Abstract
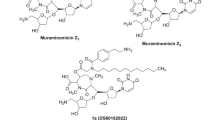
To overcome serious methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa infections, we synthesized TS2037, 5,4″-diepi-arbekacin, a novel aminoglycoside antibiotic, and evaluated its biological properties. TS2037 showed broad-range, as well as robust antibacterial activities against Gram-positive and Gram-negative bacteria. The MIC50 and MIC90 of TS2037 against clinical isolates of MRSA (n = 54) were both 0.25 µg/mL, and no resistant strain was observed. The MIC50 and MIC90 of TS2037 against clinical isolates of P. aeruginosa (n = 54) were 1 and 4 µg/mL, respectively. TS2037 and arbekacin, anti-MRSA aminoglycoside, were more stable against AAC(6′)-APH(2″), aminoglycoside-6′-N-acetyltransferase and 2″-O-phosphotransferase, produced by resistant S. aureus than gentamicin. Therapeutic efficacies of TS2037 in the mouse models of systemic infection with MRSA were superior to those of arbekacin, vancomycin, and linezolid. The efficacy of TS2037 against systemic infection caused by P. aeruginosa producing AAC(6′)-II was superior to those of arbekacin and amikacin. In the nephrotoxicity risk screening, the release of free N-acetyl-β-d-glucosaminidase from the kidney epithelial cell line after treatment with TS2037 at 2.5 and 5.0 μM were 2.0 and 2.1 (U/L), respectively, which were about two times higher than those of arbekacin. In conclusion, TS2037 exhibited the most potent antibacterial activity among aminoglycosides tested against both MRSA and P. aeruginosa in vitro and in vivo, although its nephrotoxicity risk remains to be improved.
Similar content being viewed by others
Introduction
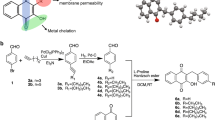
In recent years, infections caused by antibiotic-resistant strains have become a serious problem in the clinical field. In particular, methicillin-resistant Staphylococcus aureus (MRSA) is a major cause of nosocomial infections [1,2,3,4,5]. Recently, a community-acquired MRSA (CA-MRSA) has emerged that rapidly spread in the community, causing serious infections among young, and healthy individuals [5,6,7]. On the other hand, infection caused by Gram-negative bacteria, including drug-resistant Pseudomonas aeruginosa, has become a significant concern in the hospitals [8]. Meanwhile, currently available antibiotics against these serious infections caused by Gram-negative bacteria are not effective enough [9,10,11]. In order to overcome infections caused by antibiotic-resistant strains, namely MRSA and Gram-negative bacteria, including drug-resistant P. aeruginosa, we synthesized various arbekacin derivatives [12]. Among them, 5,4″-diepi-arbekacin (TS2037) emerged as the most potent anti-bacterial agent [12] (Fig. 1). Herein, we report evaluations of the efficacy of TS2037 against MRSA and P. aeruginosa in comparison with other antibiotics.
Materials and methods
Antibacterial agents
TS2037, evaluated here, was synthesized at the Pharmaceutical Research Center, Meiji Seika Pharma Co., Ltd. (Meiji, Kanagawa, Japan) [12]. The following reference antibacterial agents were purchased commercially: arbekacin, amikacin, and kanamycin B (Meiji), tobramycin and gentamicin (Sigma Chemical Co., St. Louis, MO, USA), imipenem/cilastatin (MSD, Tokyo, Japan), vancomycin (Shionogi & Co. Ltd., Osaka, Japan), teicoplanin (Sanofi K.K., Tokyo, Japan), linezolid (Pfizer Japan Inc., Tokyo, Japan), ciprofloxacin (Sequoia Research Products Ltd., Oxford, United Kingdom), and cefepime (Bristol-Myers Squibb Company, Tokyo, Japan).
Bacterial strains
The bacterial strains used in this study are listed in Table 1. The isogenic strains of S. aureus RN4220 and E. coli JM109 were made by transformation of plasmids, which were obtained from clinical isolates carrying aminoglycoside-resistant genes. We identified these isogenic strains with susceptibilities for aminoglycosides. P. aeruginosa PAO1 and its ΔmexXY/oprM derivative strains were kindly provided by Prof. Naomasa Gotoh, Kyoto Pharmaceutical University [13]. Clinical isolates were collected from various hospitals in Japan over a 10-year period.
