Abstract
Purpose:
To assess Descemet’s membrane endothelial keratoplasty (DMEK) without performing a peripheral iridotomy (PI) prior to or during surgery (“PI-less DMEK”).
Materials and methods:
This retrospective study included consecutive patients that underwent PI-less DMEK by a single surgeon (E.L) between February 2016 and February 2017 at the Rabin Medical Center, a Tertiary Hospital. Intraoperative and postoperative complications were assessed.
Results:
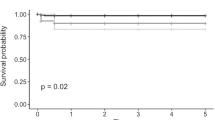
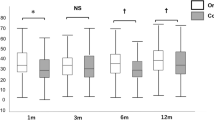
Thirty-one patients, mean age 75.9 ± 7.9 years with 58.1% female were included. Leading indications for surgery were pseudophakic bullous keratopathy (18/31) and Fuchs’ endothelial dystrophy (9/31). Preoperative best-corrected distance visual acuity was 1.13 ± 0.59 logMAR (~6/80 Snellen). For 12/31 that had postoperative endothelial cell count measurements, cell loss was 49 ± 20%. Intraoperative complications included anterior chamber (AC) hyphema during graft insertion requiring reinsertion (n = 1), and minor hyphema from the main corneal incision (n = 1). Partial slit lamp gas evacuation was performed in all patients 1.5 h postoperatively. Postoperative complications included partial graft detachment requiring rebubbling (n = 5), self-resolving minimal peripheral graft detachment (n = 5), uncontrolled intraocular hypertension requiring trabeculectomy in a patient with a history of medically controlled glaucoma (n = 1), postoperative cystoid macular edema that resolved medically (n = 1) and graft failure 5 months postoperatively (n = 1). No patients developed pupillary block. Excluding graft failure (n = 1), preoperative amblyopia (n = 2) and premature loss to follow-up (n = 1), final corrected distance visual acuity was 0.18 ± 0.14 logMAR (~20/30 Snellen) with 44.4% reaching 6/7.5 (Snellen) or more.
Conclusions:
PI-Less DMEK is a safe, technically easy, and effective modification that avoids the time and complications associated with performing a PI before or during surgery.
Similar content being viewed by others
Introduction
The emergence of Descemet’s stripping automated endothelial keratoplasty (DSAEK) and Descemet’s membrane endothelial keratoplasty (DMEK) have revolutionized the standard of care for endothelial corneal disease [1]. Specifically, despite being more technically challenging [2], DMEK has demonstrated faster rehabilitation and better visual outcomes than DSAEK [2, 3].
A common postoperative complication following DMEK is partial or complete graft detachment which has been reported to occur in up to 63% [4,5,6] and 30% [7] of cases, respectively. Consequently, in order to prolong tissue support and reduce rebubbling rates, standardized techniques make use of longer duration and larger volumes of gas in the AC compared to DSAEK and lately the use of sulfur hexafluoride gas (SF6) for tamponade instead of air were described with satisfactory outcomes [8,9,10]. Regardless of the specific type of the tamponading gas, it may lead to a dreaded complication in the form of pupillary block ocular hypertension [11]. To this end, standard techniques involve performing a prophylactic peripheral iridotomy (PI) either before [9] or during the DMEK procedure [12].
However, despite performing a prophylactic PI, pupillary block may still occur and immediate postoperative slit lamp assessment, in order to evaluate whether or not partial removal of the tamponading agent is required, is adovacted [11]. In fact, a recent report found that despite a patent iridectomy, removing some air/SF6 at the slit lamp is occasionally needed in the immediate postoperative period due to excessive gas fill of the AC [13].
Given the aforementioned study, the value of a prophylactic PI is unclear. Therefore, the purpose of this study was to describe the results of DMEK in which a prophylactic PI was not performed prior to or during surgery (PI-less DMEK).
Materials and methods
The study followed the tenets of the 2013 Declaration of Helsinki and approval from the local ethics committee of Rabin Medical Center for the use of medical records was obtained.
