Abstract
Since 2016, international research groups have focused on assessing outcomes of children with in utero Zika virus (ZIKV) exposure. While the more severe outcomes of congenital Zika syndrome (CZS) occur in up to 10% of children with antenatal exposure, early findings among ZIKV-exposed children without CZS ages 0–5 years suggest that they may also have differences in multiple domains of neurodevelopment. Thus, longitudinal follow-up of all children with antenatal ZIKV exposure has been recommended. This review presents a summary of neurodevelopmental phenotypes of infants and children following antenatal ZIKV exposure. We present a multidimensional framework to understand child neurodevelopment from an interdisciplinary and whole-child perspective (International Classification of Functioning, Disability and Health model) and multi-domain ZIKV Outcome Toolboxes. The toolboxes are for clinicians, researchers, child educators, and others to implement longitudinal multi-domain neurodevelopmental assessments between ages 0–12 years. Recent innovations in telehealth and neuroimaging can help evaluate outcomes in ZIKV exposed children. The objective is to describe the multiple facets of neurodevelopmental focused care that can support the health, function, and well-being of children with antenatal ZIKV exposure. The research and clinical follow-up strategies are applicable to ZIKV and other congenital infectious or environmental exposures that can impact child neurodevelopment.
Impact
-
International longitudinal cohort studies have revealed a range of differences in neurodevelopment among children with antenatal Zika virus (ZIKV) exposure.
-
A multidimensional and whole-child framework is necessary to understand the neurodevelopment of children with antenatal ZIKV exposure in relation to family life, community participation, and environment.
-
Multi-domain toolboxes that utilize parent questionnaires and child evaluations are presented. These toolboxes can be used internationally alongside telehealth, brain imaging, and other innovations to improve understanding of child outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Gilbert, R. K., Petersen, L. R., Honein, M. A., Moore, C. A. & Rasmussen, S. A. Zika virus as a cause of birth defects: were the teratogenic effects of Zika virus missed for decades? Birth Defects Res. 115, 265–274 (2023).
Reefhuis, J. et al. Projecting month of birth for at-risk infants after Zika virus disease outbreaks. Emerg. Infect. Dis. 22, 828–832 (2016).
Johansson, M. A., Mier-y-Teran-Romero, L., Reefhuis, J., Gilboa, S. M. & Hills, S. L. Zika and the risk of microcephaly. N. Engl. J. Med. 375, 1–4 (2016).
Focosi, D., Maggi, F. & Pistello, M. Zika virus: implications for public health. Clin. Infect. 63, 227–233 (2016).
Adebanjo, T. et al. Update: interim guidance for the diagnosis, evaluation and management of infants with possible congenital Zika virus infection—United States. Morb. Mortal. Wkly. Rep. 66, 1089–1099 (2017).
Honein, M. A. et al. US Zika Pregnancy Registry Collaboration. Birth defects among fetuses and infants of US women with evidence of possible Zika virus infection during pregnancy. JAMA 317, 59–68 (2017).
Aragao, M. F. V. V. et al. Nonmicrocephalic infants with congenital Zika syndrome suspected only after neuroimaging evaluation compared with those with microcephaly at birth and postnatally: how large is the Zika virus “iceberg”? Am. J. Neuroradiol. 38, 1427–1434 (2017).
Muller, W. J. & Mulkey, S. B. Lessons about early neurodevelopment in children exposed to ZIKV in utero. Nat. Med. 25, 1192–1193 (2019).
Mulkey, S. B. Head circumference as a measure of in utero Zika virus exposure and outcomes. JAMA Netw. Open. 3, e209461 (2020).
Moore, C. A. et al. Characterizing the pattern of anomalies in congenital Zika syndrome for pediatric clinicians. JAMA Pediatr. 171, 288–295 (2017).
Ventura, C. V. et al. Ophthalmological manifestations in congenital Zika syndrome in 469 Brazilian children. J. Aapos. 25, 158.e1–e8 (2021).