Antimicrobial susceptibility testing
Minimum inhibitory concentrations (MICs) were determined by the two-fold agar dilution method according to the Clinical and Laboratory Standards Institute (CLSI) guideline.14MRSA and methicillin-resistant coagulase negative staphylococci (MR-CNS) were determined by the oxacillin MIC (≥4 µg/mL) in the Mueller–Hinton agar containing 2% NaCl as described in the CLSI guideline [14]. MIC50 and MIC90 were defined as the lowest concentration of an antibiotic at which 50 and 90% of the tested strains were inhibited, respectively.
Bactericidal activity against MRSA
Five clinical isolates of gentamicin-resistant MRSA were used in this study. After preincubation at 35 °C for 2 h, each drug was added to the bacterial cultures at the final concentrations of 4, 2, and 1 times the MIC. No antibiotic was added to the control. The number of viable cells was counted from colonies on the agar plate after overnight culture at 35 °C.
Aminoglycoside modifying enzyme assay
For preparation of cell-free extract, S. aureus RN4220/pMF490 harboring the aac(6′)-aph(2”) gene was incubated in Luria–Bertani broth at 35 °C while on a shaker. After optimal density at 625 nm reached 0.7–0.8, the cells were harvested by centrifugation and washed with 50 mM tris–(hydroxymethyl)aminomethane buffer (pH 7.6). Then the cells resuspended in the same buffer containing 0.1 mm glass beads, and were disrupted using a Beads Shocker (Yasui Kikai, Tokyo, Japan). After centrifugation at 17,000×g for 30 min at 4 °C, the supernatant was pooled as cell-free extract. Protein concentration of the supernatant was measured by Bio-Rad protein assay kit (Bio-Rad Japan, Tokyo, Japan) and the supernatant was stored at −80 °C until use.
TS2037, arbekacin, gentamicin, and kanamycin B were incubated in the presence of acetyl-CoA and ATP with cell-free extract from S. aureus RN4220/pMF490. Modifications of aminoglycosides were analyzed by liquid chromatography/electrospray ionization (ESI) mass spectrometry method.
In vivo efficacy
All animal studies and protocols for the evaluation of TS2037 were in accordance with the Guidelines on the Management of Animal Experiments established by the Pharmaceutical Research Center and approved by the Animal Experiment Management Committee of the Pharmaceutical Research Center, Meiji. Four-week-old male ICR mice were purchased from Charles River Japan, Inc. (Kanagawa, Japan). In vivo efficacies were assessed in systemic infections caused by MRSA and P. aeruginosa in mice. Mice were treated with cyclophosphamide at 200 mg/kg by intraperitoneal administration except for P. aeruginosa PAO1, which was infected in mice without the cyclophosphamide treatment. Four days later, each inoculum suspended in 5% mucin was injected intraperitoneally to ICR mice. Drugs were administered subcutaneously 2 h (and 6 h for P. aeruginosa MSC3151 infection) after the bacterial challenge. Fifty percent effective dose (ED50) was determined for each agent from the total number of surviving mice on day 7 after the infection using the Probit analysis method.
N-Acetyl-β-d-glucosaminidase (NAG) assay
NAG is a lysosomal enzyme that is expressed in various tissues, including kidney. Increased concentration of NAG in urine indicates renal tubular cell breakdown. The release of NAG from the kidney epithelial cell line, LLC-PK1, grown on microporous culture inserts (3.0 μm pore size) as confluent monolayers, was determined in in vitro nephrotoxic activity. NAG activity in the serum-free apical conditioned medium was quantified using sodio-m-cresolsulfonphthaleinyl N-acetyl-β-d-glucosaminide as substrate [15].
Results
Antibacterial spectrum
To evaluate the effect of several resistant mechanisms of aminoglycoside on the activity of TS2037, the MICs against parent strains and their isogenic derivatives, type strains, and well-characterized clinical isolates harboring aminoglycoside modifying enzyme were determined.
