Abstract
Background/Objectives
Unsaturated fats, fibre-rich foods and polyphenols are distinctive features of a traditional Mediterranean diet and have pleiotropic properties possibly contributing to reduce the long-term risk of non-communicable diseases and mortality associated with this diet. We aimed to evaluate whether changes over time in dietary fats, fibre and polyphenols consumption are associated with modifications in cardiovascular disease (CVD) risk factors.
Methods
The analytic sample consists of a sub-cohort of 2023 men and women enrolled in the Moli-sani Study (n = 24,325). Dietary and health data were obtained both at baseline (2005–2010) and at re-examination (2017–2020). The exposures were changes in dietary fats, fibre and polyphenols consumption measured after 12.7 years (median), and the outcome was change in a composite score including 13 modifiable CVD risk factors (e.g., blood lipids, C-reactive protein), measured both at enrolment and after the 12.7 years period.
Results
In multivariable-adjusted analysis including lifestyles, sociodemographic and clinical factors, an incremental intake of the ratio of monounsaturated to saturated fats or of fibre was associated with a reduction in the composite score of CVD risk factors (β = −0.086; 95%CI −0.150, −0.021 and β = −0.051; 95%CI −0.091, −0.012, respectively). Change in polyphenol intake was not associated with a substantial variation in the CVD risk score (p = 0.15).
Conclusions
An incremental consumption over time of monounsaturated versus saturated fats and of fibre was associated with an improvement in modifiable CVD risk factors as reflected by a composite score.
Similar content being viewed by others
Introduction
Improvement of overall diet quality is a key public health strategy to prevent chronic diseases [1], and is supported by a large body of evidence indicating that healthful diets are associated with lower risk of non-communicable diseases [2, 3] and premature death [4].
Studies evaluating whether improvement in overall diet quality might have long-term advantages on health are scarce [5, 6], and were mainly focused on changes in intermediate phenotypes that predispose to higher health risk [7, 8], while a few have related incremental improvement in the overall diet quality with disease occurrence or mortality [5, 9, 10].
The traditional Mediterranean diet (MD) has long been acknowledged as one of the healthiest diets, capable of reducing the risk of developing chronic diseases and improve survival in numerous cohorts [11, 12], possibly through a favourable modulation of several cardiovascular and cerebrovascular disease (CVD) risk factors [13] and inflammatory markers [14].
The MD emphasizes the consumption of plant-based foods that are natural sources of antioxidants and fibre, while limiting the intake of saturated fats (SFA) and trans fats, animal-derived proteins, and added/refined sugars [1]. By contrast, this eating model is characterized by the large use of dietary sources of unsaturated fats, i.e. monounsaturated (MUFA) and polyunsaturated (PUFA) fats, with energy from fat representing up to 40% of the total calories eaten daily [15], and extra-virgin olive oil being the main source of MUFA.
Unsaturated fats are likely one mechanism for reducing inflammation, optimizing cholesterol, and other risk factors, and diets rich in these fats were shown to reduce total and cause-specific mortality risk [16], whereas SFA were found to impact adversely on health [17].
The health advantages deriving from a diet rich in fibre are well documented in a number of observational [18] and intervention studies [19]. Polyphenols are bioactive compounds largely present in in plant foods and plant-derived beverages [20], and there is robust evidence supporting their beneficial effects against type 2 diabetes, CVD and cancer [21,22,23,24,25,26], possibly through their well-recognized anti-inflammatory and antioxidative properties [27].
While the association of incremental diet quality changes, as measured by dietary indices, with intermediate phenotypes is well-documented, no prior investigations have seen whether improving adherence to main components of a healthy diet possibly associates with changes in modifiable CVD risk factors. Therefore, we sought to evaluate whether changes in some distinctive features of a traditional MD (i.e., dietary fats, fibre and polyphenols) are associated with modifications in several modifiable CVD risk factors, as reflected by a composite score of established CVD risk factors, in a sub-cohort of 2023 adults from the larger Moli-sani study in Italy.
