus arteriosus flow predicts outcome in neonates with congenital diaphragmatic hernia. Pediatr. Pulmonol. 58, 1711–1718 (2023).
van Laere, D. et al. Application of NPE in the assessment of a patent ductus arteriosus. Pediatr. Res. 84, 46–56 (2018).
Musewe, N. N. et al. Validation of Doppler-derived pulmonary arterial pressure in patients with ductus arteriosus under different hemodynamic states. Circulation. 76, 1081–1091 (1987).
Revanna, G. K., Kunjunju, A. & Sehgal, A. Bronchopulmonary dysplasia associated pulmonary hypertension: Making the best use of bedside echocardiography. Prog Pediatr. Cardiol. 46, 39–43 (2017).
Kipfmueller, F. et al. Echocardiographic Assessment of Pulmonary Hypertension in Neonates with Congenital Diaphragmatic Hernia Using Pulmonary Artery Flow Characteristics. J. Clin. Med. 11, 3038 (2022).
Keller, R. L. et al. Congenital diaphragmatic hernia: endothelin-1, pulmonary hypertension, and disease severity. Am. J. Respir. Crit. Care Med. 182, 555–561 (2010).
Raimondi, F. et al. Point-of-care lung ultrasound in neonatology: classification into descriptive and functional applications. Pediatr. Res. 90, 524–531 (2021).
Musolino, A. M. et al. Ten Years of Pediatric Lung Ultrasound: A Narrative Review. Front. Physiol. 6, 721951 (2022).
Mehollin-Ray, A. R. Prenatal lung volumes in congenital diaphragmatic hernia and their effect on postnatal outcomes. Pediatr. Radiol. 52, 637–642 (2022).
Gomond-Le Goff, C. et al. Effect of Different Probes and Expertise on the Interpretation Reliability of Point-of-Care Lung Ultrasound. Chest 157, 924–931 (2020).
Ruoss, J. L., Bazacliu, C., Cacho, N. & De Luca, D. Lung Ultrasound in the Neonatal Intensive Care Unit: Does It Impact Clinical Care? Children (Basel) 8, 1098 (2021).
Brat, R. et al. Lung Ultrasonography Score to Evaluate Oxygenation and Surfactant Need in Neonates Treated with Continuous Positive Airway Pressure. JAMA Pediatr 169, e151797 (2015).
Corsini, I. et al. Lung ultrasound findings in congenital diaphragmatic hernia. Eur. J. Pediatr. 178, 491–495 (2019).
Maddaloni, C. et al. Lung Ultrasound Score in Neonates with Congenital Diaphragmatic Hernia (CDH-LUS): A Cross-Sectional Study. Diagnostics (Basel) 13, 898 (2023).
Patel, N., Massolo, A. C., Kraemer, U. S. & Kipfmueller, F. The heart in congenital diaphragmatic hernia: Knowns, unknowns, and future priorities. Front. Pediatr. 10, 890422 (2022).
Usui, N. et al. Pneumothoraces as a fatal complication of congenital diaphragmatic hernia in the era of gentle ventilation. Eur. J. Pediatr. Surg. 24, 31–38 (2014).
Rubalcava, N. et al. Neonatal pneumothorax in congenital diaphragmatic hernia: Be wary of high ventilatory pressures. World J. Pediatr. Surg 5, e000341 (2022).
Cattarossi, L., Copetti, R., Brusa, G. & Pintaldi, S. Lung Ultrasound Diagnostic Accuracy in Neonatal Pneumothorax. Can. Respir. J 2016, 6515069 (2016).
Kurepa, D., Zaghloul, N., Watkins, L. & Liu, J. Neonatal lung ultrasound exam guidelines. J. Perinatol 38, 11–22 (2018).
Liu, J. et al. Lung ultrasonography to diagnose pneumothorax of the newborn. Am J Emerg Med. 35, 1298–1302 (2017).
Shojaee, S. & Argento, A. C. Ultrasound-guided pleural access. Semin. Respir. Crit. Care Med. 35, 693–705 (2014).
Raimondi, F. et al. Lung Ultrasound for Diagnosing Pneumothorax in the Critically Ill Neonate. J Pediatr 175, 74–78.e1 (2016).
Casaccia, G. et al. Pleural effusion requiring drainage in congenital diaphragmatic hernia: incidence, aetiology and treatment. Pediatr. Surg. Int. 22, 585–588 (2006).
Hansell, L. et al. Lung ultrasound has greater accuracy than conventional respiratory assessment tools for the diagnosis of pleural effusion, lung consolidation and collapse: a systematic review. J Physiother 67, 41–48 (2021).
