Abstract
Background The biomarkers of bone turnover may be vital for early detection of bone destruction in chronic periodontitis (CP). Lately, several new biochemical markers have been applied to estimate bone homeostasis.
Objective The current review aims to evaluate the role of bone biomarkers in diagnosis and treatment outcomes of CP.
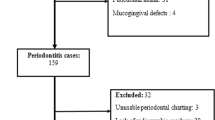
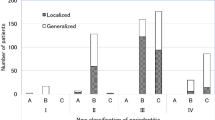
Methods Literature search was conducted in databases like Medline (PubMed) and Scopus to include original research articles related to the role of bone biomarkers in CP. About 914 documents were identified through primary search, of which 11 original research articles were included.
Results The most common bone biomarker applied in periodontal diagnosis was RANKL. Certain newer biomarkers like ICTP were also found to be useful in early detection of progressive CP.
Conclusion The bone turnover biomarkers may serve as an adjunct to the traditional methods of periodontal diagnosis. They are vital in identifying the subjects at risk for future periodontal breakdown as well as in determining the therapeutic outcomes. Their applications in periodontal diagnosis is still in the developing stage and requires further investigation. With this background, the current systematic review evaluated the role of bone-specific biomarkers in CP diagnosis and treatment outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Change history
24 June 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41432-022-0279-2
References
Strimbu K, Tavel J A. What are Biomarkers? Curr Opin HIV AIDS 2010; 5: 463-466.
Könönen E, Gursoy M, Gursoy U K. Periodontitis: A multifaceted disease of tooth-supporting tissues. J Clin Med 2019; 8: 1135.
Srivastava N, Nayak P A, Rana S. Point of care-a novel approach to periodontal diagnosis - a review. J Clin Diagn Res 2017; DOI: 10.7860/JCDR/2017/26626.10411.
Khiste S V, Ranganath V, Nichani A S, Rajani V. Critical analysis of biomarkers in the current periodontal practice. J Indian Soc Periodontol 2011; 15: 104-110.
Taba M, Kinney J, Kim A S, Giannobile W V. Diagnostic biomarkers for oral and periodontal diseases. Dent Clin North Am 2005; 49: 551-571.
Frodge B D, Ebersole J L, Kryscio R J, Thomas M V, Miller C S. Bone remodeling biomarkers of periodontal disease in saliva. J Periodontol 2008; 79: 1913-1919.
Shetty S, Kapoor N, Bondu J D, Thomas N, Paul T V. Bone turnover markers: Emerging tool in the management of osteoporosis. Indian J Endocrinol Metab 2016; 20: 846-852.
Hassan S H, El-Refai M I, Ghallab N A, Kasem R F, Shaker O G. Effect of periodontal surgery on osteoprotegerin levels in gingival crevicular fluid, saliva, and gingival tissues of chronic periodontitis patients. Dis Markers 2015; DOI: 10.1155/2015/341259.
Mishra D, Sivaram Gopalakrishnan K V, Kumar T S, Devanathan S, Misra S R. Evaluation of salivary levels of pyridinoline cross linked carboxyterminal telopeptide of type I collagen (ICTP) in periodontal health and disease. J Clin Diagn Res 2015; DOI: 10.7860/JCDR/2015/12689.6498.
Balli U, Aydogdu A, Dede F O, Turer C C, Guven B. Gingival crevicular fluid levels of sclerostin, osteoprotegerin, and receptor activator of nuclear factor-κB ligand in periodontitis. J Periodontol 2015; 86: 1396-1404.
Ochanji A A, Matu N K, Mulli T K. Association of salivary RANKL and osteoprotegerin levels with periodontal health. Clin Exp Dent Res 2017; 3: 45-50.
Doğan G E, Aksoy H, Demir T et al. Clinical and biochemical comparison of guided tissue regeneration versus guided tissue regeneration plus low-level laser therapy in the treatment of class II furcation defects: a clinical study. J Cosmet Laser Ther 2016; 18: 98-104.
Segarra-Vidal M, Guerra-Ojeda S, Vallés L S et al. Effects of photodynamic therapy in periodontal treatment: A randomized, controlled clinical trial. J Clin Periodontol 2017; 44: 915-925.
Emingil G, Gürkan A, Tervahartiala T et al. Adjunctive effects of a sub-antimicrobial dose of doxycycline on clinical parameters and potential biomarkers of periodontal tissue catabolism. Dent J (Basel) 2019; 7: 9.
Jeyasree R M, Ramakrishnan Theyagarajan V S, Navakumar M, Mani E, Santhamurthy C. Evaluation of serum and salivary alkaline phosphatase levels in chronic periodontitis patients before and after nonsurgical periodontal therapy. J Indian Soc Periodontol 2018; 22: 487-491.
Teodourescu A C, Martu I, Teslaru S et al. Assessment of salivary levels of RANKL and OPG in aggressive versus chronic periodontitis. J Immunol Res 2019; DOI: 10.1155/2019/6195258.
Borges C D, Ricoldi M S, Messora M R et al. Clinical attachment loss and molecular profile of inflamed sites before treatment. J Appl Oral Sci 2019; DOI: 10.1590/1678-7757-2018-0671.
Suthanthiran T, Annamalai S, Chellapandi S, Puthenveetil S, Dhasthaheer S, Narasimhan S. Gingival crevicular fluid levels of RANKL and OPG after placement of collagen membrane with simvastatin in the treatment of intrabony defects in chronic periodontitis. J Pharm Bioallied Sci 2019; 11(Suppl 2): S301-S304.
Jayakumar A, Rohini S, Naveen A, Haritha A, Reddy K. Horizontal alveolar bone loss: A periodontal orphan. J Indian Soc Periodontol 2010; 14: 181-185.
Kunjappu J J, Mathew V B, Hegde S, Kashyap R, Hosadurga R. Assessment of the alkaline phosphatase level in gingival crevicular fluid, as a biomarker to evaluate the effect of scaling and root planing on chronic periodontitis: An in vivo study. J Oral Maxillofac Pathol 2012; 16: 54-57.
Author information
Authors and Affiliations
Contributions
Both MY and RA conducted the data search, extraction, analysis and interpretation of data, and writing of manuscript. Both the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The authors do not have any conflict of interest.
Rights and permissions
About this article
Cite this article
Yewale, M., Agnihotri, R. The role of bone-specific biomarkers in chronic periodontitis diagnosis and treatment outcomes - a systematic review. Evid Based Dent (2022). https://doi.org/10.1038/s41432-021-0212-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41432-021-0212-0