Maia, C. Q. et al. Epilepsy in children with congenital Zika syndrome: a systematic review and meta-analysis. Epilepsia 62, 1193–1207 (2021).
van der Linden, H. Jr et al. Epilepsy and EEG abnormalities in congenital Zika syndrome. J. Clin. Neurophysiol. 1, 248–252 (2022).
Suzuki, Y., Toribe, Y., Mogami, Y., Yanagihara, K. & Nishikawa, M. Epilepsy in patients with congenital cytomegalovirus infection. Brain Dev. 30, 420–424 (2008).
Carvalho, M. D. C. G. et al. Early epilepsy in children with Zika-related microcephaly in a cohort in Recife, Brazil: characteristics, electroencephalographic findings, and treatment response. Epilepsia 61, 509–518 (2020).
van der Linden, H. et al. Epilepsy profile in infants with congenital Zika virus infection. N. Engl. J. Med. 379, 891–892 (2018).
Godfred-Cato, S. et al. 2018 Zika health brigade: delivering critical health screening in the U.S. Virgin Islands. Trop. Med. Infect. Dis. 9, 168 (2020).
Antoniou, E. et al. Congenital Zika syndrome and disabilities of feeding and breastfeeding in early childhood: a systematic review. Viruses 15, 601 (2023).
Gabriela Lopes Gama, G. et al. The impact of COVID-19 pandemic and social distancing on motor function and growth of children with congenital Zika syndrome: a prospective cohort study. Dev. Neurorehabilit. 26, 123129 (2023).
Müller, W. I. M. et al. Effect of neurodevelopmental treatment in children with congenital Zika syndrome: a pilot study. J. Paediatr. Child Health 58, 2008–2015 (2022).
Paixao, E. S. et al. Mortality from congenital Zika syndrome—nationwide cohort study in Brazil. N. Engl. J. Med. 386, 757–767 (2022).
Blair, E., Langdon, K., McIntyre, S., Lawrence, D. & Watson, L. Survival and mortality in cerebral palsy: observations to the sixth decade from a data linkage study of a total population register and National Death Index. BMC Neurol. 19, 111 (2019).
Mulkey, S. B. et al. Neurodevelopmental abnormalities in Zika-exposed infants without congenital Zika syndrome. JAMA Pediatr. 174, 269–276 (2020).
Mulkey, S. B. et al. Preschool neurodevelopment in Zika virus-exposed children without congenital Zika syndrome. Pediatr. Res. 4, 178–184 (2023).
Mulkey, S. B. et al. Sequential neuroimaging of the fetus and newborn with in utero ZIKV exposure: US detects the majority of brain findings. JAMA Pediatr. 173, 52–59 (2019).
Nielsen-Saines, K. et al. Delayed childhood neurodevelopment and neurosensory alterations in the second year of life in a prospective cohort of ZIKV-exposed children. Nat. Med. 8, 1213–1217 (2019).
Marbán-Castro, E. et al. Neurodevelopment in normocephalic children exposed to Zika virus in utero with no observable defects at birth: a systematic review with meta-analysis. Int. J. Environ. Res. Public Health 19, 7319 (2022).
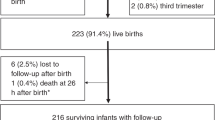
Mulkey, S. B. et al. Complexities of Zika diagnosis and evaluation in a United States congenital Zika program. Am. J. Trop. Med. Hyg. 104, 1–10 (2021).
The Functioning and Disability Reference Group, World Health Organization. The ICF: An Overview. Working paper. https://www.cdc.gov/nchs/data/icd/icfoverview_finalforwho10sept.pdf. (n.d.). Accessed 10 November 2023.
de Souza, L. C. M. R. et al. Characterizing disabilities in preschool aged children with congenital Zika virus syndrome with the ICF model. Viruses 14, 2108 (2022).