Patients
The charts of all consecutive patients who underwent DMEK at a tertiary center, Rabin Medical Center, Petach Tikva, Israel, between February 2016 and February 2017 were assessed. The study included consecutive patients that underwent PI-Less DMEK performed by a single experienced surgeon (E.L). Prior to our first PI-Less DMEK surgery, all DMEK cases in our institute routinely underwent a PI prior to or during DMEK surgery. Since the first case in which PI-Less DMEK was performed (in February 2016) all DMEK procedures have been performed without a PI. Thus, no specific inclusion criteria for patient selection was applied. Exclusion criteria included patients with pre-existing PIs, prior penetrating keratoplasty, prior glaucoma surgery or combined cataract extraction-DMEK surgery. All patients were pseudophakic with a posterior chamber intraocular lens and none were unicameral (aphakic or with an anterior chamber intraocular lens).
Data collection
Data collected included past medical and ophthalmic history, pre and postoperative slit lamp examination, donor cornea endothelial cell count, intraoperative complications, postoperative treatment and complications, pre and postoperative best-corrected distance visual acuity, and the results of specular microscopy. The main outcome measures were intraoperative complications, early postoperative pupillary block formation and postoperative detachment rate.
Surgical technique
All DMEK grafts were supplied and processed for DMEK by the Rabin Medical Center eye bank, using the “standardized no touch technique” for graft preparation described by Groeneveld et al. [14] 1 to 2 days preoperatively. The grafts were all stored at 4 centigrade in cold storage media (Optisol, Chiron Ophthalmics, Irvine, California) until surgery. During surgery, three limbal port incisions were made followed by Descemet’s membrane stripping under continuous automated air infusion into the AC, as previously described by us [15]. Next, a 2.4 mm limbal incision was made at 12 o’clock through which the graft was injected following its staining with Vision Blue (DORC International, Zuidland, Netherlands) for 5 min. Next, the graft was partially unfolded by tapping the corneal surface [16], its orientation was verified using Moutsouris sign [17]. Then, the partially unfolded graft was fully unfolded and centered by gentle taps on the cornea. Twenty percent SF6 gas was then injected beneath the graft, lifting it to the corneal stroma as previously described [8, 9]. Gas was injected into the AC until it was completely filled and furthermore until the surgeon observed that the iris was pushed back, indicating a proper tamponade of the AC. Subconjunctival injection of steroids and antibiotics was given and the eye was bandaged. No antibiotic or steroid creams were used in the conjunctival sac. The patients maintained a supine position for approximately 90 min outside the operating room. Then, topical oxybuprocaine (Localin, Fischer Pharmaceutical Labs., Bnei Barak, Israel), 5% povidone-iodine (Betadine, Alcon Laboratories, Fort Worth, Texas) and moxifloxacin 0.5% (Vigamox, Alcon Laboratories, Fort Worth, Texas) were instilled into the conjunctival sac, followed by partial evacuation of the gas from the AC by the same experienced surgeon. This was done on the slit lamp, by pressing the posterior lip of one of the port incisions that were made during the surgery using a blunt tipped 27 gauge cannula. The pressure was relieved from the posterior lip when the gas was reduced to fill approximately two-thirds to one half of the AC (Fig. 1). Next, pupil dilating drops tropicamide 0.5% (Mydramide, Fischer Pharmaceutical Labs., Bnei Barak, Israel), phenylephrine HCL 10% (Ephrin 10, Fischer Pharmaceutical Labs., Bnei Barak, Israel) were instilled and the patients were instructed to lie on their backs for another 30 min. Prior to discharge, the patients were examined for signs of pupillary block including a shallow AC or iris bombè, and that the intraocular pressure felt normal by means of gentle digital evaluation. Applanation tonometry at the immediate postoperative period was avoided as we believe that applanation tonometry can possibly cause graft detachment although there is no evidence of this occurring in the literature. All patients were instructed to maintain supine position for at least 50% of the time during the first 2 days following surgery. All patients were examined the next day by the same surgeon, as well as 1 week, 1 month and 3 months postoperatively and every 3 months thereafter.
