Abstract
Objectives
To illustrate the varying clinical presentations of cutaneous sarcoidosis affecting the periocular region, which may masquerade as other clinical entities such as basal cell carcinoma or seborrheic dermatitis. Furthermore, the authors present an unusual observation of lupus pernio involving the adnexal region with the rare presence of perineural granulomas on histology following incisional biopsy.
Methods
We report a consecutive series of four cases with lesions involving the eyelids with varying clinical appearances. All four patients presented to our adnexal service undergoing incisional diagnostic biopsy. Histology following biopsy subsequently resulted in further investigation and management of both local cutaneous lesions and systemic sarcoidosis.
Results
Three of our four cases had evidence of pulmonary involvement on chest X-ray. Over an 18-month period, one of two patients responded to intralesional triamcinolone and subsequently to oral methotrexate (15 mg/week). Two patients were observed with their periocular lesions remaining stable without therapy.
Conclusions
All four patients presented to the adnexal service with lesions of varying morphology and were diagnosed with sarcoidosis following incisional biopsy highlighting the vital role of oculoplastic surgeons in diagnosing this multisystem inflammatory disease. We describe our experience of intralesional triamcinolone, oral methotrexate and watchful observation in the management of such lesions.
Similar content being viewed by others
Introduction
Sarcoidosis is a multisystem inflammatory condition of unknown aetiology; histologically characterised by non-caseating granulomas. The incidence is higher in Afro-Caribbeans and Scandinavians and is more common in women than in men. Pulmonary involvement is the most common systemic manifestation. Cutaneous involvement is seen in approximately 20–35% cases and can be the presenting feature of disease [1]. Cutaneous features include maculopapular eruptions, lupus pernio and erythema nodosum.
While uveitis is one of the common ophthalmic manifestations, orbital inflammatory disease with dacryoadenitis is not uncommon [2]. Diagnosis is based on typical clinical features, raised inflammatory markers, elevated serum angiotensin-converting enzyme (ACE), hilar lymphadenopathy on chest radiography and presence of non-caseating granulomas on biopsy of lesions.
Management is largely targeted towards symptom relief and to limit the loss of function. Oral, intralesional and topical corticosteroids are used as first-line agents for rapid response with steroid sparing immunosuppression a therapeutic option. As the disease can remain quiescent, observation is an option for asymptomatic patients.
The authors discuss four consecutive cases of cutaneous sarcoid with a spectrum of clinical features presenting to our Adnexal service. The heterogeneity in clinical appearance of periocular lesions in combination with patients often having no extracutaneous involvement at the time of presentation highlights the vital role of diagnostic biopsy for histological support in diagnosing this multisystem disease.
The study adhered to the principles of the Declaration of Helsinki.
Patient 1
A 57-year-old Afro-Caribbean gentleman was referred by his general practitioner with a 6-week history of painless right upper lid erythematous swelling.
Examination showed a violaceous, spindle shaped, erythematous swelling involving the right upper lid with a dough-like consistency on palpation (Fig. 1a, b). He had 6/5 Snellen visual acuity in both eyes and the remainder of his ophthalmic and orbital examinations were unremarkable. There were no palpable preauricular or submandibular lymph nodes. Serum ACE and vasculitis screen were unremarkable with normal serum biochemistry and haematology.
a, b Lupus pernio: erythematous swelling of the right upper lid. c Haematoxylin and eosin (H&E)-stained section of the skin biopsy. The arrow points to a dermal granuloma. d Higher power view of c showing a well-defined collection of epithelioid histiocytes constituting a non-caseating granuloma (granulomatous inflammation). e, f Right upper lid post intralesional triamcinolone injection. g H&E showing a peripheral nerve around which there is oedema (clefts), surrounded by granulomatous inflammation
A debulking biopsy was carried out following no clinical improvement after a trial of topical hydrocortisone for presumed atopic dermatitis. A spindle-shaped strip of skin (24 × 7 × 4 mm) was excised and the histology showed the presence of non-caseating granulomas with excess mucin deposition (Fig. 1c, d) and perineural granulomas (Fig. 1g).
His upper lid swelling was affecting his field of vision and so was treated with intralesional triamcinolone at a dose of 10 mg/mL. No side effects were noted following treatment with near resolution of the lesion (Fig. 1e, f).
