Abstract
Background/Objectives
To assess the risk of immediate sudden visual loss (“wipe-out” phenomenon) following non-penetrating deep sclerectomy (NPDS) for end-stages glaucoma within the first 6-months postoperative period.
Subjects/Methods
Monocenter database study. We reviewed the results for 73 eyes with severe or end-stage glaucoma that underwent NPDS. End-stage glaucoma (stage 5) was defined by the inability of patients to perform the Humphrey visual field test or by a visual acuity <20/200 due to glaucoma, according to the Glaucoma Staging System classification. Severe glaucoma (stage 4) was defined by a mean deviation (MD) <−20 dB by the preoperative 24-2 Humphrey visual field assessment. All eyes had a severe defect on the central 10° visual field: only a central island of vision remained. “Wipe-out” was defined as the permanent postoperative reduction of visual acuity to <20/200 or to “counting fingers” or less if preoperative visual acuity was <20/200.
Results
The mean age was 60 years (range 22–86). Before surgery, the average MD (Humphrey 24-2) was −25.6 ± 3.8 dB, the MD (Humphrey 10-2) −19.9 ± 7.0 dB, and the VFI 24.6 ± 13%. There were no cases of postoperative flat anterior chamber. No patients experienced “wipe-out” within the first 6 months following surgery. At the six-month visit, intraocular pressure (IOP) had decreased significantly from 22.0 ± 8.8 to 13.5 ± 4.5 mmHg (P<0.001). There were no significant changes in mean visual acuity after 6 months (P = 6).
Conclusions
In our study, NPDS provided considerable IOP decrease with no occurrences of “wipe-out” and few other complications. Consideration of NPDS in end-stage and severe glaucoma is advisable given its low risk of intraoperative and postoperative complications and the low risk of wipe out. This surgery should probably be offered with less apprehension about the risk of “wipe-out” in end-stages glaucoma.
Similar content being viewed by others
Introduction
Low IOP and decrease of IOP diurnal fluctuations have been shown to be associated with reduced progression of visual field defects [1,2,3], especially in patients with advanced glaucoma [4]. Glaucoma filtration surgery is the major step when maximal medical and laser therapy were not efficient enough to lower the IOP and stabilize glaucoma progression. Furthermore, in cases of severe and end-stage glaucoma, significant lowering IOP is mandatory and frequently requires filtering surgery in order to achieve the target IOP. The decision to proceed with filtering surgery for glaucomatous patients with a very constricted visual field is difficult to make. Indeed, there is a potential risk of immediate sudden visual loss (“wipe-out” phenomenon). “Wipe-out” is an irreversible immediate unexplained sudden loss of vision (which includes central visual acuity) after filtering surgery, especially in glaucoma patients with severe visual field loss. It could occurs after any surgical filtering procedure and frightens surgeons, who sometimes prefer not to proceed with this kind of surgery [5]. The occurrence of this phenomenon after trabeculectomy is controversial, frequency varies from 0 to 13.6%. There are conflicting studies that report a true risk of “wipe-out” for trabeculectomy [6, 7], whereas others report none [8, 9]. Also, studies that show the highest rates of “wipe-out”, up to 13.6% after trabeculectomy, are quite old studies. Surgery techniques have evolved with higher security level, questioning the current frequency of this frightening complication. We are entitled to question the frequency of this phenomenon.
A very limited number of studies have explored the potential risk of “wipe-out” following non-penetrating deep sclerectomy (NPDS) in advanced glaucoma [10, 11], and to our knowledge, none in case of severe or end-stage glaucoma.
The aim of our study was to assess the risk of immediate sudden visual loss following NPDS in severe and end-stage glaucoma patients. According to previous reports, this population had a high theoretical risk of “wipe-out” [8, 12,13,14]. This risk assessment is important to keep in mind when a practitioner has to consider a surgical option for a patient with end-stage glaucoma, but this risk should not be over-estimated based on non-unequivocal results.
Methods
Data concerning 351 consecutive eyes of 254 patients who underwent NPDS with mitomycin-C, between 2009 and 2015, were retrospectively reviewed (Hôpital des XV-XX, Paris, France). We selected only eyes with preoperative severe or end-stage glaucoma which was our major inclusion criteria.
