Abstract
Background
Intra-individual coexistence of anthropometrically defined undernutrition and ‘metabolic obesity’, characterised by presence of at least one abnormal cardiometabolic risk factor, is rarely investigated in young children and adolescents, particularly in Low-and-Middle-Income-Countries undergoing rapid nutrition transition.
Methods
Prevalence of biomarkers of metabolic obesity was related to anthropometric and socio-demographic characteristics in 5–19 years old participants from the population-based Comprehensive National Nutrition Survey in India (2016–2018). The biomarkers, serum lipid-profile (total cholesterol (TC), low density lipoprotein (LDL), high density lipoprotein (HDL) and triglycerides), fasting glucose, and glycosylated hemoglobin (HbA1C), and all jointly were analysed in 22567, 23192, 25962 and 19143 participants, respectively.
Results
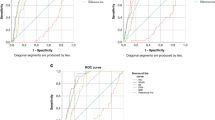
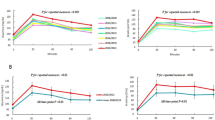
Overall (entire dataset), the prevalence of abnormalities was low (4.3–4.5%) for LDL and TC, intermediate for dysglycemia (10.9–16.1%), and high for HDL and triglycerides (21.7–25.8%). Proportions with ≥1 abnormal metabolic obesity biomarker(s) were 56.2% overall, 54.2% in thin (BMI-for-age < −2 SD) and 59.3% in stunted (height-for-age < −2 SD) participants. Comparable prevalence was evident in mild undernutrition (−1 to −2 SD). Clustering of two borderline abnormalities occurred in one-third, warranting active life-style interventions. Metabolic obesity prevalence increased with BMI-for-age. Among those with metabolic obesity, only 9% were overweight/obese (>1 SD BMI-for-age). Among poor participants, triglyceride, glucose and HDL abnormalities were higher.
Conclusions
A paradoxical, counter-intuitive prevalence of metabolic obesity biomarker(s) exists in over half of anthropometrically undernourished and normal-weight Indian children and adolescents. There is a crucial need for commensurate investments to address overnutrition along with undernutrition. Nutritional status should be characterized through additional reliable biomarkers, instead of anthropometry alone.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
World Health Organization. Guideline: implementing effective actions for improving adolescent nutrition. Geneva: World Health Organization; 2018. p. 1–59.
World Health Organization. Growth reference data for 5–19 years. Growth reference 5–19 years [website]. Geneva: World Health Organization; 2007 (http://www.who.int/growthref/en/, accessed 20 Jul 2020).
World Health Organization. The double burden of malnutrition: policy brief. Geneva: World Health Organization; 2017 (http://apps.who.int/iris/bitstream/10665/255413/1/WHO-NMH-NHD-17.3-eng.pdf?ua=1, accessed 20 Jul 2020).
Wells JC, Sawaya AL, Wibaek R, Mwangome M, Poullas MS, Yajnik CS, et al. The double burden of malnutrition: aetiological pathways and consequences for health. Lancet. 2020;395:75–88.
Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet.2020;395:65–74.
Peng W, Mu Y, Hu Y, Li B, Raman J, Sui Z. Double burden of malnutrition in the Asia-Pacific region- a systematic review and meta-analysis. J Epidemiol Glob Health. 2020;10:16–27.
Mahmudiono T, Segalita C, Rosenkranz RR. Socio-ecological model of correlates of double burden of malnutrition in developing countries: a narrative review. Int J Environ Res Public Health. 2019;16:3730.
Kosaka S, Umezaki M. A systematic review of the prevalence and predictors of the double burden of malnutrition within households. Br J Nutr. 2017;117:1118–27.
Caleyachetty R, Thomas GN, Kengne AP, Echouffo-Tcheugui JB, Schilsky S, Khodabocus J, et al. The double burden of malnutrition among adolescents: analysis of data from the global school-based student health and health behavior in school-aged children surveys in 57 low- and middle-income countries. Am J Clin Nutr. 2018;108:414–24.