Four months following initial treatment, the right upper lid swelling recurred. In consultation with the dermatologists, he was commenced on oral methotrexate at a dose of 15 mg/week. Six months post initiation of methotrexate, his upper lid erythema and swelling had resolved completely. He remains in remission currently on 10 mg/week with a view to cessation of methotrexate therapy following a reducing regimen.
Patient 2
A 51-year-old Caucasian gentleman was referred by his general practitioner for a 12-month history of painless right upper lid dermatitis unresponsive to topical hydrocortisone.
Examination of his right upper lid showed a raised, localised patch of scaly erythematous dermatitis with no nodular or telangiectatic changes (Fig. 2a). Ophthalmic examination was completely unremarkable with 6/6 Snellen visual acuity in both eyes with no orbital inflammation or lymphadenopathy of the head and neck.
Serum ACE and routine biochemistry and haematology were within normal limits.
He had an incisional biopsy where an ellipse of skin measuring 11 × 6 × 3 mm was excised from his right upper lid demonstrating granulomatous dermatitis with, nodular, non-caseating granulomatous inflammation (Fig. 2b, c). The patient underwent bronchoscopy and was found to have lung nodules, which on biopsy were characteristic of pulmonary sarcoid.
Following biopsy, the patient did not want any further treatment and was discharged from the oculoplastic service and remains under annual review with the respiratory team.
Patient 3
A 47-year-old Caucasian female was referred to our oculoplastic service by her general practitioner for a suspected basal cell carcinoma of her right medial canthus. She had a past medical history of asthma secondary to alpha-1-antitrypsin deficiency for which she was on inhalers only.
On examination, there was a raised, scaly, nodular lesion involving the right medial upper lid margin above the level of the medial canthal ligament associated with yellowish discoloration (Fig. 3a). No evidence of lacrimal gland enlargement or lymphadenopathy was found. She underwent a punch biopsy, which revealed granulomatous dermatitis with many well-defined granulomas that contained giant cells with no evidence of caseation (Fig. 3b–d).
a Right medial canthal nodular thickening with yellowish discoloration. b Low-power view ×20 with surface epithelium on the right-hand side and dermis on left-hand side showing eosinophilic appearances due to granulomas. c ×100 view of surface epithelium appearing normal. d ×200 high-power view of dermal granuloma with histiocytes with eosinophilic cytoplasm and little surrounding inflammation
Further investigations revealed a raised serum ACE level of 110 U/L (ref range 20–70). Chest X-ray showed mediastinal and bilateral hilar lymphadenopathy. The patient underwent contrast enhanced Computed Tomography (CT) studies of her thorax and bronchoscopy studies under the respiratory team, which confirmed sarcoidosis.
On follow-up, the right medial canthal nodule was inflamed and so intralesional triamcinolone was administered at a dose of 4 mg. Six months later, the patient reported little benefit from treatment and declined further therapy. One year following initial presentation, the lesion was unchanged and she remains under annual review in our adnexal service.
Patient 4
A 56-year-old Caucasian male was referred to our oculoplastic service with a history of bilateral swelling of the medial aspect of both upper lids. He was otherwise fit and well with no past medical history.
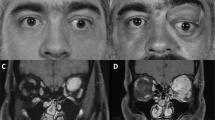
Clinical examination found erythema and firm swelling with thickening of the skin of the medial aspect of the right and left upper lids, with left lower lid involvement also (Fig. 4a, b). There was no evidence of lymphadenopathy or lacrimal gland enlargement. Visual acuity was 6/4 OD and 6/5 OS and the remainder of his ophthalmic examination was unremarkable.
a, b Bilateral swelling and erythema of upper lids medially and left lower lid. c Haematoxylin and eosin (H&E) showing skin peppered with numerous dermal granulomas, an example of which is indicated by the black arrow. d Higher power view of Fig. 4c showing two non-caseating well-defined granulomas, the right one of which contains giant cells
Serum ACE, biochemistry and haematology studies were all within normal limits, however, a vasculitic screen demonstrated a raised serum Antineutrophil Cytoplasmic Antibodies (ANCA) level. Three incisional biopsies of approximately 5 mm each were taken from both medial canthal lesions and the left lower lid lesion. Histology showed numerous well-defined, non-caseating granulomas within the dermis (Fig. 4c, d). The patient declined any treatment and on 6 months follow-up, the lesions appeared unchanged. Lung spirometry and CT scan of his thorax showed hilar lymphadenopathy consistent with sarcoidosis.