Methods
Study population
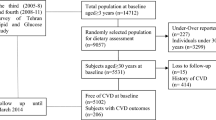
The Moli-sani Study is a large population-based cohort study that in 2005–2010 randomly recruited 24,325 men and women aged ≥ 35 years from the adult general population of the Molise region, a central-southern area of Italy with the aim of investigating genetic and environmental risk factors in the onset of cardiovascular, cerebrovascular and cancer diseases. Exclusion criteria were pregnancy at the time of recruitment, disturbances in mental or decision-making impairments, current poly-traumas or coma, or refusal to sign the informed consent. Details of the study are provided elsewhere [28]. In 2017–2020, the first 5438 residents in Campobasso (the chief town of the Molise region), previously recruited in the Moli-sani study, were re-contacted for a full re-examination, including dietary, lifestyle and psychological assessments, along with medical examination and blood collection. Of them, 3896 accepted (acceptance rate = 71.6%) and 2581 underwent the re-examination from May 2017 until the beginning of March 2020; the recruitment of the remaining 1315 participants was not completed since the COVID-19 outbreak. The final sample was of 2023 individuals (Supplementary Fig. 1). The Moli-sani Study complies with the Declaration of Helsinki and was approved by the Ethics Committee of the Catholic University Medical School in Rome, Italy. The re-examination of the cohort was granted the approval of the Ethics Committee of the IRCCS Neuromed, Pozzilli (IS), Italy. All participants provided written informed consent both at baseline and at re-examination.
Dietary assessment
Dietary intake during the year before enrolment was assessed at baseline (2005–2010) and follow-up (2017–2020) by an interviewer-administered semi-quantitative EPIC food frequency questionnaire (FFQ) validated and adapted to the Italian population [29].
The Nutrition Analysis of Food frequency questionnaire (NAF) [30] was used to convert questionnaire dietary data into frequencies of consumption and average daily quantities of foods (g/d) and energy intake (Kcal/d). The NAF software was linked to the Italian food composition tables for energy assessment [31].
The FFQ includes a total of 188-food items that were classified into 45 predefined food groups on the basis of similar nutrient characteristics or culinary usage.
Adherence to the traditional MD was defined according to the MD Score (MDS) developed by Trichopoulou et al. [32], ranging from 0 to 9 (the latter reflecting maximal adherence). Assessment of MDS at re-examination was made by using the sex-specific cut-offs for each food group as evaluated at baseline.
Intake of total and sub-types of fats (SFA, MUFA, and PUFA) was considered as percentage of the total energy intake or as the ratio of MUFA to SFA, used as a proxy of olive oil consumption. Total dietary fibre consumption from various food sources (e.g., bread, pasta, vegetables) was defined as g/d.
The Phenol-Explorer database [33] was used to estimate the total intake of polyphenols in the diet of participants. This is the most complete database currently available for polyphenol content. Both at baseline and follow-up, the individual polyphenol intake was calculated by multiplying the content of each polyphenol in a particular food item (mg/g) by the daily consumption of this food item (g/d) and then summing the product across all food items. Total polyphenol intake resulted as the sum of all individual polyphenol intakes.
Assessment of covariates
Data on socio-demographic, lifestyle and clinical variables were collected through an interviewer-administered questionnaire. Educational level was based on the highest qualification attained and was categorized as up to lower secondary (≤ 8 years), upper secondary (8–13 years) and postsecondary (>13 years). Housing tenure was defined as rented, 1 dwelling ownership or > 1 dwelling ownership. Present occupation was categorized as professional/managerial, skilled non-manual, skilled manual, semi-skilled/unskilled and unemployed/unclassified. Marital status was grouped as married/in couple, separated/divorced, single and widowed. Subjects were classified as never-smokers, current smokers, or former smokers (reported not having smoked at all over the previous 12 months or more) at baseline and at follow-up. Physical exercise was expressed as daily energy expenditure in metabolic equivalent task-hours (MET-h/d). Participants were considered to have diabetes, hypertension or dyslipidaemia if they were receiving disease-specific drugs. History of cardiovascular disease (angina, myocardial infarction, peripheral artery disease, revascularization procedures and cerebrovascular events) was self-reported and confirmed by medical records and therapy. History of cancer was self-reported and confirmed by medical records.
Blood collection and measurement of biomarkers
Serum lipids (total cholesterol, HDL-cholesterol, triglycerides) and blood glucose were assayed by enzymatic reaction methods using an automatic analyzer (ILab 350, Instrumentation Laboratory, Milan, Italy at baseline, and ILab Aries at re-examination). Quality control (high and low levels) for lipids was obtained by a commercial standard provided by IL and an in-house serum standard pool. Serum high sensitivity C-reactive protein (CRP) was measured by a particle-enhanced immunoturbidimetric assay (ILab 350, Instrumentation Laboratory, Milan, Italy at baseline, and ILab Aries at re-examination).