End-stage glaucoma (stage 5) was defined by the inability of patients to perform the 24-2 Humphrey visual field test as a result of severe loss of field or by a visual acuity <20/200 due to glaucoma, according to the Glaucoma Staging System (Bascom Palmer) [15]. Severe glaucoma (stage 4) was defined by a mean deviation (MD) <−20 dB by the preoperative 24-2 Humphrey visual field assessment, with at least two points with sensitivity of 0 dB within the central 5° (Fig. 1) [15].
All the eyes had a constricted visual field <0° (severe defect on the Humphrey 10-2 visual field assessment and most of the 24-2 visual field points had no sensitivity at all (0 dB) or <5 dB. Only a central island of vision remained. The need for surgery was made by the treating physician on the basis of progressing damage to several visual fields despite maximal tolerate antiglaucomatous therapy (beta-blockers, prostaglandins, 2-alpha agonists, and carbonic anhydrase inhibitors). “Wipe-out” was defined as the permanent postoperative reduction of visual acuity to <20/200, to “counting fingers” or less if preoperative visual acuity was <20/200 [16].
Preoperative examinations consisted in corrected visual acuity, Goldmann applanation tonometry, central cornea thickness and slit-lamp examination, including vertical cup/disk ratio and gonioscopy, showing an open angle. These elements were recorded during the last visit before surgery. All visual field measurements were performed using the threshold automated perimetry SITA-standard with stimulus III-White in 24-2 and 10-2 programs of the Humphrey Field Analyzer; Carl Zeiss Meditec®).
Surgical method
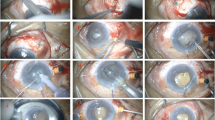
The procedure consisted of NPDS alone or combined with phacoemulsification. All procedures have been done by the same team (four experienced surgeons). The steps of the NPDS procedure were the following: topical anesthesia with oxybuprocaine eye drops and xylocaine gel, limbus-based conjunctival flap, scleral light cautery applied as needed, application of a sponge soaked in 0.2 mg/ml mitomycin below the conjunctival flap (1–2 min), 1/3 scleral thickness superficial rectangular flap, deep scleral rectangular flap, peeling off of the floor of Schlemm’s canal and external trabeculum (if NPDS was alone, a paracentesis was performed just before the peeling), collagen implant if necessary depending on the local risk of postoperative flap fibrosis (Aquaflow, Staar®)—placed radially below the scleral thickness superficial flap, secured with nylon 10/0 sutures—conjunctival sutures with resorbable vicryl® 8/0. The phacoemulsification procedure was according to the “divide-and-conquer” technique with monofocal intraocular lens implantation. Postoperatively, all patients received topical steroid (dexamethasone 0.1%; one drop three times per day) for 3 months following the procedure.
All patients were examined 1 day, 8 days, 1 month, 3 and 6 months after the procedure. The incidence of postoperative complications, such as flat or shallow anterior chamber, choroidal detachment and bleb leak, was recorded at each visit. The main outcome measures of our study were: occurrence of “wipe-out”, best corrected visual acuity, IOP, and number of antiglaucomatous medicines needed. Data from the 6-month visit was used for statistical analysis. This study was conducted in accordance with the tenets of the Helsinki Declaration.
The paired-t-test was used to compare IOP and logMAR visual acuity and the Student t test for outcomes, with or without collagen implant. Statistical significance was defined as P<0.05.
Results
Seventy-three eyes of 59 patients fulfilled the inclusion criteria and their data were reviewed in this study. Demographic and baseline clinical characteristics of our study population are summarized in Table 1. Ten eyes out of 73 were stage 5 or end-stage glaucoma and 63 eyes of 73 were stage 4 or severe glaucoma, according to the Glaucoma Staging System (Bascom Palmer) classification [15].
Sixty-two eyes had primary open-angle glaucoma, four juvenile glaucoma, and seven secondary open-angle glaucoma. The mean age was 60 years ranging from 22 to 86. The mean preoperative IOP was 22 ± 9 mmHg with maximal medical therapy (range 11–50). Preoperative visual acuity ranged between “light perception” and 20/20 (mean 0.34 ± 0.50 logMAR) and six (8%) eyes had visual acuity of 20/400 or worse. Regarding preoperative visual fields, the average MD (Humphrey 24-2) was −25.6 ± 3.8 dB, the visual function index (VFI) was 24.6 ± 13% and the MD (Humphrey 10-2) −19.9 ± 7.0 dB.
