Abstract
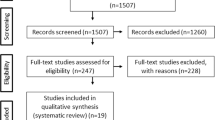
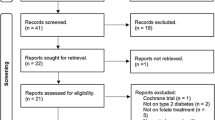
There has been no established food and nutrition guidance for diseases characterized by the presence of iron overload (IOL) yet. Hepcidin is a hormone that diminishes iron bioavailability. Its levels increase in response to increased iron stores. Hence, IOL conditions could hypothetically trigger a self-regulatory mechanism for the reduction of the intestinal absorption of iron. In addition, some food substances may modulate intestinal iron absorption and may be useful in the dietary management of patients with IOL. This scoping review aimed to systematize studies that support dietary prescriptions for IOL patients. It was carried out according to the method proposed by the Joanna Briggs Institute and the preferred reporting items for systematic reviews and meta-analyses (PRISMA). Although the need to restrict iron in the diet of individuals with hemochromatosis is quite clear, there is a consensus that IOL diminishes the rate of iron absorption. Reduced iron absorption is also present and has been reported in some diseases with transfusion IOL, in which serum hepcidin is usually high. The consumption of polyphenols and 6-shogaol seems to reduce iron absorption or serum ferritin concentration, while procyanidins do not cause any changes. Vitamin C deficiency is often found in IOL patients. However, vitamin C supplementation and alcohol consumption should be avoided not only because they increase iron absorption, but also because they provoke toxic oxidative reactions when the iron is excessive. Dietary approaches must consider the differences in the pathophysiology and treatment of IOL diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
McDermid JM, Lönnerdal B. Iron. Adv Nutr. 2012;3:532–3. https://doi.org/10.3945/an.112.002261
Green R, Charlton R, Seftel H, Bothwell T, Mayet F, Adams B, et al. Body iron excretion in man: a collaborative study. Am J Med. 1968;45:336–53. https://doi.org/10.1016/0002-9343(68)90069-7
Ganz T, Nemeth E. Hepcidin and iron homeostasis. Biochim Biophys Acta. 2012;1823:1434–43. https://doi.org/10.1016/j.bbamcr.2012.01.014
Ward R. An update on disordered iron metabolism and iron overload. Hematology. 2010;15:311–7. https://doi.org/10.1179/102453310X12647083621164
Darbari DS, Kple-Faget P, Kwagyan J, Rana S, Gordeuk VR, Castro O. Circumstances of death in adult sickle cell disease patients. Am J Hematol. 2006;81:858–63. https://doi.org/10.1002/ajh.20685
Piperno A, Pelucchi S, Mariani R. Inherited iron overload disorders. Transl Gastroenterol Hepatol. 2020;5:25 https://doi.org/10.21037/tgh.2019.11.15
Piperno A. Classification and diagnosis of iron overload. Haematolgica. 1998;83:447–55.
Fowler C. Hereditary hemochromatosis: pathophysiology, diagnosis, and management. Crit Care Nurs Clin North Am. 2008;20:191–201. https://doi.org/10.1016/j.ccell.2008.01.003
Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American association for the study of liver diseases. Hepatology. 2011;54:328–43. https://doi.org/10.1002/hep.24330.
Tavill AS. American association for the study of liver diseases, American college of gastroenterology; American gastroenterological association. diagnosis and management of hemochromatosis. Hepatology. 2001;33:1321–8. https://doi.org/10.1053/jhep.2001.24783
Powell LW, Seckington RC, Deugnier Y. Haemochromatosis. Lancet. 2016;388:706–16. https://doi.org/10.1016/S0140-6736(15)01315-X
Rachmilewtiz EA, Giardina PJ. How I treat thalassemia. Blood. 2011;118:3479–88. https://doi.org/10.1182/blood-2010-08-300335
Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010;376:2018–31. https://doi.org/10.1016/S0140-6736(10)61029-X
Giardina PJ, Grady RW. Chelation therapy in beta-thalassemia: the benefits and limitations of desferroxamine. Semin Hematol. 1995;32:304–12.