At the slit lamp, partial gas evacuation is performed by pressing the posterior lip of a paracentesis with a 27 gauge blunt cannula. a The anterior chamber (AC) is completely filled with gas. b First press with the cannula evacuated some gas, not yet to the desired extent. Some fluid is noted in the AC as an inferior fluid meniscus. c Second press with the cannula evacuated some more gas, resulting in an ~50% gas fill of the AC as desired
Results
Out of 86 DMEK surgeries performed during the study period, 31 consecutive patients with a mean age of 75.9 ± 7.9 (range 61–91) of which 58.1% were female underwent PI-less DMEK and were included in this study. Leading indications for surgery were pseudophakic bullous keratopathy (18/31) and Fuchs’ endothelial dystrophy (9/31) (Table 1). Mean preoperative corrected distance visual acuity was 1.13 ± 0.59 logMAR (~6/80 Snellen). In one patient AC hyphema developed upon graft insertion. The graft was explanted, the AC was evacuated, washed and the graft was then re-inserted. Another patient had minor hyphema from the main corneal incision. There were no other intraoperative complications. One and a half hours postoperatively all patients underwent partial evacuation of gas at the slit lamp. None of the patients demonstrated pupillary block. Five patients (5/31 = 16%) required AC re-bubbling for partial graft detachment and five more patients had minimal peripheral graft detachment which resolved spontaneously.
Table 2 depicts the visual outcomes of these patients over time. Excluding one patient who developed graft failure 5 months postoperatively, one patient with premature loss to follow-up and two patients with amblyopia, the mean postoperative best-corrected distance visual acuity obtained at last visit was 0.18 ± 0.14 logMAR (~20/30 Snellen) with 12/27 (44.4%) reaching 6/7.5 (Snellen) or more. Donor preoperative endothelial cell count was 2639 ± 176 cells/mm2. Endothelial cell counts were obtained for 12/31 (39%) patients between 2 and 6 months postoperatively and averaged at 1336 ± 522 cells/mm2, representing a 49 ± 20% cell loss.
Discussion
In this study, a modified PI-less DMEK technique was described in a cohort of consecutive patients, none of which developed pupillary block or its sequela.
All patients received tropicamide 0.5% (Mydramide, Fischer Pharmaceutical Labs., Bnei Barak, Israel) and phenylephrine HCL 10% (Ephrin 10, Fischer Pharmaceutical Labs., Bnei Barak, Israel) drops for pupil dilation after partial evacuation of the gas from the AC. This assures further safety of the PI-less DMEK technique for avoiding pupillary block. The ability of the pupil to dilate well is probably necessary for assuring a safe PI-less DMEK surgery. Both DMEK and DSEK/DSAEK require the use of air or other gas to fill the AC, in order to tamponade the graft to the stroma of the host. It is generally believed by most surgeons that the duration of tamponade should be longer [12, 18] and the size of gas bubble in the AC should be bigger [2, 19] in DMEK than in DSEK/DSAEK, to reduce the postoperative detachment rate. To avoid postoperative pupillary block, surgeons combine the surgery with PI (usually performed inferiorly) either prior to surgery by Nd:YAG laser [20] or during surgery by means of intraocular scissors [21], vitrectome [8], bended needles etc. Another option is to keep the patient at the operating room (OR) or in its vicinity and then remove part of the air/gas 60–90 min after the surgery, on the OR bed [22].
There are several potential difficulties with the aforementioned techniques. A prophylactic preoperative PI must either be performed by the referring ophthalmologist or this may necessitate an additional visit prior to surgery outside of the OR. Second, in the current study, a leading indication for DMEK was pseudophakic bullous keratopathy, in which the cornea is severely decompensated rendering Nd:YAG PI very challenging if at all possible. Third, performing an intraoperative PI is not without risks such as bleeding, as was recently showed by Crews et al. to occur in >40% during intraoperative PI creation [23]. Fourth, inadvertent excessively large PIs (Fig. 2) may lead to glare/diplopia/photophobia, lens capsule compromise or even vitreal strands that might stray through the PI. Last, maintaining the postoperative patient on the OR bed for more than an hour and only then reducing the bubble size is not an efficient use of the operating room. With the hereby proposed technique, there is no “bubble time” on the OR bed as the patient is routinely assessed postoperatively at the slit lamp and the gas bubble size is reduced at the slit lamp by the same experienced surgeon. Therefore, the surgery ends as soon as the graft is lifted to the stroma of the host and the AC is completely filled with gas. The results of the PI-less DMEK technique described in this study are similar to those in which a PI is performed. There were no cases of pupillary block after surgery, and the detachment rate and primary failure rate was similar to previous publications [9, 24, 25].
Inadvertent large inferior PIs—performed intraoperatively by scissors. a Cornea is edematous due to primary failure of the graft. Bleeding from this large PI was noted during surgery and may have contributed to the poor outcome in this case. b The cornea is clear following DMEK. Fortunately, despite the large inferior PI, in this case the patient denied having glare/diplopia/photophobia
It is worth mentioning that office gas evacuation should be done with caution by an experienced DMEK surgeon as premature evacuation of too much gas can occur increasing chances of graft detachment [26].