Hemochromocytometric analysis was performed by cell count (Coulter HMX, Beckman Coulter, IL Milan, Italy at baseline, and Siemens ADVIA 120 at re-examination) within 3 h from blood collection.
Blood pressure was measured by an automatic device (OMRON-HEM-705CP at baseline, and OMRON-HEM-FL31 at re-examination) three times on the non-dominant arm and the average of the last two values was taken as the BP. Measurements were made in a quiet room with comfortable temperature with the participants lying down for at least 5 min. Body weight and height were measured with a column mechanical scale with telescopic measuring rod (SECA 700, Hamburg, Germany), in subjects wearing no shoes and only light indoor clothing. Body mass index (BMI) was calculated as kg/m2. Waist circumferences were measured according to the National Institutes of Health, Heart, Lung, and Blood Guidelines [34]. The same procedures were used for collecting data during the re-examination of the cohort.
Computation of the composite score of CVD risk factors
To appraise participants’ CVD risk both at baseline and at re-examination, we derived a composite score that summarized levels of 13 modifiable risk factors reflecting different underlying pathways to CVD incidence and progression, that is systolic and diastolic blood pressure, heart rate, total serum cholesterol, HDL-cholesterol, triglycerides, blood glucose, BMI, waist-to-hip ratio, creatinine, CRP, white blood cell count, granulocyte-to lymphocyte ratio (GLR). Participants were categorized into sex-specific deciles of each marker level. For all components, higher levels (i.e., > Q6) scored increasing positively (from 1 to 4) while lower levels (i.e., < Q5) got negative scoring (from −1 to −4). Being in the deciles 5 or 6 got zero points. For HDL- cholesterol we reversed the scoring.
The composite CVD risk factors score resulted from summing the 13 individual scores and theoretically ranging from −52 to 52, with increased values reflecting worse cardiovascular health. For analyses purposes, this composite score was modelled as a continuous variable (1 standard deviation increase).
Statistical analysis
In this study, the exposures were changes in the intake of fats, fibre and polyphenols measured after a 12.7 years period, and the outcomes were changes in the composite score of CVD risk factors measured after the same 12.7 years period. We computed changes in the variables of exposure and outcome at individual level by subtracting values at baseline from those at 12.7 years follow-up.
Descriptive baseline characteristics are reported as mean and standard deviation (SD) or percentage.
Multivariable linear regression analysis (PROC REG in SAS) was used to estimate the relation between changes in the consumption of dietary fats, fibre and polyphenols (independent variables, standardised to one SD) with changes in the score of CVD risk factors (standardised to one SD) and results were expressed as regression coefficients (β) with 95% confidence interval (95%CI).
On the basis of previous literature and biological plausibility, the following 3 models were fitted: Model 1 was adjusted for age, sex, duration of follow-up, baseline energy intake and changes in energy intake, and baseline levels of each dietary exposure and the composite score of CVD risk factors; Model 2 was adjusted as in Model 1 and further controlled for baseline socioeconomic status (i.e. marital status, educational level, housing, occupational class), history of CVD (at baseline and follow-up), history of cancer (at baseline and follow-up), diabetes (at baseline and follow-up), hypertension (at baseline and follow-up), dyslipidaemia (at baseline and follow-up), baseline physical activity and changes in physical activity and smoking status (at baseline and follow-up); Model 3 was adjusted as in Model 2 and including changes in alcohol intake (g/d), energy from carbohydrates and protein, and all the listed dietary variables simultaneously.
Distribution of missing values was as follows: baseline CVD = 27; CVD at follow up = 43; baseline cancer = 4; cancer at follow up = 4; baseline diabetes = 24; diabetes at follow-up = 15; baseline hypertension = 21; hypertension at follow up = 5; baseline dyslipidaemia = 82; dyslipidaemia at follow up = 57; baseline smoking habit = 3; marital status = 1; baseline physical exercise = 1; physical exercise at follow up = 19.