Ganz T, Nemeth E. Iron imports. IV. Hepcidin and regulation of body iron metabolism. Am J Physiol Gastrointest Liver Physiol. 2006;290:G199–203. https://doi.org/10.1152/ajpgi.00412.2005
Ohemeng A, Boadu I. The role of nutrition in the pathophysiology and management of sickle cell disease among children: a review of literature. Crit Rev Food Sci Nutr. 2018;58:2299–305. https://doi.org/10.1080/10408398.2017.1319794
Ganz T. Hepcidin and its role in regulating systemic iron metabolism. Hematol Am Soc Hematol Educ Program. 2006;507:29–35. https://doi.org/10.1182/asheducation-2006.1.29
Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2015;6:62–72. https://doi.org/10.4291/wjgp.v6.i3.62
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: scoping reviews (2020 version). In: Aromatari ES, Munn Z, editors. JBI manual for evidence synthesis. JBI, 2020. https://synthesismanual.jbi.global Accessed 7 June 2020.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097 https://doi.org/10.1371/journal.pmed.1000097
Bezwoda WR, Disler PB, Lynch SR, Charlton RW, Torrance JD, Derman D, et al. Patterns of food iron absorption in iron-deficient white and indian subjects and in venesected haemochromatotic patients. Br J Haematol. 1976;33:425–36. https://doi.org/10.1111/j.1365-2141.1976.tb03560.x
Lynch SR, Skikne BS, Cook JD. Food iron absorption in idiopathic hemochromatosis. Blood. 1989;74:2187–93.
Milder MS, Cook JD, Finch CA. Influence of food iron absorption on the plasma iron level in idiopathic hemochromatosis. Acta Haematol. 1978;60:65–75. https://doi.org/10.1159/000207699
Kaltwasser JP, Werner E, Schalk K, Hansen C, Gottschalk R, Seidl C. Clinical trial on the effect of regular tea drinking on iron accumulation in genetic haemochromatosis. Gut. 1998;43:699–704. https://doi.org/10.1136/gut.43.5.699
Lobbes H, Gladine C, Mazur A, Pereira B, Dualé C, Cardot JM. Effect of procyanidin on dietary iron absorption in hereditary hemochromatosis and in dysmetabolic iron overload syndrome: a crossover double-blind randomized controlled trial. Clin Nutr. 2020;39:97–103. https://doi.org/10.1016/j.clnu.2019.02.012
Golombick T, Diamond TH, Manoharan A, Ramakrishna R, Badmaev V. Effect of the ginger derivative, 6-shogaol, on ferritin levels in patients with low to intermediate-1-risk myelodysplastic syndrome—a small, investigative study. Clin Med Insights Blood Disord. 2017;10:1179545X17738755 https://doi.org/10.1177/1179545X17738755
Elalfy MS, Saber MM, Adly AAM, Ismail EA, Tarif M, Ibrahim F, et al. Role of vitamin C as an adjuvante therapy to different iron chelators in young β-thalassemia major patients: efficacy and safety in relation to tissue iron overload. Eur J Haematol. 2015;96:318–26. https://doi.org/10.1111/ejh.12594
Chapman RW, Hussain MA, Gorman A, Laulicht M, Politis D, Flynn DM, et al. Effect of ascorbic acid deficiency on serum ferritin concentration in patients with β-thalassemia major and iron overload. J Clin Pathol. 1982;35:487–91. https://doi.org/10.1136/jcp.35.5.487
Walters GO, Jacobs A, Worwood M, Trevett D, Thomson W. Iron absorption in normal subjects and patients with idiopathic haemochromatosis: relationship with serum ferritin concentration. Gut. 1975;16:188–92. https://doi.org/10.1136/gut.16.3.188
International Atomic Energy Agency (IAEA). Assessment of iron bioavailability in humans using stable iron isotope techniques. IAEA Human Health Series no. 21. International Atomic Energy Agency, Austria, 2012.