Williams AM, Guo J, Addo OY, Ismaily S, Namaste SML, Oaks BM, et al. Intraindividual double burden of overweight or obesity and micronutrient deficiencies or anemia among women of reproductive age in 17 population-based surveys. Am J Clin Nutr. 2020;112:468S–77S.
Engle-Stone R, Guo J, Ismaily S, Addo OY, Ahmed T, Oaks B, et al. Intraindividual double burden of overweight and micronutrient deficiencies or anemia among preschool children. Am J Clin Nutr. 2020;112:478S–87S.
Ruderman NB, Schneider SH, Berchtold P. The “metabolically-obese,” normal-weight individual. Am J Clin Nutr. 1981;34:1617–21.
Klitgaard HB, Kilbak JH, Nozawa EA, Seidel AV, Magkos F. Physiological and lifestyle traits of metabolic dysfunction in the absence of obesity. Curr Diab Rep. 2020;20:17.
Heshmat R, Hemati Z, Payab M, Hamzeh SS, Motlagh ME, Shafiee G, et al. Prevalence of different metabolic phenotypes of obesity in Iranian children and adolescents: the CASPIAN V study. J Diabetes Metab Disord. 2018;17:211–21.
Li YP, Yang XG, Zhai FY, Piao JH, Zhao WH, Zhang J, et al. Disease risks of childhood obesity in China. Biomed Environ Sci. 2005;18:401–10.
Ramachandran A, Snehalatha C, Yamuna A, Murugesan N, Narayan KM. Insulin resistance and clustering of cardiometabolic risk factors in urban teenagers in southern India. Diabetes Care. 2007;30:1828–33.
Garg P, Kaur S, Gupta D, Osmond C, Lakshmy R, Sinha S, et al. Variability of thinness and its relation to cardiometabolic risk factors using four body mass index references in school children from Delhi, India. Indian Pediatr. 2013;50:1025–32.
Ministry of Health and Family Welfare, Government of India, UNICEF, Population Council. Comprehensive national nutrition survey 2016–2018. national health mission, 2019. https://nhm.gov.in/showfile.php?lid=712. Accessed 20 Jul 2020.
National Family Health Survey 4. International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015–16: India. Mumbai; International Institute of Population Science; 2015–16.
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128:S213–56.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33:S62–9.
Leite HP, Rodrigues da Silva AV, de Oliveira Iglesias SB, Koch Nogueira PC. Serum albumin is an independent predictor of clinical outcomes in critically ill children. Pediatr Crit Care Med. 2016;17:e50–7.
Kim S, McClave SA, Martindale RG, Miller KR, Hurt RT. Hypoalbuminemia and clinical outcomes: what is the mechanism behind the relationship? Am Surg. 2017;83:1220–7.
Ogata E, Asahi K, Yamaguchi S, Iseki K, Sato H, Moriyama T, et al. Low fasting plasma glucose level as a predictor of new-onset diabetes mellitus on a large cohort from a Japanese general population. Sci Rep. 2018;8:13927.
Serbis A, Giapros V, Galli-Tsinopoulou A, Siomou E. Metabolic syndrome in children and adolescents: is there a universally accepted definition? Does it matter? Metab Syndr Relat Disord. 2020 Aug 13. https://doi.org/10.1089/met.2020.0076. Epub ahead of print.
Ataie-Jafari A, Heshmat R, Kelishadi R, Ardalan G, Mahmoudarabi M, Rezapoor A, et al. Generalized or abdominal obesity: which one better identifies cardiometabolic risk factors among children and adolescents? The CASPIAN III study. J Trop Pediatr. 2014;60:377–85.
González-Gil EM, Cadenas-Sanchez C, Santabárbara J, Bueno-Lozano G, Iglesia I, Gonzalez-Gross M, et al. Inflammation in metabolically healthy and metabolically abnormal adolescents: the HELENA study. Nutr Metab Cardiovasc Dis. 2018;28:77–83.
Martin L, Oepen J, Reinehr T, Wabitsch M, Claussnitzer G, Waldeck E, et al. Ethnicity and cardiovascular risk factors: evaluation of 40,921 normal-weight, overweight or obese children and adolescents living in Central Europe. Int J Obes (Lond). 2015;39:45–51.