We used a multiple imputation technique (SAS PROC MI, followed by PROC MIANALYZE) to maximize data availability for all variables, avoid bias introduced by not-at-random missing (MNAR) data patterns and achieve robust results over different simulations (n = 10 imputed datasets). Statistical tests were two-sided, and P values of less than 0.05 were considered to indicate statistical significance. Data analysis were generated using SAS/STAT software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
We analysed data on 2023 men and women with an average baseline age of 54.5 years (SD ± 8.8 years, range 35–79 years).
Distribution of baseline age and sex-standardized CVD risk factors in the Moli-sani participants was comparable to that from the Italian Health Examination Survey OEC/HES (2008–2012) [35], except for systolic blood pressure, that was higher in the Moli-sani study (Supplementary Table 1). Therefore, the median cut off of the individual CVD risk factors reflect neutral risk.
Over 12.7 years of follow-up (interquartile range: 12.3–13.3 years), energy from fat increased from 33.1% (SD ± 5.6) to 34.9% (SD ± 5.3) and the same upward trend were observed for other subtypes of fat, with the exception of the MUFA-to-SFA ratio, that was otherwise decreased, as well as dietary fibre and total polyphenols (Table 1).
Overall, the composite score of CVD risk factors significantly lowered from 0.01 to −0.05 (Table 1).
Regarding individual biomarkers, relevant decreases were observed for total blood cholesterol and systolic and diastolic blood pressure, while major increases pertained to blood glucose levels, waist-to-hip ratio and the ratio of granulocytes to lymphocytes (Table 1).
Characteristics of the study participants at baseline and follow-up are reported in Table 2. Among lifestyles, data indicate lower prevalence of smokers and reduced levels of physical activity after 12.7 years as compared to baseline data; an increase in the prevalence of all chronic health conditions was also documented, likely as a consequence of aging.
In multivariable-adjusted analyses, an increase in the percentage of energy from total fat or SFA was directly associated with the composite score of CVD risk factors (β = 0.104; 95% CI 0.030, 0.179 and β = 0.103; 95%CI 0.034, 0.172, respectively; Table 3, Models 3).
Increases in the amount of MUFA on SFA inversely associated with the CVD risk factors score (β = −0.086; 95%CI −0.150, −0.021; Table 3, Model 3), while increases in energy from MUFA or PUFA taken individually were not associated with the outcome under study.
Higher intake of dietary fibre, but not polyphenols, was inversely associated with the composite score of CVD risk factors (β = −0.051; 95% CI −0.091, −0.012 and β = −0.053; 95%CI −0.124, 0.018; Table 3, Models 3; respectively). Similar results were observed when changes in dietary exposures were modelled as tertiles (Fig. 1).
Regression coefficient β with 95% confidence interval (95%CI) obtained from the linear regression analysis adjusted for age, sex, duration of follow-up, baseline marital status, educational level, housing, occupational class, baseline energy intake and changes in energy intake, history of CVD (at baseline and follow-up), history of cancer (at baseline and follow-up), diabetes (at baseline and follow-up), hypertension (at baseline and follow-up), dyslipidaemia (at baseline and follow-up), baseline physical activity and changes in physical activity, smoking status (at baseline and follow-up), baseline levels of each the dietary exposure and initial levels of the score of cardiovascular disease risk factors, changes in alcohol intake (g/d), energy from carbohydrates and protein, and included all the listed dietary variables simultaneously.
Discussion
The health advantages of an MD are well-documented in a variety of population cohorts [11, 12, 32] and also supported by RCTs [36, 37]; this diet is characterized by olive oil as a major source of unsaturated fat and high content of fibre and polyphenols, all acting on different, though complementary, health-promoting pathways.
In the present study, we sought to examine the associations of changes in key features of a traditional MD with concurrent changes in in modifiable CVD risk factors over a 12.7-year period.
The key findings of our analyses were that participants who have increased their optimal ratio of MUFA to SFA, that can be considered as a marker of olive oil consumption, were more likely to experience an improvement in a composite score of modifiable CVD risk factors; consistently, an incremental intake of energy from saturated fat was associated with an increase in this score.
A traditional MD has lipid-lowering effects that have been proposed among key biological mechanisms through which this diet likely exerts its favourable effects on health [38].
The role of dietary fats on health has been long studied as a modifiable factor in the prevention and treatment of several non-communicable diseases, as well as mortality risk [39, 40].