Schlager, A., Arps, K., Siddharthan, R. & Clifton, M. S. Tube Thoracostomy at the Time of Congenital Diaphragmatic Hernia Repair: Reassessing the Risks and Benefits. J. Laparoendosc. Adv. Surg. Tech. A. 27, 311–317 (2017).
Volpicelli, G. et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 38, 77–91 (2012).
Papacci, P. et al. Neonatal colour Doppler ultrasound study: Normal values of abdominal blood flow velocities in the neonate during the first month of life. Pediatr. Radiol. 39, 328–335 (2009).
Pracros, J. P. et al. Ultrasound diagnosis of midgut volvulus: the “whirlpool” sign. Pediatr. Radiol. 22, 18–20 (1992).
Guang, Y. et al. Early Doppler Ultrasound in the Superior Mesenteric Artery and the Prediction of Necrotizing Enterocolitis in Preterm Neonates. J Ultrasound Med. 38, 3283–3289 (2019).
Murphy, C., Baskind, S., Aladangady, N. & Banerjee, J. Measuring gut perfusion and blood flow in neonates using Ultrasound Doppler of the Superior Mesenteric Artery - a narrative review. Front. Pediatr. 11, 1154611 (2023).
Elsayed, Y. & Seshia, M. A new intestinal ultrasound integrated approach for the management of neonatal gut injury. Eur. J. Pediatr. 181, 1739–1749 (2022).
Faingold, R. et al. Necrotizing enterocolitis: Assessment of bowel viability with color doppler US. Radiology 235, 587–594 (2005).
Barczuk-Falęcka, M. et al. Hepatic Portal Venous Gas in Children Younger Than 2 Years Old - Radiological and Clinical Characteristics in Diseases Other Than Necrotizing Enterocolitis. Pol. J. Radiol. 82, 275–278 (2017).
Engel, C., Silva, C., Baker, K. & Goodman, T. R. Underutilized ultrasound applications in the neonatal intensive care unit. Ultrasound Q 28, 299–304 (2012).
Kiblawi, R. et al. Vena Cava Thrombosis after Congenital Diaphragmatic Hernia Repair: Multivariate Analysis of Potential Risk Factors. Eur. J. Pediatr. Surg. 32, 91–97 (2022).
Scott, J. E., Hunter, E. W., Lee, R. E. & Matthews, J. N. S. Ultrasound measurement of renal size in newborn infants. Arch. Dis. Child. 65, 361–364 (1990).
Rumack, C. & Levine, D. Diagnostic Ultrasound. 5th ed. (2018).
Karaoglanoglu, N., Turkyilmaz, A., Eroglu, A. & Alici, H. A. Right-sided Bochdalek hernia with intrathoracic kidney. Pediatr. Surg. Int. 22, 1029–1031 (2006).
Slovis, T. L., Bernstein, J. & Gruskin, A. Practical pediatric nephrology - Hyperechoic kidneys in the newborn and young infant. Pediatr. Nephrol. 43, 294–302 (1993).
Murat, A. et al. Renal resistive index in healthy children. Eur. J. Radiol. 53, 67–71 (2005).
Husain-Syed, F. et al. Doppler-Derived Renal Venous Stasis Index in the Prognosis of Right Heart Failure. J. Am. Heart Assoc. 8, e013584 (2019).
Qian, X., Zhen, J., Meng, Q., Li, L. & Yan, J. Intrarenal Doppler approaches in hemodynamics: A major application in critical care. Front. Physiol. 13, 1–9 (2022).
Miller, L. E., Stoller, J. Z. & Fraga, M. V. Point-of-care ultrasound in the neonatal ICU. Curr. Opin. Pediatr. 32, 216–227 (2020).
Dudink, J., Jeanne Steggerda, S., Horsch, S. & eurUS.brain group. State-of-the-art neonatal cerebral ultrasound: technique and reporting. Pediatr. Res 87, 3–12 (2020).
Danzer, E. & Hedrick, H. L. Neurodevelopmental and neurofunctional outcomes in children with congenital diaphragmatic hernia. Early Hum. Dev. 87, 625–632 (2011).
Danzer, E. & Kim, S. S. Neurodevelopmental outcome in congenital diaphragmatic hernia: Evaluation, predictors and outcome. World J. Clin. Pediatr 3, 30–36 (2014).
Danzer, E. et al. Longitudinal neurodevelopmental and neuromotor outcome in congenital diaphragmatic hernia patients in the first 3 years of life. J. Perinatol. 33, 893–898 (2013).