NPDS alone was performed on 55 (75%) eyes, whereas 18 (25%) underwent NPDS combined with phacoemulsification and intraocular lens implantation. For the NPDS procedure, 33 (45%) eyes received a collagen implant (Aquaflow, Staar®), whereas 40 (55%) did not. Four eyes had previously undergone trabeculectomy, which was not functional at the time of the NPDS. Six patients were blind in the fellow eye, of which five were due to uncontrolled glaucoma and one due to retinal detachment.
There were no intraoperative complications, except seven micro-perforations of the trabeculo-descemet membrane which did not required iridectomy (no trabeculectomy conversion). When a micro-perforation occurred, IOP was significantly lower at day-1 (4.8 ± 1.0 versus 7.4 ± 2.9 mmHg, P<0.001; IC95 [1.15; 4.06]; Student-t-test), but not at day-8 and month-6. The prognosis was no worse in term of visual acuity and post-operatives complications, such as shallow anterior chamber, choroidal detachment, bleb leak and iris incarceration.
Immediate postoperative complications were (within the first 8 days):
Two cases of iris incarcerations: one treated by laser iridoplasty (intraoperative micro-perforation) and the other by surgery.
Two localized choroidal detachments.
One hypertonia at 35 mmHg, that went down to 10 mmHg after goniopuncture (YAG laser procedure performed on the trabeculo-descemet window in order to increase the filtration).
One inflammatory bleb requiring early needling.
Four bleb leaks (Seidel) that required sutures, including one with shallow anterior chamber.
There were no cases of postoperative flat anterior chamber.
After 6 months, three eyes underwent needling with injection of 5-Fluorouracil (5-FU), 19 (26%) have needed goniopuncture and 4 (5%) eyes had iris incarceration (three spontaneous and one posttraumatic) without consequences on IOP. Regarding goniopuncture, 13 (68%) did not have any complications, four (21%) had iris incarceration that needed peripheral iridectomy, 2 (11%) had incarcerations with successful laser iridoplasty.
There were no cases of “wipe-out” within the 6-month postoperative follow-up period and there were no significant changes in visual acuity (from 0.34 ± 0.5 to 0.31 ± 0.49 logMAR, P = 0.6; paired-t-test).
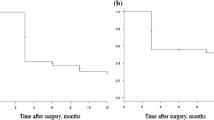
At the 6-month visit, IOP had decreased significantly from 22.0 ± 8.8 mmHg before surgery to 13.5 ± 4.5 mmHg (P < 0.001; IC95 [6.20; 10.67]; paired-t-test) (decrease of 39%). Fifty-six (77%) eyes had an IOP <16 mmHg and 69 (95%) an IOP <21 mmHg (Fig. 2). Forty-seven patients (64%) had got an IOP decrease more than 20% from the baseline. The postoperative number of IOP-lowering eye drops decreased from 3.0 ± 0.8 to 0.02 ± 0.16 (P < 0.001; IC95 [2.7; 3.1]; paired-t-test).
There were no statistically significant differences in IOP for patients who were treated by NPDS with or without collagen implant (13.8 mmHg versus 13.3 mmHg, P = 0.6; Student t test) (Table 2). No significant changes in visual acuity was observed in the group with collagen implant (from 0.33 ± 0.48 to 0.27 ± 0.49 logMAR, P = 0.4; paired-t-test) and in the group without collagen implant (from 0.36 + ± 0.57 to 0.35 ± 0.49 logMAR, P = 0.7; paired-t-test).
At month-6, visual acuity was significantly better when the NPDS was combined with phacoemulsification (from 0.36 ± 0.30 to 0.14 ± 0.17 logMAR; P = 0.001; IC95 [0.05; 0.39]; paired-t-test). There was no significant changes in visual acuity at month-6 when NDPS was proceed alone (from 0.34 ± 0.59 to 0.37 ± 0.54 logMAR, P = 0.4; paired-t-test). IOP was significantly higher at day-1 and day-8 when it was a combined procedure and was not significant at month-6 (Student t test) (Table 3).