Extra-virgin olive oil is the major dietary source of MUFA in the Mediterranean diet and several studies showed its beneficial effects in the development and progression of diseases associated with chronic low-grade inflammation [36], as well as its positive association with survival [41].
A high ratio of MUFA to SFA, which is a proxy of olive oil consumption at least in Mediterranean populations, resulted in a significant risk reduction for all-cause and cardiovascular mortality in numerous prospective cohorts worldwide [42], and was also found to be a top contributing factor to increased survival associated with an MD among a population of elderly Italians recruited in the same Moli-sani cohort [43]. In the last years, the PREDIMED dietary intervention trial on over 7000 Spanish individuals at high CVD risk showed that Mediterranean diets enriched with extra-virgin olive oil or nuts are effective in reducing the risk of developing CVD, cancer and diabetes compared to a standard low-fat diet [36, 44, 45]. Also, participants assigned to the MD arms of the trial experienced lower cellular and plasma concentrations of inflammatory markers related to atherosclerosis [46], as well as improvements in lipid profile and blood pressure [47].
Our findings on a direct association between increases in total or saturated fat intake with the CVD risk factors score support the notion that limiting SFA in the diet, also by preferring vegetable sources of cooking fat (e.g., olive oil over butter), should be prioritized for reduction of non-communicable disease risk [48].
Findings from our longitudinal analyses also point to an inverse association between an increase in dietary fibre and CVD risk factors; this is in line with several observational studies showing that a large dietary share of fibre is associated with lower long-term risk of developing CVD, diabetes and cancer, as well as reducing mortality risk [49].
Fibre can positively impact on cardiovascular health by exerting beneficial metabolic effects that include reduction of cholesterol levels, improved control of blood glucose levels, and better regulation of body weight [50].
Unexpectedly, in our analyses an increase in dietary polyphenols over time was not associated with an improvement in cardiovascular risk factors. This finding is in contrast with a large body of epidemiological evidence indicating that a diet rich in polyphenols is associated with reduced risk of non-communicable diseases [51, 52], especially cardiovascular disease [24, 53], possibly through a favourable modulation of intermediate phenotypes that ultimately translate into lower disease risk.
Yet, it is worth noting that our study used a limited number of blood markers of inflammation, and these may not necessarily reflect inflammation in tissue compartments or response to inflammatory challenges [54]; this possibly explains the lack of an association between increases in polyphenol intake and the CVD risk factors score in our population.
Strengths and limitations
To the best of our knowledge, this is the first study evaluating in an adult general population longitudinal changes in key components of a traditional MD, and subsequently assessing their association with changes in CVD risk factors.
The present study has several strengths which include a prospective design, a second dietary assessment over 12.7 years by a validated dietary questionnaire, and comprehensive information on a wide range of potential covariates.
However, there are several limitations that need to be considered. First, these are observational data which limit causal inference; second, although we have used Phenol-Explorer, which is the most comprehensive food composition database on polyphenols to date [33], measurement error in collecting and estimating dietary polyphenol intake remains an issue. Another critical point is represented by the effect of seasonality, storage and cooking process which is not always considered.
Also, we did not explore the different dietary sources of fats, that may have different effects on human health. A further weakness is the use of a limited number of inflammatory markers to evaluate low-grade inflammation, although a composite score based on these markers was found to be predictive of health outcomes [55].
Further investigations using biomarkers, such as human plasma or urine samples, may be necessary for better understanding of the role in human health of polyphenols, fibre and fats consumed within an MD.
Also, we acknowledge that the intake of total SFAs without considering specific types of SFAs and their food sources is insufficient, since food composition results in different physiological effects.
Finally, it might be that dietary changes observed in this cohort can be partly explained by regression to the mean [56] or changes in disease status, and this should be taken into account when interpreting our results.
Conclusions
In a prospective cohort of Italian adults, an incremental intake of monounsaturated fats and fibre over a 12.7-year period is associated with improvement in modifiable CVD risk factors at the end of the subsequent 12.7 years. Findings from this longitudinal study shed light on the role of key components of a traditional MD acting on concurrent changes in established markers of cardiovascular risk, which possibly predispose to lower the long-term risk of developing chronic disease and mortality. Results from the present study may be used to plan novel strategies aimed to improve population health through dietary recommendations, namely by ensuring adequate consumption of fibre-rich foods and optimal food sources of unsaturated fats.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author. The data are stored in an institutional repository (https://repository.neuromed.it) and access is restricted by the ethical approvals and the legislation of the European Union.