This study had several limitations, first of which was its retrospective nature. A second major limitation of this study is that endothelial cell density (ECD) data following surgery was incomplete (available for only 12 patients), occasionally was performed by automated ECD counter (that is considered less accurate than manually counting) [27], and was not performed according to a predetermined timely schedule. Third was the lack of a PI control group which would have introduced a bias as the surgeon only performed PI while in the midst of the DMEK learning curve and has not performed DMEK with a PI in the past 2 years. As such a comparison between cases with and without PI would not account for the difference in the surgeon’s experience at the time of surgery. Fourth, a high proportion of patients underwent DMEK (over 50%) for pseudophakic bullous keratopathy while a smaller proportion underwent DMEK for Fuchs’ endothelial dystrophy. Finally, the findings of this study only apply to the types of cases that were included, as such, its results do not apply to patients with prior penetrating keratoplasty, prior glaucoma surgery, combined cataract extraction-DMEK or phakic DMEK.
In summary, this study demonstrates that in DMEK surgeries of pseudophakic cases, it is possible to avoid performing PI before or during surgery, with satisfactory results. Partial evacuation of the air/gas from the AC an hour to 1.5 h following surgery is necessary and can be performed safely and easily at the slit lamp and should be combined with postoperative mydriatics.
Summary
What was known before:
-
Descemet’s membrane endothelial keratoplasty (DMEK) has revolutionized the standard of care for endothelial corneal disease.
-
Regardless of the specific type of the tamponading gas, DMEK may lead to a dreaded complication in the form of pupillary block ocular hypertension.
-
Standard DMEK techniques involve performing a prophylactic peripheral iridotomy (PI) either before or during the DMEK procedure.
What this study adds:
-
Novel, safe and simple technique for pseudophakic “PI-less DMEK” described.
-
Peripheral iridectomy can be avoided during DMEK surgery.
-
Partial evacuation of the air or gas from the anterior chamber 1–2 h following surgery combined with postoperative mydriatics is necessary with this technique
References
Ple-Plakon Pa, Shtein RM. Trends in corneal transplantation: indications and techniques. Curr Opin Ophthalmol. 2014;25:300–5. http://www.ncbi.nlm.nih.gov/pubmed/24865170.
Hamzaoglu EC, Straiko MD, Mayko ZM, Sáles CS, Terry MA. The first 100 eyes of standardized Descemet stripping automated endothelial keratoplasty versus standardized Descemet membrane endothelial keratoplasty at one institution. Ophthalmology. 2015;122: 2193–9.
Droutsas K, Lazaridis A, Papaconstantinou D, Brouzas D, Moschos MM, Schulze S, et al. Visual outcomes after descemet membrane endothelial keratoplasty versus Descemet stripping automated endothelial keratoplasty-comparison of specific matched pairs. Cornea. 2016;35:765–71.
Guerra FP, Anshu A, Price MO, Price FW. Endothelial keratoplasty: fellow eyes comparison of Descemet stripping automated endothelial keratoplasty and Descemet membrane endothelial keratoplasty. Cornea. 2011;30:1382–6.
Guerra FP, Anshu A, Price MO, Giebel AW, Price FW. Descemet’s membrane endothelial keratoplasty: prospective study of 1-year visual outcomes, graft survival, and endothelial cell loss. Ophthalmology. 2011;118:2368–73.
Price MO, Giebel AW, Fairchild KM, Price FW. Descemet’s membrane endothelial keratoplasty. Prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology. 2009;116:2361–8.
Melles GRJ, Ong TS, Ververs B, van der Wees J. Preliminary clinical results of Descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2008;145:222–7.
Terry MA, Straiko MD, Veldman PB, Talajic JC, VanZyl C, Sales CS, et al. Standardized DMEK technique: reducing complications using prestripped tissue, novel glass injector, and sulfur hexafluoride (SF6) gas. Cornea. 2015;34:845–52.
Schaub F, Enders P, Snijders K, Schrittenlocher S, Siebelmann S, Heindl LM, et al. One-year outcome after Descemet membrane endothelial keratoplasty (DMEK) comparing sulfur hexafluoride (SF6) 20% versus 100% air for anterior chamber tamponade. Br J Ophthalmol. 2017;101:902–8.