Discussion
It is known that a decrease in IOP reduce the rate of visual field progression in glaucomatous disease [1,2,3,4, 17]. The AGIS study showed that the lower the IOP, the slower the degradation of the visual field, in advanced glaucoma patients [4]. Everyone acknowledges the importance to achieve low target IOP, but the decision is especially difficult to make in these patients, because of the potential risk of “wipe-out”. This phenomenon is an irreversible and immediate sudden reduction of visual acuity with no apparent causes after filtering surgery (especially in glaucoma with advanced visual field loss). The mechanism of “wipe-out” is not clear but it appears to be associated with ocular hypotony during filtering surgery [9, 18, 19]. This risk appears to increase with the rapidity of onset and the duration of the intraoperative hypotony. It may cause optic nerve hemorrhage and disorders in perfusion pressure (disrupting the balance between IOP and blood pressure). A flat anterior chamber in the first postoperative week [20] and choroidal effusion [14, 21] are also a significant risk factor for severe visual loss. Older age and coronary artery disease seems to also be a risk factor [13, 22]. Also, it has been suggested that it can happen due to postoperative hypertonia resulting in macular ischemia [23].
Trabeculectomy in severe or end-stage glaucoma has been well studied and the results have split the authors into two camps. Some fear the danger of performing this surgical procedure in this population and warn about it, whereas others suggest that the risk is minimal or non-existent. Kolker et al. [6] reported three cases (13.6%) of sudden visual loss after trabeculectomy (preoperative visual fields defects extending to within 5° of fixation) and Aggarwal et al. [12] (preoperative visual fields confined to a central island around 10°) reported one (11%), with two other cases having identifiable causes. In a later study, Costa et al. [13] stated that “wipe-out” was a risk, but relatively rare (4/508 eyes, 0.8%), as Langerhorst et al. (1/50 eyes, 2%) [24] and Fujishiro et al. (2/27 eyes, 7%) [25]. Levene et al. [26] and Law et al. [16] (mean preoperative MD −25.2 ± 5.1 dB) also reported several cases of central vision loss, but there were clearly identifiable causes, such as macular edema, hypotony, hypertony, and uveitis. More recently, Topouzis et al. (mean preoperative MD −27.9 ± 2.7 dB) [8] reported no cases of “wipe-out” in prospective studies with end-stage glaucoma and Balekudaru et al. [22] concluded that visual loss after surgery in advanced glaucoma is rare and most often because of reversible causes. Several other studies have also reported no cases of “wipe-out” in treating patients with advanced glaucoma [9, 18, 19, 22, 23, 27,28,29]. Some authors even question its real existence [9, 30, 31]: “There is an old adage that if the operation is done when there is a small remaining central island of field, with or without some peripheral field, the patient will lose the rest of his central vision, but we have not found this to be true” [31].
This discrepancy in the incidence of “wipe-out” is probably related to confusion concerning its definition and technological advances in surgery. Many studies recorded macular edema, cataract, and other causes as sudden visual loss. Moreover, studies reporting a high rate of “wipe-out” are old studies and were performed more than 25 years ago. The technology several years ago was probably insufficient to accurately detect the causes of visual loss (OCT and macular edema for example) and some visual loss were probably wrongly labeled “wipe-out”. As a reminder, “wipe-out” phenomenon is a diagnosis of elimination. Furthermore, the surgical techniques were less highly developed than nowadays. We are using increasingly smaller instruments, which was not used for studies reporting the highest rates of “wipe-out” several years ago. For example, we can mention the Khaw Small Membrane Punch, developed in the “trabeculectomy – Moorfields safer surgery system” [32, 33].
In 2005, Moster and Moster wrote that: “With meticulous efforts to avoid known postoperative complications, we will be able to relegate “wipe-out” to its proper place in history and not to a complication of modern glaucoma filtering surgery” [30].
A small number of studies have explored the risk of “wipe-out” following NDPS in advanced glaucoma, but none in terminal cases (severe and end-stage). In NPDS, by removing the inner wall of Schlemm’s canal and the trabecular meshwork with the conservation of the trabeculo-Descemet’s membrane, the aqueous outflow is increased but controlled towards the filtration site [34]. Indeed, the non-penetration of the anterior chamber in NPDS results in a progressive and controlled decrease of IOP. There is no massive hypotony and flat anterior chamber during the procedure, in contrast to trabeculectomy. NPDS appears to have superior safety profile [34] and may theoretically reduce the risk of “wipe-out”. The relief of IOP appears to be comparable to that achieved with trabeculectomy, but with a lower rate of early postoperative complications [35], and offer potential gains for patients in terms of quality of life [36].