References
Dietary Guidelines Advisory Committee. 2020. Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and the Secretary of Health and Human Services. U.S. Department of Agriculture, Agricultural Research Service, Washington, DC.
Schulze MB, Martínez-González MA, Fung TT, Lichtenstein AH, Forouhi NG. Food based dietary patterns and chronic disease prevention. BMJ 2018;361:k2396.
Bruins MJ, Van Dael P, Eggersdorfer M. The role of nutrients in reducing the risk for noncommunicable diseases during aging. Nutrients 2019;11:85.
Wang DD, Li Y, Afshin A, Springmann M, Mozaffarian D, Stampfer MJ, et al. Global improvement in dietary quality could lead to substantial reduction in premature death. J Nutr. 2019;149:1065–74.
Ley SH, Pan A, Li Y, Manson JE, Willett WC, Sun Q, et al. Changes in overall diet quality and subsequent type 2 diabetes risk: Three U.S. prospective cohorts. Diabetes Care. 2016;39:2011–8.
Xu Z, Steffen LM, Selvin E, Rebholz CM. Diet quality, change in diet quality and risk of incident CVD and diabetes. Public Health Nutr. 2020;23:329–38.
Fung TT, Pan A, Hou T, Chiuve SE, Tobias DK, Mozaffarian D, et al. Long-term change in diet quality is associated with body weight change in men and women. J Nutr. 2015;145:1850–6.
Kang M, Boushey CJ, Shvetsov YB, Setiawan VW, Paik HY, Wilkens LR, et al. Changes in diet quality and body weight over 10 years: The Multiethnic Cohort Study. Br J Nutr. 2021;126:1389–97.
Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, et al. Changes in diet quality scores and risk of cardiovascular disease among us men and women. Circulation 2015;132:2212–9.
Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, et al. Association of changes in diet quality with total and cause-specific mortality. N. Engl J Med. 2017;377:143–53.
Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17:2769–82.
Dinu M, Pagliai G, Casini A, Sofi F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. 2018;72:30–43.
Grosso G, Mistretta A, Frigiola A, Gruttadauria S, Biondi A, Basile F, et al. Mediterranean diet and cardiovascular risk factors: a systematic review. Crit Rev Food Sci Nutr. 2014;54:593–610.
Bonaccio M, Cerletti C, Iacoviello L, de Gaetano G. Mediterranean diet and low-grade subclinical inflammation: the Moli-sani study. Endocr Metab Immune Disord Drug Targets. 2015;15:18–24.
Kromhout D, Keys A, Aravanis C, Buzina R, Fidanza F, Giampaoli S, et al. Food consumption patterns in the 1960s in seven countries. Am J Clin Nutr. 1989;49:889–94.
Wang DD, Li Y, Chiuve SE, Stampfer MJ, Manson JE, Rimm EB, et al. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 2016;176:1134–45.
O’Sullivan TA, Hafekost K, Mitrou F, Lawrence D. Food sources of saturated fat and the association with mortality: A meta-analysis. Am J Public Health. 2013;103:e31–4.
Reynolds AN, Diep Pham HT, Montez J, Mann J. Dietary fibre intake in childhood or adolescence and subsequent health outcomes: A systematic review of prospective observational studies. Diabetes Obes Metab. 2020;22:2460–7.
McRae MP. Dietary fiber is beneficial for the prevention of cardiovascular disease: An umbrella review of meta-analyses. J Chiropr Med. 2017;16:289–99.
Manach C, Scalbert A, Morand C, Remesy C, Jimenez L. Polyphenols: Food sources and bioavailability. Am J Clin Nutr. 2004;79:727–47.
van Dam RM, Naidoo N, Landberg R. Dietary flavonoids and the development of type 2 - diabetes and cardiovascular diseases: review of recent findings. Curr Opin Lipido. 2013;24:25–33.
Del Rio D, Rodriguez-Mateos A, Spencer JP, Tognolini M, Borges G, Crozier A. Dietary (poly)phenolics in human health: structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid Redox Signal. 2013;18:1818–92.