Kloppenborg JT, Fonvig CE, Nielsen TRH, Mollerup PM, Bøjsøe C, Pedersen O, et al. Impaired fasting glucose and the metabolic profile in Danish children and adolescents with normal weight, overweight, or obesity. Pediatr Diabetes. 2018;19:356–65.
National Heart Lung and Blood Institute. What is energy balance? Balance Food and Activity. Available from: https://www.nhlbi.nih.gov/health/educational/wecan/healthy-weight-basics/balance.htm#:~:text=What%20is%20Energy%20Balance%3F,physical%20activity%20is%20ENERGY%20OUT. Accessed 13 Nov 2020.
Sachdev HPS. Undersized Indian children: nutrients-starved or hungry for development? Proc Indian Natn Sci Acad. 2018;84:867–75.
Bray GA, Bouchard C. The biology of human overfeeding: a systematic review. Obes Rev. 2020;21:e13040.
Most J, Tosti V, Redman LM, Fontana L. Calorie restriction in humans: an update. Ageing Res Rev. 2017;39:36–45.
Kraus WE, Bhapkar M, Huffman KM, Pieper CF, Krupa Das S, Redman LM, et al. 2 years of calorie restriction and cardiometabolic risk (CALERIE): exploratory outcomes of a multicentre, phase 2, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:673–83.
Eckel RH, Jakicic JM, Ard JD, de Jesus J, Miller NH, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S76–99.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines circulation. Circulation 2019;140:e596–646.
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;139:e1082–143.
American Diabetes Association. 3. prevention or delay of type 2 diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S29–33.
Chooi YC, Ding C, Chan Z, Choo J, Sadananthan SA, Michael N, et al. Moderate weight loss improves body composition and metabolic function in metabolically unhealthy lean subjects. Obes (Silver Spring). 2018;26:1000–7.
Kelishadi R, Hashemipour M, Sarrafzadegan N, Mohammadifard N, Alikhasy H, Beizaei M, et al. Effects of a lifestyle modification trial among phenotypically obese metabolically normal and phenotypically obese metabolically abnormal adolescents in comparison with phenotypically normal metabolically obese adolescents. Matern Child Nutr. 2010;6:275–86.
Van Hulst A, Ybarra M, Mathieu ME, Benedetti A, Paradis G, Henderson M. Determinants of new onset cardiometabolic risk among normal weight children. Int J Obes (Lond). 2020;44:781–9.
Nier A, Brandt A, Baumann A, Conzelmann IB, Özel Y, Bergheim I. Metabolic abnormalities in normal weight children are associated with increased visceral fat accumulation, elevated plasma endotoxin levels and a higher monosaccharide intake. Nutrients. 2019;11:652.
India State-Level Disease Burden Initiative Collaborators. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 2017;390:2437–60.
Kuriyan R, Selvan S, Thomas T, Jayakumar J, Lokesh DP, Phillip MP, et al. Body composition percentiles in Urban South Indian children and adolescents. Obes (Silver Spring). 2018;26:1629–36.
D’Angelo S, Yajnik CS, Kumaran K, Joglekar C, Lubree H, Crozier SR, et al. Body size and body composition: a comparison of children in India and the UK through infancy and early childhood. J Epidemiol Comm Health. 2015;69:1147–53.
National Sample Survey Office. Nutritional Intake in India: 2011–12, NSS 68th Round. New Delhi, India: National Statistical Organization. Government of India; 2014.
Parks EJ, Hellerstein MK. Carbohydrate-induced hypertriacylglycerolemia: historical perspective and review of biological mechanisms. Am J Clin Nutr. 2000;71:412–33.
Vos MB, Kaar JL, Welsh JA, Van Horn LV, Feig DI, Anderson CAM, et al. Added sugars and cardiovascular disease risk in children: a scientific statement from the American Heart Association. Circulation. 2017;135:e1017–34.