De Alarcon PA, Donovan ME, Forbes GB, Landaw AS, Stockman JA 3rd. Iron absorption in the thalassemia syndromes and its inhibition by tea. N Engl J Med. 1979;300:5–8. https://doi.org/10.1056/NEJM197901043000102
Alqasoumi S, Yusufoglu H, Farraj A, Alam A. Effect of 6-shogaol and 6-gingerol on diclofenac sodium induced liver injury. Int J Pharm. 2011;7:868–73. https://doi.org/10.3923/ijp.2011.868.873
Zhuang X, Deng ZB, Mu J, Zhang L, Yan J, Miller D, et al. Ginger-derived nanoparticles protect against alcohol-induced liver damage. J Extracell Vesicles. 2015;4:1–18. https://doi.org/10.3402/jev.v4.28713
Bell H, Skinningsrud A, Raknerud N, Try K. Serum ferritin and transferrin saturation in patients with chronic alcoholic and non-alcoholic liver diseases. J Intern Med. 1994;236:315–22. https://doi.org/10.1111/j.1365-2796.1994.tb00802.x
Rouault TA. Hepatic iron overload in alcoholic liver disease: why does it occur and what is its role in pathogenesis? Alcohol. 2003;30:103–6. https://doi.org/10.1016/s0741-8329(03)00102-2
Harrison-Findik DD, Schafer D, Klein E, Timchenko NA, Kulaksiz H, Clemens D, et al. Alcohol metabolism-mediated oxidative stress down-regulates hepcidin transcription and leads to increased duodenal iron transporter expression. J Biol Chem. 2006;281:22974–82. https://doi.org/10.1074/jbc.M602098200
Milman N, Kirchhoff M. Relationship between serum ferritin, alcohol intake, and social status in 2235 Danish men and women. Ann Hematol. 1996;72:145–51. https://doi.org/10.1007/s002770050153
Whitfield JB, Zhu G, Heath AC, Powell LW, Martin NG. Effects of alcohol consumption on indices of iron stores and of iron stores on alcohol intake markers. Alcohol Clin Exp Res. 2001;25:1037–45.
Ioannou GN, Dominitz JA, Weiss NS, Heagerty PJ, Kowdley KV. The effect of alcohol consumption on the prevalence of iron overload, iron deficiency, and iron deficiency anemia. Gastroenterology. 2004;126:1293–301. https://doi.org/10.1053/j.gastro.2004.01.020
Fletcher LM, Dixon JL, Purdie DM, Powell LW, Crawford DHG. Pathophysiological classification of iron overloa Excess alcohol greatly increases the prevalence of cirrhosis in hereditary hemochromatosis. Gastroenterology. 2002;122:281–9. https://doi.org/10.1053/gast.2002.30992
Scotet V, Mérour MC, Mercier AY, Chanu B, Le Faou T, Raguénes O, et al. Hereditary hemochromatosis: Effect of excessive alcohol consumption on disease expression in patients homozygous for the C282Y mutation. Am J Epidemiol. 2003;158:129–34. https://doi.org/10.1093/aje/kwg123
Lane DJR, Bae DH, Merlot AM, Sahni S, Richardson DR. Duodenal cytochrome b (DCYTB) in iron metabolism: an update on function and regulation. Nutrients. 2015;7:2274–96. https://doi.org/10.3390/nu7042274
Chiu PF, Ko SY, Chang CC. Vitamin C affects the expression of hepcidin and erythropoietin receptor in HepG2 cells. J Ren Nutr. 2012;22:373–6. https://doi.org/10.1053/j.jrn.2011.09.007
O´Brien RT. Ascorbic acid enhancement of desferrioxamine-induced urinary iron excretion in thalassemia major. Ann N Y Acad Sci. 1974;232:221–5. https://doi.org/10.1111/j.1749-6632.1974.tb20588.x
Modell CB, Beck J. Long-term desferrioxamine therapy in thalassemia. Ann N Y Acad Sci. 1974;232:201–10. https://doi.org/10.1111/j.1749-6632.1974.tb20586.x
Brissot P, Deugnier Y, Le Treut A, Regnouard F, Simon M, Bourel M. Ascorbic acid status in idiopathic hemochromatosis. Digestion. 1978;17:479–87. https://doi.org/10.1159/000198154
Sarantos K, Evans P, Garbowski M, Davis B, Porter JB. Vitamin C in patients on long-term deferasirox without supplementation. Blood. 2008;112:1858 https://doi.org/10.1182/blood.V112.11.1858.1858
Schulz EJ, Swanepoel H. Scorbutic pseudoscleroderma: an aspect of Bantu siderosis. S Afr Med J. 1962;36:367–72.