Grosso G, Godos J, Lamuela-Raventos R, Ray S, Micek A, Pajak A, et al. A comprehensive meta-analysis on dietary flavonoid and lignan intake and cancer risk: level of evidence and limitations. Mol Nutr Food Res. 2017;61:1600930.
Mendonça RD, Carvalho NC, Martin-Moreno JM, Pimenta AM, Lopes ACS, Gea A, et al. Total polyphenol intake, polyphenol subtypes and incidence of cardiovascular disease: The SUN cohort study. Nutr Metab Cardiovasc Dis. 2019;29:69–78.
Castro-Barquero S, Tresserra-Rimbau A, Vitelli-Storelli F, Doménech M, Salas-Salvadó J, Martín-Sánchez V, et al. Dietary polyphenol intake is associated with HDL-cholesterol and a better profile of other components of the metabolic syndrome: A PREDIMED-Plus Sub-Study. Nutrients 2020;12:689.
Tresserra-Rimbau A, Rimm EB, Medina-Remón A, Martínez-González MA, de la Torre R, Corella D, et al. Inverse association between habitual polyphenol intake and incidence of cardiovascular events in the PREDIMED study. Nutr Metab Cardiovasc Dis. 2014;24:639–47.
Steffen Y, Gruber C, Schewe T, Sies H. Mono-O-methylated flavanols and other flavonoids as inhibitors of endothelial NADPH oxidase. Arch Biochem Biophys. 2008;469:209e19.
Di Castelnuovo A, Costanzo S, Persichillo M, Olivieri M, de Curtis A, Zito F, et al. Distribution of short and lifetime risks for cardiovascular disease in Italians. Eur j Prev Cardiol. 2012;19:723–30.
Pisani P, Faggiano F, Krogh V, Palli D, Vineis P, Berrino F. Relative validity and reproducibility of a food frequency dietary questionnaire for use in the Italian EPIC centres. Int J Epidemiol. 1997;26:S152–60.
Pala V, Sieri S, Palli D, Salvini S, Berrino F, Bellegotti M, et al. Diet in the Italian EPIC cohorts: presentation of data and methodological issues. Tumori. 2003;89:594–607.
Salvini S, Parpinel M, Gnagnarella P, Maissoneuve P, Turrini A. Banca dati composizione degli alimenti per studi epidemiologici in Italia. Milano: Eur Inst Oncol. 1998. Available online: http://www.bda-ieo.it/wordpress/en/(accessed June 2022).
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl J Med. 2003;348:2599–608.
Neveu V, Perez-Jiménez J, Vos F, Crespy V, du Chaffaut L, Mennen L, et al. Phenol-Explorer: an online comprehensive database on polyphenol contents in foods. Database (Oxf). 2010;2010:bap024.
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults-The Evidence Report. National Institutes of Health. Obes Res. 1998;6:464.
The Italian Health Examination Survey OEC/HES data. Available online: https://www.cuore.iss.it/indagini/CuoreData (accessed June 2022).
Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl J Med. 2018;378:e34.
de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994;343:1454–9.
Tosti V, Bertozzi B, Fontana L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J Gerontol A Biol Sci Med Sci. 2018;73 318–26.
Crowe FL, Key TJ, Appleby PN, Travis RC, Overvad K, Jakobsen MU, et al. Dietary fat intake and risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition. Am J Clin Nutr. 2008;87:1405–13.
Guasch-Ferré M, Babio N, Martínez-González MA, Corella D, Ros E, Martín-Peláez S, et al. Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am J Clin Nutr. 2015;102:1563–73.
Guasch-Ferré M, Li Y, Willett WC, Sun Q, Sampson L, Salas-Salvadó J, et al. Consumption of Olive Oil and Risk of Total and Cause-Specific Mortality Among U.S. Adults. J Am Coll Cardiol. 2022;79:101–12.
Schwingshackl L, Hoffmann G. Monounsaturated fatty acids, olive oil and health status: a systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014;13:154.
Bonaccio M, Di Castelnuovo A, Costanzo S, Gialluisi A, Persichillo M, Cerletti C, et al. Mediterranean diet and mortality in the elderly: a prospective cohort study and a meta-analysis. Br J Nutr. 2018;120:841–54.
Mourouti N, Panagiotakos DB. The beneficial effect of a Mediterranean diet supplemented with extra virgin olive oil in the primary prevention of breast cancer among women at high cardiovascular risk in the PREDIMED Trial. Evid Based Nurs. 2016;19:71.