Ates et al. in a prospective study of 54 eyes with advanced field loss (visual fields with MD<−12 dB) and Gierek-Lapinska et al. (35 eyes with advanced glaucoma, mean preoperative MD −17 ± 5.2 dB) reported no cases of sudden visual loss after deep sclerectomy [10, 11]. Ates concluded that NDPS “could be a valuable alternative to trabeculectomy especially in cases of advanced medically uncontrolled open angle glaucoma” [10].
Our study investigated the risk of immediate sudden visual loss following deep sclerectomy for severe and end-stage glaucoma. This population had a high risk of “wipe-out” (small visual field <10°), according to previous reports [8, 12,13,14]. We observed the same rate of IOP control and complications in our sclerectomy study as in others [10, 11, 37,38,39,40]. It provided considerable IOP decrease with a great security, as there are no occurrences of “wipe-out” and few other complications.
One of the short comings of our report was the relatively small sample size. Some of the reports regarding the risk of wipe-out after trabeculectomy was <1% and our sample size of severe or end-stage glaucoma patients was only 73 eyes. If the risk is in the range of 1%, it may not have been detected.
We followed our patients longer (mean of 22 months) but we resumed our data in the 6 months following the surgery voluntarily because we were looking for an early sudden visual loss (“wipe-out”) and we felt that delay was enough regarding other studies [8]. We were also interested in changes in the central 10° visual field after NPDS, that seems to provide stability, but it was not the focus of our study. As a reminder, assessing visual acuity becomes as important as visual field data to estimate the evolution of glaucomatous disease at terminal stages [41].
To finish, our findings are limited by the retrospective design of our study. The need for surgery was made by the treating physician on the basis of progressing damage to several visual fields despite maximal medical treatment.
We found no significant changes in IOP and visual acuity for patients who were treated by NPDS with or without collagen implant. On the other side, IOP was significantly higher at day-1 and day-8 when NPDS was combined with phacoemulsification and was not significant at month-6. It is a well-known result due to a higher inflammation and residual viscoelastic in the anterior chamber in early postoperative combined procedure period. Obviously, visual acuity was significantly better when the NPDS was combined with phacoemulsification.
Otherwise, we can notice the relative young age of our sample (60 years old). This reminds us that it is a severe pathology that often concerns patients with a very long life expectancy and there will be further loss of vision from glaucoma, unless the IOP is lower than the level at which the damage occurred.
Regarding the paradigm of glaucoma therapy, cyclodestructive procedures appears to be the last resort in eyes with multiples failed filtering surgery and in painful eyes which have no visual potential [42]. Micro invasive glaucoma surgery (MIGS) could be an option also, but usually target pressure obtained are higher in these techniques. It is an emerging treatment option that can decrease dependency on medication. These new procedures are bleb-independent and hence have a better safety profile (especially the risk for generating hypotony) [43, 44] but it seems to offer a modest IOP reduction [45, 46]. Therefore, it is currently performed and approved by the FDA in open angle glaucoma patients with early to moderate disease [44, 46]. These techniques have not yet been validated for end-stages glaucoma.
In conclusion, consideration of NPDS in end-stage and severe glaucoma is advisable given its security and efficiency: controlled reduction of IOP during the surgery, low risk of intraoperative flat chamber, of postoperative complications and low risk of wipe out with a significant IOP lowering.
Regarding our results, this surgery should probably be offered with less apprehension about the risk of “wipe-out” in end-stages glaucoma, our efforts be concentrated to avoid the occurrence of a sudden hypotonia. Obviously, the management of theses end-stages glaucoma must take into account the patient’s age and co-morbidities: the life expectancy. A risk-benefit analysis on a case-to-case basis is needed.
What was known before
There are conflicting studies that report a true risk of “wipe-out” in filtering surgery for advanced glaucoma
What this study adds
Assess the risk of immediate sudden visual loss (“wipe-out” phenomenon) following non-penetrating deep sclerectomy (NPDS) for end-stages glaucoma within the first 6-months postoperative period.
References
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol Chic Ill 1960. 2002;120:1268–79.
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–97.