Alvarado-Domenech, L. I. et al. Early childhood neurodevelopmental outcomes in children with prenatal Zika virus exposure: a cohort study in Puerto Rico. J. Pediatr. 247, 38–45 (2022).
Mulkey, S. B. et al. Harnessing the power of telemedicine to accomplish international pediatric outcome research during the COVID-19 pandemic. J. Telemed. Telecare. 30, 388–392 (2024).
Peyton, C. et al. Validity of the Warner Initial Developmental Evaluation of Adaptive and Functional Skills (WIDEA-FS): a daily activity criterion checklist for infants and toddlers. Pediatr. Res. 90, 1052–1057 (2021).
Msall, M. E. Measuring functional skills in preschool children at risk for neurodevelopmental disabilities. Ment. Retard. Dev. Disabil. Res. Rev. 11, 263–273 (2005).
Bode, M. M. et al. Predictive validity of the Bayley, at 2 years for intelligence quotient at 4 years in preterm infants. J. Dev. Behav. Pediatr. 35, 570–575 (2014).
Spencer-Smith, M. M. et al. Bayley-III cognitive and language scales in preterm children. Pediatrics 135, e1258–e1265 (2015).
Hack, M. et al. Poor predictive validity of the Bayley Scales of Infant Development for cognitive function of extremely low birth weight children at school age. Pediatrics 116, 333–341 (2005).
O’Shea, T. M. et al. Accuracy of the Bayley-II mental development index at 2 years as a predictor of cognitive impairment at school age among children born extremely preterm. J. Perinatol. 38, 908–916 (2018).
de Wilde, L. H. et al. 2021 U.S. Virgin Islands Zika health brigade: providing recommended pediatric health screenings for children born to mothers with laboratory evidence of possible Zika virus infection during pregnancy. Birth Defects Res. 115, 572–577 (2023).
Mulkey, S. B. Use of telehealth methods to track infant neurodevelopment after in utero SARS-CoV-2 exposure. JAMA Netw. Open. 6, e237403 (2023).
Baumel, T. W. & Strawn, J. R. Neurobiology of treatment in pediatric anxiety disorders. Child Adolesc. Psychiatr. Clin. N. Am. 32, 589–600 (2023).
Shiohama, T. & Tsujimura, K. Quantitative structural brain magnetic resonance imaging analyses: methodological overview and application to Rett syndrome. Front Neurosci. 16, 835964 (2022).
Simonato, M. et al. Identification of clinically relevant biomarkers of epileptogenesis—a strategic roadmap. Nat. Rev. Neurol. 17, 231–242 (2021).
Eppes, C. et al. Testing for Zika virus infection in pregnancy: key concepts to deal with an emerging epidemic. Am. J. Obstet. Gynecol. 216, 209–225 (2017).
Honein, M. A. & Jamieson, D. Revealing the effects of Zika—detection of brain abnormalities and other disabilities associated with congenital infection. JAMA Pediatr. 173, 16–18 (2019).
Barkovich, M. et al. Challenges in pediatric neuroimaging. NeuroImage 185, 793–801 (2019).
Sanders Pereira Pinto, P. et al. Brain abnormalities on neuroimaging in children with congenital Zika syndrome in Salvador, Brazil, and its possible implications on neuropsychological development. Int. J. Dev. Neurosci. 80, 189–196 (2020).
Sanz Cortes, M. et al. Clinical assessment and brain findings in a cohort of mothers, fetuses and infants infected with ZIKA virus. Am. J. Obstet. Gynecol. 218, 440.e1–e36 (2018).
Daza, M. et al. Clinical and neurodevelopmental outcomes based on brain imaging studies in a Colombian cohort of children with probable antenatal Zika virus exposure. Birth Defects Res. 113, 1299–1312 (2021).