Peetsold, M. G. et al. The long-term follow-up of patients with a congenital diaphragmatic hernia: a broad spectrum of morbidity. Pediatr. Surg. Int. 25, 1–17 (2009).
Van der Veeken, L. et al. Prenatal cerebellar growth is altered in congenital diaphragmatic hernia on ultrasound. Prenat. Diagn. 42, 330–337 (2022).
Steggerda, S. J. & van Wezel-Meijler, G. Cranial ultrasonography of the immature cerebellum: Role and limitations. Semin. Fetal Neonatal Med. 21, 295–304 (2016).
Steggerda, S. J. et al. Cerebellar injury in preterm infants: incidence and findings on US and MR images. Radiology. 252, 190–199 (2009).
Limperopoulos, C. et al. Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation. 121, 26–33 (2010).
Masoller, N. et al. Severity of Fetal Brain Abnormalities in Congenital Heart Disease in Relation to the Main Expected Pattern of in utero Brain Blood Supply. Fetal Diagn. Ther. 39, 269–278 (2016).
Kosiv, K. A. et al. Fetal cerebrovascular impedance is reduced in left congenital diaphragmatic hernia. Ultrasound Obstet. Gynecol. 57, 386–391 (2021).
Larson, A. C. et al. The fetal lamb model of congenital diaphragmatic hernia shows altered cerebral perfusion using contrast enhanced ultrasound. J. Pediatr. Surg 57, 991–998 (2022).
Radhakrishnan, R. et al. Fetal brain morphometry on prenatal magnetic resonance imaging in congenital diaphragmatic hernia. Pediatr. Radiol. 49, 217–223 (2019).
Van Mieghem, T. et al. Fetal cerebral blood flow velocities in congenital diaphragmatic hernia. Ultrasound Obstet. Gynecol. 36, 452–457 (2010).
Elmfors, A. F. et al. Normal values of the resistivity index of the pericallosal artery with and without compression of the anterior fontanelle. Pediatr. Radiol. 49, 646–651 (2019).
Lucignani, M. et al. Morphometric analysis of brain in newborn with congenital diaphragmatic hernia. Brain Sci 11, 455 (2021).
Grover, T. R. et al. Central Line Utilization and Complications in Infants with Congenital Diaphragmatic Hernia. Am. J. Perinatol. 29, 1524–1532 (2022).
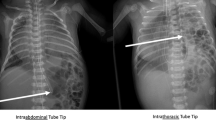
Dassios, T., Hickey, A., Krokidis, M. & Greenough, A. Congenital diaphragmatic hernia in newborn infants: Variable endotracheal tube and umbilical venous catheter positions. Early Hum. Dev. 128, 12–14 (2019).
D’Andrea, V. et al. Umbilical Venous Catheter Update: A Narrative Review Including Ultrasound and Training. Front. Pediatr. 9, 774705 (2021).
Fleming, S. E. & Kim, J. H. Ultrasound-guided umbilical catheter insertion in neonates. J. Perinatol. 31, 344–349 (2011).
Barone, G., D’Andrea, V., Vento, G. & Pittiruti, M. A Systematic Ultrasound Evaluation of the Diameter of Deep Veins in the Newborn: Results and Implications for Clinical Practice. Neonatology 115, 335–340 (2019).
Barone, G., Pittiruti, M. & D’Andrea, V. Ultrasound-guided catheter tip location in neonatal central venous access. Focus on well-defined protocols and proper ultrasound training. J. Pediatr. 247, 181 (2022).
Barone, G. et al. Neo-ECHOTIP: A structured protocol for ultrasound-based tip navigation and tip location during placement of central venous access devices in neonates. J. Vasc. Access. 23, 679–688 (2022).
Funding
This work was supported by the Italian Ministry of Health with “Current Research” funds.
Author information
Authors and Affiliations
Contributions
C.M., D.U.D.R., and F.Cal. conceptualized and designed the study, collected and interpreted data, carried out the initial analyses, and wrote the first and final drafts of the manuscript. S.R., F.P., L.M., S.C. and I.B. collected data from literature and provided significant edits to the manuscript. R.L. supervised ultrasound images acquisition and provided significant edits to the manuscript. A.C., F.Cam., P.T., I.C. and A.D. supervised data collection, critically reviewed the manuscript for important intellectual content. All authors participated to the writing of this paper, approved the final manuscript as submitted, and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maddaloni, C., De Rose, D.U., Ronci, S. et al. The role of point-of-care ultrasound in the management of neonates with congenital diaphragmatic hernia. Pediatr Res 95, 901–911 (2024). https://doi.org/10.1038/s41390-023-02889-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02889-4