Antibacterial spectra of TS2037, other aminoglycosides, and imipenem against 20 pathogenic bacteria are shown in Table 1. Though TS2037 clearly showed superior antibacterial activity (MIC: 0.25 μg/mL) against S. aureus RN4220 (MSSA) and RN4220 derivatives producing ANT(3′)-III, ANT(4′)-I, and AAC(6′)-APH(2″), it was thought that TS2037 was slightly modified with these aminoglycoside modifying enzyme. The activity of arbekacin and gentamicin showed a slight (4–16 times) and marked (≥512 times) decrease against S. aureus producing AAC(6′)-APH(2″), respectively. Amikacin and tobramycin showed weak activity against most of S. aureus strains harboring aminoglycoside modifying enzyme. Gratifyingly, TS2037 showed certain antibacterial activity against vancomycin-resistant Enterococcus faecim (VRE). Furthermore, TS2037 also displayed potent antibacterial activity against various Gram-negative bacteria, except Burkholderia cepacia and Serratia marcescens, and P. aeruginosa PAO1/GN315 producing AAC(6′)-I. Although the MIC of TS2037 increased, such as other aminoglycosides in the presence of MexXY multidrug efflux system, an aminoglycoside efflux pump in P. aeruginosa, the basic activity of TS2037 for P. aeruginosa PAO1 was lower and comparable to that of tobramycin.
Collectively, TS2037 exhibits wide-range of antibiotic activity against both Gram-positive and Gram-negative bacteria, and is stable against various aminoglycoside-modifying enzyme, such as ANT(3′)-III, ANT(4′)-I, and AAC(6′)-APH(2″).
Antibacterial activity against clinical isolates
TS2037 clearly showed potent antibacterial activity against various Gram-positive and Gram-negative bacteria (Table 1). Thus, we further evaluated the antibacterial activities of TS2037, as well as other known antibiotics against 241 strains of clinical isolates (Table 2). The MIC90 values of TS2037 against clinical isolates of MRSA and MRCNS were 0.25 and 0.12 μg/mL, respectively, and showed no resistant strain, determined by reference to criteria of other aminoglycosides in CLSI [14]. The activity of TS2037 against E. faecium was moderate and equaled to that of gentamicin. It also displayed potent activity against Escherichia coli and Klebsiella pneumonia, including gentamicin-resistant and tobramycin-resistant isolates. Furthermore, the MIC90 of TS2037 against P. aeruginosa was the lowest among the antibiotics tested. These results clearly indicate that TS2037 shows the most potent activity among aminoglycosides tested against the drug-resistant Gram-positive and Gram-negative bacteria, including MRSA and P. aeruginosa.
Bactericidal activity
To evaluate the bactericidal activity of T2037 for MRSA, the time killing curves of TS2037 against five clinical isolates of gentamicin-resistant MRSA were compared with those of arbekacin, gentamicin, vancomycin, and linezolid, and the MICs are shown in Table 3. TS2037 showed more potent bactericidal activity than arbekacin and gentamicin, with respect to MIC-based concentrations (Fig. 2). On the other hand, vancomycin and linezolid showed weaker bactericidal and bacteriostatic activities against MRSA. These results clearly demonstrated the strongest bactericidal activity of TS2037 at the lowest concentration among the antibiotics tested.
Killing curves of TS2037 and other antibiotics against 5 isolates of methicillin-resistant S. aureus. The data points represent averages of the five strains tested. a TS2037 (MIC: 0.5–1 μg/mL), b arbekacin (MIC: 1–4 μg/mL), c gentamicin (MIC: 64–128 μg/mL), d vancomycin (MIC: 1 μg/mL), and e linezolid (MIC: 2 μg/mL). Symbols: °, 1 × MIC; Δ, 2 × MIC; ●, 4 × MIC. The solid line indicates growth control. No antibiotic was added to the control. Error bars represent ± standard deviation
Effect on aminoglycoside modifying enzyme
To understand superior activity of TS2037 against aminoglycoside-resistant strains, we performed stability test of TS2037 against aminoglycoside modifying enzyme in comparison with those of other aminoglycoside drugs. Figure 3 shows the modification of TS2037, arbekacin, gentamicin, and kanamycin B by bifunctional enzyme AAC(6′)-APH(2″) from S. aureus RN4220/pMF490. Gentamicin and kanamycin B were markedly modified by AAC(6′)-APH(2″). In the presence of 0.3 mg protein/mL, most of the gentamicin and kanamycin B were modified to their 2″-O-phosporylation, 6′-N-acetylation, as well as both derivatives. On the other hand, TS2037 and arbekacin resisted modification(s) by AAC(6′)-APH(2″). In particular, TS2037 exhibited greater stability even at a high concentration of crude enzyme (1.0 mg protein/mL).