Pool, K.-L. et al. Association between neonatal neuroimaging and clinical outcomes in Zika-exposed infants from Rio de Janeiro, Brazil. JAMA Netw. Open. 2, e198124 (2019).
Schuler-Faccini, L. et al. Neurodevelopment in children exposed to Zika in utero: clinical and molecular aspects. Front. Genet. 13, 758715 (2022).
Yerys, B. E. et al. The FMRI success rate of children and adolescents: typical development, epilepsy, attention deficit/hyperactivity disorder, and autism spectrum disorders. Hum. Brain Mapp. 30, 3426–3435 (2009).
Sato, J. R. et al. A guide for the use of FNIRS in microcephaly associated to congenital Zika virus infection. Sci. Rep. 11, 19270 (2021).
Beauchaine, T. P., Constantino, J. & Hayden, E. P. Psychiatry and developmental psychopathology: unifying themes and future directions. Compr. Psychiatry 87, 143–152 (2018).
Bethell, C. D. Engaging families (and ourselves) in quality improvement: an optimistic and developmental perspective. Acad. Pediatr. 13, S9–S11 (2013).
World Health Organization. Psychosocial Support for Pregnant Women and for Families with Microcephaly and Other Neurological Complications in the Context of Zika Virus: Interim Guidance for Health-care Providers. Technical Document (2016).
Williams, N. A. et al. Anxiety and depression among caregivers of young children with Congenital Zika Syndrome in Brazil. Disabil. Rehabil. 43, 2100–2109 (2021).
Bethell, C., Kennedy, S., Martinez-Vidal, E. & Simpson, L. Payment for Progress: Investing to Catalyze Child and Family Well-Being Using Personalized and Integrated Strategies to Address Social and Emotional Determinants of Health. Report. https://academyhealth.org/sites/default/files/payment_for_progress_fullreport_nov2018.pdf. (2018).
Palfrey, J., Rosen-Reynoso, M., Ogilus, N. & Foley, S. Reducing Health Disparities for Hispanic Children with Special Health Care Needs. Report. https://cahmi.org/docs/default-source/resources/reducing-health-disparities-for-hispanic-children-with-special-healh-care-needs.pdf?sfvrsn=afe10988_0. (2013).
Bauer, S. C. & Msall, M. E. Optimizing neurodevelopmental outcomes after prematurity: lessons in neuroprotection and early intervention. Minerva Pediatr. 62, 485–497 (2010).
Falcão do Vale, P. R. L., Vitória Alves, D., da Cruz Amorim, R. & de Santana Carvalho, E. S. Rosette of care for children with zika congenital syndrome: caring attitudes of relatives. Esc. Anna Nery. 24, e20190268 (2020).
Lemmon, M. E. et al. Neonatal seizure registry. Family-centered care for children and families impacted by neonatal seizures: advice from parents. Pediatr. Neurol. 124, 26–32 (2021).
World Health Organization. WHO Toolkit for the Care and Support of People Affected by Complications Associated with Zika Virus (World Health Organization, 2017).
Lemmon, M. E. et al. The ALIGN framework: a parent-informed approach to prognostic communication for infants with neurologic conditions. Neurology 100, e800–e807 (2023).
Santos, D. B. C. D. et al. Sensitizing mothers of children with microcephaly in promoting the health of their children. Rev. Esc. Enferm. Usp. 53, e03491 (2019).
Tirado, V., Morales, M. S. A., Kinsman, J., Ekström, A. M. & Restrepo Jaramillo, B. N. Women’s reluctance for pregnancy: experiences and perceptions of Zika virus in Medellin, Colombia. Int. J. Gynaecol. Obstet. 148, 36–44 (2020).
Duttine, A. et al. Assessment of the feasibility of Juntos: a support programme for families of children affected by Congenital Zika Syndrome. Wellcome Open Res. 7, 77 (2022).
Kotzky, K. et al. Depressive symptoms and care demands among primary caregivers of young children with evidence of congenital Zika virus infection in Brazil. J. Dev. Behav. Pediatr. 40, 344–353 (2019).