Guell JL, Morral M, Gris O, Elies D, Manero F. Comparison of sulfur hexafluoride 20% versus air tamponade in Descemet membrane endothelial keratoplasty. Ophthalmology. 2015;122:1757–64.
Gonzalez A, Price FW, Price MO, Feng MT. Prevention and management of pupil block after Descemet membrane endothelial keratoplasty. Cornea. 2016;35:1391–5.
Terry MA, Straiko MD, Veldman PB, Talajic JC, VanZyl C, Sales CS, et al. Standardized DMEK technique. Cornea. 2015;34:845–52.
Arnalich-Montiel F, Pérez-Sarriegui A, Lauzirika G, Porrua L, Hernández-Verdejo JL. Pupillary abnormalities in Descemet membrane endothelial keratoplasty after nearly full tamponade. Cornea. 2017;36:290–4. https://www.ncbi.nlm.nih.gov/pubmed/28129299.
Groeneveld-Van Beek EA, Lie JT, Van Der Wees J, Bruinsma M, Melles GRJ. Standardized ‘no-touch’ donor tissue preparation for DALK and DMEK: Harvesting undamaged anterior and posterior transplants from the same donor cornea. Acta Ophthalmol. 2013;91:145–50.
Gabbay IE, Bahar I, Nahum Y, Livny E. Comparison of Descemet stripping under continuous air flow, manual air injection and balanced salt solution for DMEK: a pilot study. Graefe’s Arch Clin Exp Ophthalmol. 2017;255:1605–11.
Dapena I, Moutsouris K, Droutsas K, Ham L, van Dijk K, Melles GRJ. Standardized "no-touch" technique for Descemet membrane endothelial keratoplasty. Arch Ophthalmol. 2011;129:88–94.
Liarakos VS, Dapena I, Ham L, van Dijk K, Melles GRJ. Intraocular graft unfolding techniques in Descemet membrane endothelial keratoplasty. JAMA Ophthalmol. 2013;131:29.
Busin M, Leon P, Scorcia V, Ponzin D. Contact lens-assisted pull-through technique for delivery of tri-folded (endothelium in) DMEK grafts minimizes surgical time and cell loss. Ophthalmology. 2016;123:476–83.
Ćirković A, Beck C, Weller JM, Kruse FE, Tourtas T. Anterior chamber air bubble to achieve graft attachment after DMEK. Cornea. 2016;35:482–5.
Phillips PM, Phillips LJ, Muthappan V, Maloney CM, Carver CN. Experienced DSAEK surgeonʼs transition to DMEK. Cornea. 2017;36:275–9.
Deng SX, Sanchez PJ, Chen L. Clinical outcomes of Descemet membrane endothelial keratoplasty using eye bank–prepared tissues. Am J Ophthalmol. 2015;159:590–6.
Baydoun L, van Dijk K, Dapena I, Musa FU, Liarakos VS, Ham L, et al. Repeat Descemet membrane endothelial keratoplasty after complicated primary Descemet membrane endothelial keratoplasty. Ophthalmology. 2015;122:8–16.
Crews JW, Price MO, Lautert J, Feng MT, Price FW. Intraoperative hyphema in Descemet membrane endothelial keratoplasty alone or combined with phacoemulsification. J Cataract Refract Surg. 2018;44:198–201.
Rodríguez-Calvo-De-Mora M, Quilendrino R, Ham L, Liarakos VS, Van Dijk K, Baydoun L, et al. Clinical outcome of 500 consecutive cases undergoing Descemet’s membrane endothelial keratoplasty. Ophthalmology. 2015;122:464–70.
Gorovoy MS. DMEK complications. Cornea. 2014;33:101–4.
Leon P, Parekh M, Nahum Y, Mimouni M, Giannaccare G, Sapigni L, et al. Factors associated with early graft detachment in primary Descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2018;187:117–24.
Price MO, Fairchild KM, Price FW. Comparison of manual and automated endothelial cell density analysis in normal eyes and DSEK eyes. Cornea. 2013;32:567–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Livny, E., Bahar, I., Levy, I. et al. “PI-less DMEK”: results of Descemet’s membrane endothelial keratoplasty (DMEK) without a peripheral iridotomy. Eye 33, 653–658 (2019). https://doi.org/10.1038/s41433-018-0294-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-018-0294-x