Protective effect against systemic infection
To identify the relationship between the in vitro and in vivo activities of TS2037, the protective effect of TS2037 against systemic infection caused by MRSA or P. aeruginosa in mice was evaluated. As shown in Table 4, the ED50s of TS2037 against MRSA MF126 and MRSA MF535 were 2.65 and 0.85 mg/kg, respectively, which were lower than those of arbekacin, gentamicin, vancomycin, and linezolid. The ED50s of TS2037 against P. aerugonosa PAO1 and P. aeruginosa MSC3151 were 0.38 and 7.10 mg/kg, respectively, which were the lowest among aminoglycoside antibiotics tested.
NAG release from LLC-PK1
The NAG release from LLC-PL1 cells by TS2037 and arbekacin was determined to compare nephrotoxic potential, which is one of the side effects of aminoglycoside. The NAG releases from LLC-PK1 after treatment with TS2037 at 2.5 and 5 μM were 2.0 and 2.1 (U/L), respectively, and those were higher than that of arbekacin (Table 5). This results suggest the nephrotoxicity risk of TS2037 is higher than that of arbekacin.
Discussion
MRSA and P. aeruginosa are challenging nosocomial pathogens, commonly causing mixed infections, and are often resistant to multiple drugs. Arbekacin is an aminoglycoside launched for treatment of MRSA infections in Japan, but it is also active against Gram-negative bacteria including the drug-resistant P. aeruginosa [16]. In the course of our research program to obtain drugs with more improved efficacy than arbekacin, its 5,4″-diepi derivative, TS2037 showed strong activities against MRSA and P. aeruginosa [17]. We studied in vitro and in vivo activities of TS2037 against Gram-positive and Gram-negative bacteria.
One of the resistant mechanisms of bacteria to aminoglycosides is inactivation by producing aminoglycoside-modifying enzymes, such as acetyltransferase, phosphotransferase, and adenylyltransferase [18]. These enzymes, in general, can confer some degrees of resistance to each aminoglycoside based on their substrate specificities. Indeed, while a number of aminoglycoside-resistant MRSA strains have appeared, arbekacin still showed sufficient clinical efficacy [19,20,21].
Arbekacin is modified by AAC(6′)-APH(2″) at a lower rate than gentamicin, which explains why majority of the staphylococci possessing aac(6′)-aph(2″) remains susceptible to arbekacin in vitro [22]. In this study, the residual rate of TS2037 possessing antibacterial activity was higher than that of arbekacin after the reaction with crude enzyme preparation, derived from strains producing aminoglycoside-modifying enzyme at each protein concentration. Both gentamicin and amikacin were affected by these aminoglycoside-modifying enzymes and that translated to the antibacterial activities against such aminoglycoside-resistant strains. We believe that is why the antibacterial activity of TS2037 for S. aureus RN4220/pR1948 and RN4220/pMF490 is superior to amikacin. We analyzed the variations of MICs of amikacin for these strains depend on the amount of AAC(6′)-APH-(2″) enzyme, and the antibacterial activity also depends on the enzyme stability. That is consistent to the result in which no resistant strain of TS2037 determined by reference to criteria of other aminoglycosides in CLSI [14] was observed in laboratory strains or clinical isolates of MRSA. As in the case of most other aminoglycosides, TS2037 had mild activity against Enterococcus spp. High-level gentamicin resistance in the vast majority of enterococci is associated with the presence of bifunctional enzyme AAC(6′)-APH(2″). As shown in Table 1, TS2037 was more effective to E. faecium producing this enzyme than other aminoglycosides tested, except for arbekacin. In consideration of this result, we presumed both TS2037 and arbekacin were more stable to the bifunctional enzyme, AAC(6′)-APH(2″), derived from enterococci-like MRSA than other aminoglycosides.
The bactericidal activity of TS2037 at a concentration of four times the MIC against MRSA strains was the strongest among those of arbekacin, gentamicin, vancomycin, and linezolid. The stability of TS2037 for aminoglycoside-modifying enzymes, such as AAC(6′)-APH(2″) would contribute to not only the high antibacterial activity, which indicates the effect on bacterial growth, but also the improvement of bactericidal activity which indicates the ability of killing bacteria.