Ornelas Pereira, I. et al. Parental stress in primary caregivers of children with evidence of congenital Zika virus infection in Northeastern Brazil. Matern. Child Health J. 25, 360–367 (2021).
Kuper, H. et al. The association of depression, anxiety, and stress with caring for a child with congenital Zika syndrome in Brazil; results of a cross-sectional study. PLoS Negl. Trop. Dis. 13, e0007768 (2019).
Carroll, C., Booth, A., Campbell, F. & Relton, C. What are the implications of Zika Virus for infant feeding? A synthesis of qualitative evidence concerning congenital Zika syndrome (CZS) and comparable conditions. PLoS Negl. Trop. Dis. 14, e0008731 (2020).
Laza-Vásquez, C., Briones-Vozmediano, E. & Gea-Sánchez, M. Caring for children with congenital Zika syndrome: the unmet needs of mothers in Southern Colombia. Glob. Public Health 17, 2752–2763 (2022).
Marbán-Castro, E. et al. “One feels anger to know there is no one to help us!”. Perceptions of mothers of children with Zika virus-associated microcephaly in Caribbean Colombia: a qualitative study. PLoS Negl. Trop. Dis. 16, e0010328 (2022).
Brooks, S. K., Weston, D. & Greenberg, N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health 189, 26–36 (2020).
Williams, M. E. et al. Positive and negative effects of the COVID-19 pandemic on families of young children in rural Colombia and implications for child outcome research. Child Care Health Dev. 49, 825–833 (2023).
Acknowledgements
We appreciate the families and their children who have participated in our research studies in the United States and in Colombia and experienced Zika virus firsthand or in their community. The ICF model was created in Spanish during a virtual interactive Zoom session with members of the Biomelab research team in Barranquilla, Colombia: Ana Cecilia Perez, Lorenzo Cervantes, Javier Restrepo, Ramiro Galindo, Jose Ospino, and Miguel Castillo. The ICF models were created in Spanish and translated by Regan Andringa-Seed, BA, a clinical research coordinator at Children’s National Hospital, Washington, DC.
Funding
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (grant number R01HD102445 [to S.B.M.]), the Thrasher Research Fund (to S.B.M.), the National Center for Advancing Translational Sciences (grant KL2TR001424 [to C.P.]), and the DC Intellectual and Developmental Disabilities Research Center (NICHD P50HD105328-01 [to M.M.B.]). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. S.B.M. has an additional contract with the US Centers for Disease Control and Prevention for work on Zika virus separate from this study and M.E.M. received additional funding from the Health Resources and Services Administration of the US Department of Health and Human Services under award UA6MC32492, the Life Course Intervention Research Network.
Author information
Authors and Affiliations
Contributions
Sarah B. Mulkey—conceptualization, obtained funding, literature review, writing initial draft, participated in development of ICF models, review of manuscript and editing, review and approval of final draft. Meagan E. Williams—literature review, writing initial draft, developed figures and tables, participated in development of ICF models, review of manuscript and editing, review and approval of final draft. Colleen Peyton—conceptualization, literature review, writing initial draft, participated in development of ICF models, review of manuscript and editing, review and approval of final draft. Margarita Arroyave-Wessel—writing initial draft, participated in development of ICF models, review of manuscript and editing, review and approval of final draft. Madison M. Berl—conceptualization, writing initial draft, review of manuscript and editing, review and approval of final draft. Carlos Cure—conceptualization, participated in development of ICF models, review of manuscript and editing, review and approval of final draft. Michael E. Msall—conceptualization, literature review, writing initial draft, participated in development of ICF models, review of manuscript and editing, review and approval of final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mulkey, S.B., Williams, M.E., Peyton, C. et al. Understanding the multidimensional neurodevelopmental outcomes in children after congenital Zika virus exposure. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03056-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03056-z