Abstract
Background
Shared decision-making (SDM) is recommended for prostate-specific antigen (PSA) testing but appears underutilized. This population-based study assessed the prevalence and determinants of SDM for PSA testing among US men.
Methods
We assessed PSA testing rates and SDM engagement in men aged 40 and older without prostate cancer history using the 2019 National Health Interview Survey. SDM was defined as discussing the advantages and disadvantages of PSA testing with a physician. We used multivariable logistic regression with machine learning to identify factors associated with lack of SDM.
Results
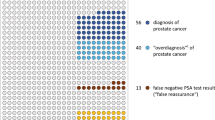
Among 9723 eligible participants (mean age 58 years), lifetime PSA testing prevalence was 45.9% and the 1-year testing incidence was 29.1%. Only 24.1% reported engaging in SDM with a physician, while 62.9% never discussed PSA testing. Younger age and lower education levels were the primary determinants of decreased SDM engagement. Men with less education engaged in SDM less than half as often as those with higher education levels across all age groups.
Conclusions
Societal guidelines recommend SDM for PSA testing. However, most men, regardless of age, have never engaged in SDM conversations with a healthcare provider about PSA testing, especially those with less education. More efforts are needed to improve patient-provider conversations about the potential benefits and harms of PSA testing.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The 2019 NHIS data are publicly available at https://www.cdc.gov/nchs/nhis/2019nhis.htm.
References
American Cancer Society. Key Statistics for Prostate Cancer. https://www.cancer.org/cancer/types/prostate-cancer/about/key-statistics.html. September 20, 2023.
Ilic D, Djulbegovic M, Jung JH, Hwang EC, Zhou Q, Cleves A, et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ. 2018;362:k3519.
Force USPST, Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB, et al. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018;319:1901–13.
Wei JT, Barocas D, Carlsson S, Coakley F, Eggener S, Etzioni R, et al. Early detection of prostate cancer: AUA/SUO guideline part I: prostate cancer screening. J Urol. 2023;210:46–53.
American Cancer Society. American Cancer Society Recommendations for Prostate Cancer Early Detection. https://www.cancer.org/cancer/types/prostate-cancer/detection-diagnosis-staging/acs-recommendations.html. September 20, 2023.
Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–7.
Han PK, Kobrin S, Breen N, Joseph DA, Li J, Frosch DL, et al. National evidence on the use of shared decision making in prostate-specific antigen screening. Ann Fam Med. 2013;11:306–14.
Leyva B, Persoskie A, Ottenbacher A, Hamilton JG, Allen JD, Kobrin SC, et al. Do men receive information required for shared decision making about PSA testing? Results from a national survey. J Cancer Edu. 2016;31:693–701.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Makarov DV, Chrouser K, Gore JL, Maranchie J, Nielsen ME, Saigal C, et al. AUA white paper on implementation of shared decision making into urological practice. Urol Pract. 2016;3:355–63.
Nohara Y, Matsumoto K, Soejima H, Nakashima N. Explanation of machine learning models using Shapley additive explanation and application for real data in hospital. Comput Methods Programs Biomed. 2022;214:106584.
Fong J, Venables M, D’Souza D, Maskerine C. Patient communication preferences for prostate cancer screening discussions: a scoping review. Ann Fam Med. 2023;21:448–55.
Pignone MP, Howard K, Brenner AT, Crutchfield TM, Hawley ST, Lewis CL, et al. Comparing 3 techniques for eliciting patient values for decision making about prostate-specific antigen screening: a randomized controlled trial. JAMA Intern Med. 2013;173:362–8.
De Oliveira GS Jr., Errea M, Bialek J, Kendall MC, McCarthy RJ. The impact of health literacy on shared decision making before elective surgery: a propensity matched case control analysis. BMC Health Serv Res. 2018;18:958.
Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. 2018;39:273–89.
Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:CD001431.
Legare F, Adekpedjou R, Stacey D, Turcotte S, Kryworuchko J, Graham ID, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2018;7:CD006732.
Rydland HT, Solheim EF, Eikemo TA. Educational inequalities in high- vs. low-preventable health conditions: exploring the fundamental cause theory. Soc Sci Med. 2020;267:113145.
Hall HI, Van Den Eeden SK, Tolsma DD, Rardin K, Thompson T, Hughes Sinclair A, et al. Testing for prostate and colorectal cancer: comparison of self-report and medical record audit. Prev Med. 2004;39:27–35.
Sayre EC, Bunting PS, Kopec JA. Reliability of self-report versus chart-based prostate cancer, PSA, DRE and urinary symptoms. Can J Urol. 2009;16:4463–71.
Davis K, Haisfield L, Dorfman C, Krist A, Taylor KL. Physicians’ attitudes about shared decision making for prostate cancer screening. Fam Med. 2011;43:260–6.
Smith SK, Dixon A, Trevena L, Nutbeam D, McCaffery KJ. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc Sci Med. 2009;69:1805–12.
Singh Ospina N, Toloza FJK, Barrera F, Bylund CL, Erwin PJ, Montori V. Educational programs to teach shared decision making to medical trainees: a systematic review. Patient Educ Couns. 2020;103:1082–94.
Funding
Boston Scientific (Marlborough, MA, United States) supported this research.
Author information
Authors and Affiliations
Contributions
The authors confirm their contribution to the paper as follows: study conception and design: LM, SB; data collection: LM; analysis and interpretation of results: all authors; draft manuscript preparation: LM; reviewed and approved the final version of the manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
N Bhojani is a consultant for Olympus, Boston Scientific, and Procept BioRobotics. L Miller is a consultant for Boston Scientific. K Zorn is a consultant and proctor for Boston Scientific, Procept BioRobotics, and investigator for Zenflow. B Chughtai is a consultant for Olympus, Boston Scientific, Ferring Pharmaceuticals, and Allergan. D Elterman reports grants and personal fees from Boston Scientific, grants from Olympus, grants from Urotronic, grants from Procept Biorobotics, and grants from Zenflow. S Bhattacharyya is an employee of Boston Scientific. B Chew is a consultant for Boston Scientific.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhojani, N., Miller, L.E., Zorn, K.C. et al. Prevalence and determinants of shared decision-making for PSA testing in the United States. Prostate Cancer Prostatic Dis (2024). https://doi.org/10.1038/s41391-024-00843-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-024-00843-x