WHO, WFP, UNSCN, UNICEF. Community-based management of severe acute malnutrition. A joint statement by the World Health Organization, World Food Programme, United Nations Standing Committee on Nutrition, United Nations Children’s Fund. Geneva, World Health Organization; 2007. Available from: http://www.who.int/nutrition/publications/severemalnutrition/9789280641479/en/. Accessed 20 Aug 2020.
World Health Organization. WHO Recommendations on antenatal care for a positive pregnancy experience. Geneva: World Health Organization; 2016. Available from: https://www.who.int/reproductivehealth/publications/maternal_perinatal_health/anc-positive-pregnancy-experience/en/. Accessed 20 Aug 2020.
von Grebmer K, Bernstein J, Mukerji R, Patterson F, Wiemers M, Ní Chéilleachair R, et al. 2019 Global Hunger Index: The Challenge of Hunger and Climate Change. Bonn: Welthungerhilfe; and Dublin: Concern Worldwide, 2019. Available at: https://www.globalhungerindex.org/pdf/en/2019.pdf. Accessed on 23 Aug 2020.
United Nations. Sustainable development Goals. Goal 2: Zero Hunger. Available at: https://www.un.org/sustainabledevelopment/hunger. Accessed 23 August, 2020.
Acknowledgements
HSS and AVK are recipients of the Wellcome Trust/Department of Biotechnology India Alliance Clinical/Public Health Research Centre Grant # IA/CRC/19/1/610006. AVK is also supported by the India Alliance through their Margdarshi Fellowship.
Funding
The CNNS was conducted by the Ministry of Health and Family Welfare, Government of India, and the UNICEF, with financial support from the Mittal Foundation. These secondary analyses and paper were not supported by any specific funding.
Data sharing and declarationThe Ministry of Health and Family Welfare (MoHFW), Government of India owns the Comprehensive National Nutrition Survey data. The data used in this paper were released for public use by the MoHFW and United Nations Children Fund, India Country Office. The code book and the analytic code can be made available upon reasonable request to the corresponding author(s).
Author information
Authors and Affiliations
Contributions
HSS conceived the idea, guided the analysis and drafted the manuscript. AP conducted all statistical analyses. AVK provided analytic insight for the National Sample Survey Office dietary consumption data. All authors were involved at every iteration of analyses and drafting, and approved the final paper. All authors had access to raw data.
Corresponding authors
Ethics declarations
Conflict of interest
HSS designed the draft protocol of the CNNS with consultancy support from the UNICEF, India. HSS, AS, UK and AVK were members of the Technical Advisory Committee of the CNNS, constituted by the Ministry of Health and Family Welfare of the Government of India, to oversee its conduct and analysis. HSS is a member of the World Health Organization Nutrition Guidance Expert Advisory Subgroup on Diet and Health and member of Expert Groups of the Ministry of Health and Family Welfare on Nutrition and Child Health. AS, RA, SR and AP were involved in the CNNS study implementation and main analyses. There were no other conflicts to declare.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Population Council’s International Review Board (New York, USA) and ethics committee of Post Graduate Institute of Medical Education and Research (Chandigarh, India). No separate ethical approval was required or taken for this secondary analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sachdev, H.S., Porwal, A., Sarna, A. et al. Intraindividual double-burden of anthropometric undernutrition and “metabolic obesity” in Indian children: a paradox that needs action. Eur J Clin Nutr 75, 1205–1217 (2021). https://doi.org/10.1038/s41430-021-00916-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-021-00916-3
This article is cited by
-
Is iron status associated with markers of non-communicable disease in adolescent Indian children?
European Journal of Clinical Nutrition (2023)
-
Intraindividual double burden of malnutrition among women (15–49 years) in India, Myanmar, and Nepal: evidence from the recent Demographic and Health Surveys
European Journal of Clinical Nutrition (2023)
-
Body composition from birth to 2 years
European Journal of Clinical Nutrition (2023)
-
Dyslipidemia Among Overweight and Obese Children in Jharkhand: A Hospital-Based Study
Indian Pediatrics (2023)
-
Comparison of Weight for Height and BMI for Age for Estimating Overnutrition Burden in Under-Five Populations With High Stunting Prevalence
Indian Pediatrics (2023)