Five resistant mechanisms of aminoglycosides in P. aeruginosa have been reported as follows: (i) modification by enzyme, (ii) impairment of outer membrane uptake, (iii) reduction in active transport, (iv) increase in MexXY-OprM-mediated active efflux, and (v) alteration of target of aminoglycosides [23]. MexXY is an aminoglycoside-inducible multidrug transporter shown to contribute to intrinsic and acquired aminoglycoside resistance in clinical isolates of P. aeruginosa. We, therefore, compared the aminoglycoside substrate specificity of MexXY efflux system of P. aeruginosa using laboratory isogenic strains of PAO1 and its ΔMexXY (deleted MexXY) derivative. The effect of MexXY on MICs of TS2037 was less than those of other aminoglycosides, except tobramycin that exerted the same effect. We believe that the less effect of MexXY on TS2037 activity contributes to high intrinsic susceptibility to P. aeruginosa, as in the case of tobramycin.
The improved activity of TS2037 in in vitro study also translated into in vivo acute systemic infections in mice. When it was dosed subcutaneously, TS2037 showed protective effect against infections caused by MRSA carrying ANT(4′) or AAC(6′)-APH(2″). The ED50s of TS2037 in the models of systemic infection caused by MRSA were also lower than those of arbekacin, gentamicin, vancomycin, and linezolid. In the model of systemic infection caused by aminoglycoside susceptible and resistant P. aeruginosa strains, TS2037 was more effective than all other aminoglycosides tested. The results in the animal models support the evaluation of TS2037 clinical efficacy in humans, and also predict clinical efficacy in the empirical treatment of severe infections.
On contrary, the results of NAG release from LLC-PK1 suggest that the nephrotoxicity risk associated to TS2037 might be higher than that of arbekacin. Hence, we need to analyze PK/PD data carefully for the dosage and administration of TS2037 in clinical use, in reference to arbekacin. However, the acquired data showed TS2037 is more stable to aminoglycoside-modifying enzymes and has higher efficacy against strains producing these enzymes, such as MRSA than other aminoglycosides including arbekacin. We therefore believe there is some appropriate dosing of TS2037 for its potent efficacy, like short-term dosing as in the case of plazomicin [24].
At present, antibiotics used for the treatment of MRSA are arbekacin, vancomycin, teicoplanin, linezolid, and daptomycin in Japan, and several new anti-MRSA compounds have emerged recently from the clinical developments. Most of these possess antimicrobial efficacy only to Gram-positive bacteria, but not Gram-negative pathogens. On the other hand, with a handful of antimicrobials in the development for Gram-negative bacteria, the future drug design should focus not only MRSA but also drug-resistant Gram-negative pathogens, including P. aeruginosa. As an added advantage, beside having activity against both Gram-positive and Gram-negative bacteria, TS2037 is also active against MRSA and P. aeruginosa. Although several new anti-MRSA drugs that have been developed in the clinical settings, aminoglycoside TS2037 is one of the very promising candidates with potent antimicrobial activities, and should find its way into further evaluations.
References
Tokajian S. New epidemiology of Staphylococcus aureus infections in the Middle East. Clin Microbiol Infect. 2014;20:624–8.
Chen CJ, Huang YC. New epidemiology of Staphylococcus aureus infection in Asia. Clin Microbiol Infect. 2014;20:605–23.
Sharma Y, Jain S, Singh H, Govil V. Staphylococcus aureus: Screening for nasal carriers in a community setting with special reference to MRSA. Science. 2014;2014:479048.
Coombs GW, Monecke S, Pearson JC, Tan HL, Chew YK, et al. Evolution and diversity of community-associated methicillin-resistant Staphylococcus aureus in a geographical region. BMC Microbiol. 2011;11:215.
Cocchi P, Taccetti G, Montagnani C, Campana S, Galli L, et al. Evidence of transmission of a Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus clone: a family affair. Clin Microbiol Infect. 2013;19:1158–62.
Shetty V, Trumbull K, Hegde A, Shenoy V, Prabhu R, et al. Prevalence of community-acquired methicillin-resistant Staphylococcus aureus nasal colonization among children. J Clin Diagn Res. 2014;8:DC12–5.
Lo WT, Lin WJ, Tseng MH, Lu JJ, Lee SY, et al. Nasal carriage of a single clone of community-acquired methicillin-resistant Staphylococcus aureus among kindergarten attendees in Northern Taiwan. BMC Infect Dis. 2007;7:51.
Ali Z, Mumtaz N, Naz SA, Jabeen N, Shafique M. Multi-drug resistant Pseudomonas aeruginosa: a threat of nosocomial infections in tertiary care hospitals. J Pak Med Assoc. 2015;65:12–6.