Lichter PR, Musch DC, Gillespie BW, Guire KE, Janz NK, Wren PA, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108:1943–53.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429–40.
Marques A. Managing advanced unilateral pseudoexfoliative glaucoma. BMJ Case Rep. 2014. https://doi.org/10.1136/bcr-2014-204011.
Kolker AE. Visual prognosis in advanced glaucoma: a comparison of medical and surgical therapy for retention of vision in 101 eyes with advanced glaucoma. Trans Am Ophthalmol Soc. 1977;75:539–55.
Otto J. Loss of point of fixation after glaucoma surgery. Klin Mon Augenheilkd Augenarzt Fortbild. 1957;131:178–95.
Topouzis F, Tranos P, Koskosas A, Pappas T, Anastasopoulos E, Dimitrakos S, et al. Risk of sudden visual loss following filtration surgery in end-stage glaucoma. Am J Ophthalmol. 2005;140:661.e1–e7.
Lichter PR, Ravin JG. Risks of sudden visual loss after glaucoma surgery. Am J Ophthalmol. 1974;78:1009–13.
Ates H, Andac K, Uretmen O. Non-penetrating deep sclerectomy and collagen implant surgery in glaucoma patients with advanced field loss. Int Ophthalmol. 1999;23:123–8.
Gierek-Lapińska A, Leszczyński R, Wróbel A. Non-penetrating deep sclerectomy in the treatment of advanced cases of open angle glaucoma]. Klin Ocz. 2004;106(1-2 Suppl):168–9.
Aggarwal SP, Hendeles S. Risk of sudden visual loss following trabeculectomy in advanced primary open-angle glaucoma. Br J Ophthalmol. 1986;70:97–9.
Costa VP, Smith M, Spaeth GL, Gandham S, Markovitz B. Loss of visual acuity after trabeculectomy. Ophthalmology. 1993;100:599–612.
Francis BA, Hong B, Winarko J, Kawji S, Dustin L, Chopra V. Vision loss and recovery after trabeculectomy: risk and associated risk factors. Arch Ophthalmol Chic Ill 1960. 2011;129:1011–7.
Mills RP, Budenz DL, Lee PP, Noecker RJ, Walt JG, Siegartel LR, et al. Categorizing the stage of glaucoma from pre-diagnosis to end-stage disease. Am J Ophthalmol. 2006;141:24–30.
Law SK, Nguyen AM, Coleman AL, Caprioli J. Severe loss of central vision in patients with advanced glaucoma undergoing trabeculectomy. Arch Ophthalmol. 2007;125:1044–50.
Aptel F, Bron AM, Lachkar Y, Schweitzer C. Change in visual field progression following treatment escalation in primary open-angle glaucoma. J Glaucoma. 2017;26:875–80.
Martinez JA, Brown RH, Lynch MG, Caplan MB. Risk of postoperative visual loss in advanced glaucoma. Am J Ophthalmol. 1993;115:332–7.
O’Connell EJ, Karseras AG. Intraocular surgery in advanced glaucoma. Br J Ophthalmol. 1976;60:124–31.
De Smedt SK, Fonteyne YS, Muragijimana F, Palmer K, Murdoch I. Glaucoma surgery outcome in Rwanda. J Glaucoma. 2016;25:698–703.
Gedde SJ, Herndon LW, Brandt JD, Budenz DL, Feuer WJ, Schiffman JC. Surgical complications in the Tube Versus Trabeculectomy Study during the first year of follow-up. Am J Ophthalmol. 2007;143:23–31.
Balekudaru S, George R, Panday M, Singh M, Neog A, Lingam V. Prospective evaluation of early visual loss following glaucoma-filtering surgery in eyes with split fixation. J Glaucoma. 2014;23:211–8.
Chockalingam M. Visual outcome and risk of sudden visual loss following trabeculectomy in end-stage glaucoma. Kerala J Ophthalmol. 2010;22:346–9.
Langerhorst CT, de Clercq B, van den Berg TJ.Visual field behavior after intra-ocular surgery in glaucoma patients with advanced defects Doc Ophthalmol Adv Ophthalmol. 1990;75:281–9.
Fujishiro T, Mayama C, Aihara M, Tomidokoro A, Araie M. Central 10-degree visual field change following trabeculectomy in advanced open-angle glaucoma. Eye. 2011;25:866–71.