Lynch SR, Seftel HC, Torrance JD, Charlton RW, Bothwell TH. Accelerated oxidative catabolism of ascorbic acid in siderotic Bantu. Am J Clin Nutr. 1967;20:641–7. https://doi.org/10.1093/ajcn/20.6.641
Imam MU, Zhang S, Ma J, Wang H, Wang F. Antioxidants mediate both iron homeostasis and oxidative stress. Nutrients. 2017;9:3–19. https://doi.org/10.3390/nu9070671
Erlandson ME, Walden B, Stern G, Hilgartner MW, Wehman J, Smith CH. Studies on congenital hemolytic syndromes, IV. Gastrointestinal absorption of iron. Blood. 1962;19:359–78.
Ringelhann B, Konotey-Ahulu F, Dodu SR. Studies on iron metabolism in sickle cell anaemia, sickle cell haemoglobin C disease, and haemoglobin C disease using a large volume liquid scintillation counter. J Clin Pathol. 1970;23:127–34. https://doi.org/10.1136/jcp.23.2.127
Omena J, Cople-Rodrigues CS, Cardoso JDA, Soares AR, Fleury MK, Brito FSB, et al. Serum hepcidin concentration in individuals with sickle cell anemia: Basis for the dietary recommendation of iron. Nutrients. 2018;10:498 https://doi.org/10.3390/nu10040498
Mangaonkar AA, Thawer F, Son J, Ajebo G, Xu H, Barrett NJ, et al. Regulation of iron homeostasis through the erythroferrone-hepcidin axis in sickle cell disease. Br J Haematol. 2020;189:1204–9. https://doi.org/10.1111/bjh.16498
Acknowledgements
The authors thank the Brazilian Ministry of Health for encouraging scientific research on sickle cell disease between 2010 and 2014.
Funding
This study was funded by the Ministry of Health (process# 777022/2012), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (process# 408401/2017-6); Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES) (Finance Code 001).
Author information
Authors and Affiliations
Contributions
JO participated in the conception and design of the study and wrote the first draft of the manuscript. MC developed the concept and design of this study, supervised the writing of the manuscript, and revised the final version. CC and CSCR critically revised the manuscript and contributed to the writing of the manuscript. All authors were involved in the review and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Omena, J., Curioni, C., Cople-Rodrigues, C.d.S. et al. The effect of food and nutrients on iron overload: what do we know so far?. Eur J Clin Nutr 75, 1771–1780 (2021). https://doi.org/10.1038/s41430-021-00887-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00887-5
This article is cited by
-
Evaluation of dietary composition between hemoglobin categories, total body iron content and adherence to multi-micronutrients in preschooler residents of the highlands of Puno, Peru
BMC Nutrition (2024)
-
Influence of Fe(III) on the Fluorescence of Lysozyme: a Facile and Direct Method for Sensitive and Selective Sensing of Fe(III)
Journal of Fluorescence (2021)