Salas-Salvadó J, Bulló M, Babio N, Martínez-González MÁ, Ibarrola-Jurado N, Basora J, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011;34:14–9.
Casas R, Sacanella E, Urpí-Sardà M, Corella D, Castañer O, Lamuela-Raventos RM, et al. Long-Term Immunomodulatory Effects of a Mediterranean Diet in Adults at High Risk of Cardiovascular Disease in the PREvención con DIeta MEDiterránea (PREDIMED) Randomized Controlled Trial. J Nutr. 2016;146:1684–93.
Tuttolomondo A, Simonetta I, Daidone M, Mogavero A, Ortello A, Pinto A. Metabolic and Vascular Effect of the Mediterranean Diet. Int J Mol Sci. 2019;20:4716.
Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organ; Geneva, Switzerland: 2013.
Crowe FL, Key TJ, Appleby PN, Overvad K, Schmidt EB, Egeberg R, et al. Dietary fibre intake and ischaemic heart disease mortality: the European Prospective Investigation into Cancer and Nutrition-Heart study. Eur J Clin Nutr. 2012;66:950–6.
Anderson JW, Baird P, Davis RH Jr, Ferreri S, Knudtson M, Koraym A, et al. Health benefits of dietary fiber. Nutr Rev. 2009;67:188–205.
Koch W. Dietary Polyphenols-important non-nutrients in the prevention of chronic noncommunicable diseases. A systematic review. Nutrients 2019;11:1039.
Grosso G. Effects of Polyphenol-rich foods on human health. Nutrients 2018;10:1089.
Adriouch S, Lampuré A, Nechba A, Baudry J, Assmann K, Kesse-Guyot E, et al. Prospective association between total and specific dietary polyphenol intakes and cardiovascular disease risk in the Nutrinet-Santé French Cohort. Nutrients 2018;10:1587.
Minihane AM, Vinoy S, Russell WR, Baka A, Roche HM, Tuohy KM, et al. Low-grade inflammation, diet composition and health: Current research evidence and its translation. Br J Nutr. 2015;114:999–1012.
Bonaccio M, Di Castelnuovo A, Pounis G, De Curtis A, Costanzo S, Persichillo M, et al. A score of low-grade inflammation and risk of mortality: Prospective findings from the Moli-sani study. Haematologica 2016;101:1434–41.
Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. 2005;34:215–20.
Acknowledgements
We are grateful to the population of the Molise region who enthusiastically joined the study and wish to thank the Associazione Cuore Sano ONLUS (Campobasso, Italy) for its cultural support, and the Moli-sani Study Investigators (full list available in the Supplementary Information file.). ER was supported by Fondazione Umberto Veronesi that is gratefully acknowledged. The present work has been performed in the context of the Fondazione Umberto Veronesi - IRCCS Neuromed framework agreement.
Funding
The enrolment phase of the Moli-sani Study (2005–2010) was supported by research grants from the Pfizer Foundation (Rome, Italy), the Italian Ministry of University and Research (MIUR, Rome, Italy)–Programma Triennale di Ricerca, Decreto no.1588 and Instrumentation Laboratory, Milan, Italy. The second examination of the sub-cohort of Moli-sani (2017–2020) was partially funded by the Italian Ministry of Health [grant to MB, number GR-2013–02356060] and by the Italian Medicines Agency -AIFA [grant to GdG and SC, number AIFA-2016-02364690]. The present analyses were partially supported by the Italian Ministry of Health (Ricerca corrente 2022–2024).
Author information
Authors and Affiliations
Contributions
MB and ER conceived the present study; LI, MB, ER, and ADiC contributed to its design and to interpretation of data; SC, SE and MP managed data collection; ADeC organized and performed laboratory tests; MB and ER analysed the data and drafted the manuscript; MBD, CC, GdG and LI originally inspired the Moli-sani study and critically reviewed this manuscript. All Authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ruggiero, E., Di Castelnuovo, A., Costanzo, S. et al. Incremental monounsaturated to saturated fat ratio and fibre consumption is associated with a reduction in a composite score of modifiable cardiovascular risk factors: Prospective results from the Moli-sani study. Eur J Clin Nutr 76, 1697–1704 (2022). https://doi.org/10.1038/s41430-022-01185-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-022-01185-4