Levene RZ. Central visual field, visual acuity, and sudden visual loss after glaucoma surgery. Ophthalmic Surg. 1992;23:388–94.
Grunewald F, Bresson-Dumont H, Bechetoille A. La trabéculectomie est-elle sans danger en cas de menace sur le point de fixation? J Fr Ophtalmol. 1996;19:253–8.
Baser EF, Seymenoglu G, Mayali H. Trabeculectomy for advanced glaucoma. Int Ophthalmol. 2011;31:439–46.
Popovic V, Sjöstrand J. Long-term outcome following trabeculectomy: II. Acta Ophthalmol (Copenh). 1991;69:305–9.
Moster MR, Moster ML. Wipe-out: a complication of glaucoma surgery or just a blast from the past? Am J Ophthalmol. 2005;140:705–6.
Chandler PA, Grant WM. Lectures on glaucoma. 431 p. Philadelphia: Lea and Febiger; 1965. p.136.
Dhingra S, Khaw PT. The moorfields safer surgery system. Middle East Afr J Ophthalmol. 2009;16:112–5.
Khaw PT, Chiang M, Shah P, Sii F, Lockwood A, Khalili A. Enhanced trabeculectomy: the moorfields safer surgery system. Dev Ophthalmol. 2017;59:15–35.
Sarodia U, Shaarawy T, Barton K. Nonpenetrating glaucoma surgery: a critical evaluation. Curr Opin Ophthalmol. 2007;18:152–8.
Ambresin A, Shaarawy T, Mermoud A. Deep sclerectomy with collagen implant in one eye compared with trabeculectomy in the other eye of the same patient. J Glaucoma. 2002;11:214–20.
Eldaly MA, Bunce C, Elsheikha OZ, Wormald R. Non-penetrating filtration surgery versus trabeculectomy for open-angle glaucoma. Cochrane Database Syst Rev. 2014;CD007059.
Sponsel WE, Groth SL. Mitomycin-augmented non-penetrating deep sclerectomy: preoperative gonioscopy and postoperative perimetric, tonometric and medication trends. Br J Ophthalmol. 2013;97:357–61.
Suominen SMA, Harju MP, Vesti ET. Deep sclerectomy in primary open-angle glaucoma and exfoliative glaucoma. Eur J Ophthalmol. 2016;26:568–74.
Moreno-López M, Pérez-Alvarez MJ. Short- and medium-term intraocular pressure lowering effects of combined phacoemulsification and non-penetrating deep sclerectomy without scleral implant or antifibrotics. Arch Soc Esp Oftalmol. 2006;81:93–100.
Lachkar Y, Neverauskiene J, Jeanteur-Lunel MN, Gracies H, Berkani M, Ecoffet M, et al. Nonpenetrating deep sclerectomy: a 6-year retrospective study. Eur J Ophthalmol. 2004;14:26–36.
Guedes RAP, Guedes VMP. Comment surveiller un glaucome agonique ? J Fr Ophtalmol. 2013;36:442–8.
Sharaawy T, Bhartiya S. Surgical management of glaucoma: evolving paradigms. Indian J Ophthalmol. 2011;59(Suppl 1):S123–30.
Saheb H, Ahmed IIK. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23:96–104.
Pillunat LE, Erb C, Jünemann AG, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;29:1583–1600.
Buffet J, Brasnu E, Baudouin C, Labbé A. Efficacy of 2 trabecular micro-bypass stents during phacoemulsification for mild to advanced primary open-angle glaucoma controlled with topical hypotensive medications. J Glaucoma. 2017;26:1149–54.
Pathak-Ray V. Advances in glaucoma surgery: paradigm shift in management. Oman J Ophthalmol. 2016;9:1–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leleu, I., Penaud, B., Blumen-Ohana, E. et al. Risk assessment of sudden visual loss following non-penetrating deep sclerectomy in severe and end-stage glaucoma. Eye 33, 902–909 (2019). https://doi.org/10.1038/s41433-019-0336-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0336-z
This article is cited by
-
Five-year results of non-penetrating deep sclerectomy with demineralized cancellous bone xenogenically derived collagen glaucoma implant
International Ophthalmology (2021)
-
Long term outcomes of cataract surgery in severe and end stage primary angle closure glaucoma with controlled IOP: a retrospective study
BMC Ophthalmology (2020)