Rodrigues AC, Chang MR, Nóbrega GD, Rodrigues MS, Carvalho NC, et al. Metallo-β-lactamase and genetic diversity of Pseudomonas aeruginosa in intensive care units in Campo Grande, MS, Brazil. Braz J Infect Dis. 2011;15:195–9.
Karlowsky JA, Hoban DJ, Hackel MA, Lob SH, Sahm DF. Antimicrobial susceptibility of Gram-negative ESKAPE pathogens isolated from hospitalized patients with intra-abdominal and urinary tract infections in Asia-Pacific countries: SMART 2013-2015. J Med Microbiol. 2017;66:61–9.
Mediavilla JR, Patrawalla A, Chen L, Chavda KD, Mathema B, et al. Colistin- and carbapenem-resistant Escherichia coli harboring mcr-1 and blaNDM-5, causing a complicated urinary tract infection in a patient from the United States. MBio. 2016;30:7.
Hiraiwa Y, Minowa N, Usui T, Akiyama Y, Maebashi K, et al. Effect of varying the 4”-position of arbekacin derivatives on antibacterial activity against MRSA and Pseudomonas aeruginosa. Bioorg Med Chem Lett. 2007;17:6369–72.
Masuda N, Sakagawa E, Ohya S, Gotoh N, Tsujimoto H, et al. Contribution of the MexX-MexY-oprM efflux system to intrinsic resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2000;44:2242–6.
Performance standards for antimicrobial susceptibility testing; Twenty-second informational supplement. Clinical and Laboratory Standards Institute. 2012;M100-S22.
Takahashi Y, Umemura E, Kobayashi Y, Murakami S, Nawa T et al. Discovery of 2-hydroxyarbekacin, a new aminoglycoside antibiotic with reduced nephrotoxicity. J Antibiot 2017;1–3. https://doi.org/10.1038/ja.2017.60.
Kondo S, Iinuma K, Yamamoto H. Syntheses of 1-N-(S)-4-amino-2-hydroxybutyryl)-kanamycin B and -3′, 4′-dideoxykanamycin B active against kanamycin-resistant bacteria. J Antibiot. 1973;26:412–5.
Hiraiwa Y, Usui T, Akiyama Y, Maebashi K, Minowa N. Synthesis and antibacterial activity of 5-deoxy-5-episubstituted arbekacin derivatives. Bioorg Med Chem Lett. 2007;17:3540–3.
Magnet S, Blanchard JS. Molecular insights into aminoglycoside action and resistance. Chem Rev. 2005;105:477–98.
Goto H, Iwasaki M. Susceptibilities of bacteria isolated from patients with lower respiratory infectious diseases to antibacterial agents. Jpn J Antibiot. 2015;68:85–104. (2010)
Matsumoto T. Arbekacin: another novel agent for treating infections due to methicillin-resistant Staphylococcus aureus and multidrug-resistant Gram-negative pathogens. Clin Pharmacol. 2014;6:139–48.
Holbrook SY, Garneau-Tsodikova S. Expanding aminoglycoside resistance enzyme regiospecificity by mutation and truncation. Biochemistry. 2016;55:5726–37.
Tabata M, Shimizu M, Araake M, Ogawa H. Relationship between arbekacin-susceptibility and aminoglycoside-resistant gene of methicillin-resistant Staphylococcus aureus (MRSA). Jpn J Antibiot. 2003;56:36–43.
Keith P. Aminoglycoside resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49:479–87.
Cass RT, Brooks CD, Havrilla NA, Tack KJ, Borin MT, et al. Pharmacokinetics and safety of single and multiple doses of ACHN-490 injection administered intravenously in healthy subjects. Antimicrob Agents Chemother. 2011;55:5874–80.
Acknowledgements
We thank Prof. Naomasa Gotoh, Kyoto Pharmaceutuical University, for kindly providing us with P. aeruginosa PAO1 and its ΔmexXY/oprM derivative strain. We also thank Ms. Erumi Murase for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hirai, Y., Maebashi, K., Fushimi, H. et al. In vitro and in vivo antimicrobial activity of TS2037, a novel aminoglycoside antibiotic. J Antibiot 71, 363–371 (2018). https://doi.org/10.1038/s41429-017-0002-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41429-017-0002-2