Discussion
After the lungs, the skin is the second most common organ to be involved in sarcoidosis [3] with studies showing that in roughly a third of cases it is the presenting manifestation of the disease [4]. All four patients presented with periocular lesions of varying morphology with a diagnosis of sarcoidosis following incisional biopsy of their lesions, demonstrating that this multisystem inflammatory condition can present to adnexal services.
Table 1 summarises the salient characteristics of our cohort. In Prabhakaran et al.’s study of 26 patients with orbital sarcoidosis, all three patients with periocular lid lesions were of Caucasian ethnicity [5]. Similarly, our cohort of four patients is also predominantly Caucasian with only one Afro-Caribbean patient. While the incidence of sarcoidosis overall is higher in Afro-Caribbean individuals [1], particular forms of the cutaneous disease are not. For example, subcutaneous sarcoidosis (Darier–Roussy sarcoidosis) is almost exclusively reported in Caucasians [6].
Given the small nature of our series, it is difficult to draw any meaningful conclusions regarding the usefulness of serum ACE as a diagnostic tool. In a series of 120 patients with cutaneous sarcoidosis, Yanardag et al. found that 56 (47%) patients had an elevated serum ACE [4]. Moreover, they found that 67% of patients had respiratory involvement, which is reflected in our small series with three (75%) patients demonstrating evidence of bilateral hilar lymphadenopathy on chest X-ray.
The most common ophthalmic manifestation of sarcoidosis is acute or chronic uveitis [5]. However, adnexal involvement is rarely associated with intraocular inflammation. Demirci et al., in a retrospective review of 30 patients with biopsy proven adnexal sarcoidosis, found only 3% of patients had concomitant intraocular inflammation. Furthermore, they reported eyelid swelling and eyelid mass as the most common presenting symptoms of adnexal disease, and lid oedema and erythema as the most common findings on examination [2]. The incidence of eyelid involvement in adnexal sarcoidosis ranges from 11.5 to 17% [2, 5] with lid involvement such as “millet seed” nodules, ulcerated nodules, plaques, swelling, anterior and posterior lamella scarring with entropion and lid notching, all previously reported [7, 8]. In each of our four cases, the clinical appearance of each lesion varied indicating that eyelid sarcoidosis may take any morphological appearance and, like ocular sarcoidosis, may mimic other pathology. For example, patient 2 was initially treated with topical steroids for atopic dermatitis and patient 3 was originally referred as a suspected basal cell carcinoma. The violet hue to patient 1’s upper eyelid fullness is characteristic of lupus pernio, which is pathognomonic of cutaneous sarcoid and typically affects the face, specifically the nose. There has previously been one case of biopsy-proven lupus pernio affecting eyelids. This was a 42-year-old African-American woman whose disease was centred on the nose with some involvement of both lower eyelids, which responded to topical steroids.
Acknowledging the usefulness of other diagnostic criteria for sarcoidosis, positive histology on diagnostic biopsy has shown to be an important diagnostic tool in our case. The usual histological features of cutaneous sarcoidosis are dermal infiltrates of non-caseating, non-necrobiotic and non-suppurative granulomas, superficially or throughout the dermis with some degree of fibrosis. Multinucleate giant cells can feature Schaumann bodies. Diagnoses that must be excluded include foreign body reaction, infections, lymphomas, rosacea, acne agnimata and common variable immunodeficiencies. This is particularly relevant to patient 1 with the patient’s occupation as an arc welder, where metallic foreign body injuries are a common occupational hazard requiring a thorough exploration at the time of biopsy. No foreign bodies were found. However, patient 1’s biopsy revealed the presence of perineural granulomas. The differential diagnosis for perineural granulomas includes among others, leprosy, non-tuberculous mycobacterial infection, secondary syphilis, herpes simplex, scleroderma, eosinophilic fasciitis, sarcoidosis, behcet’s disease and cutaneous lupus. Stains for mycobacteria were negative, however, some reports have documented perineural granulomas in sarcoidosis in up to 25% of biopsied cases and some reports have documented small fibre neuropathy [9].
The traditional practice of performing diagnostic biopsy for periocular lesions is crucial and from our experience the authors recommend avoiding superficial biopsies, as key pathological changes are often found within the subcutaneous tissues [6]. Furthermore, patients with cutaneous sarcoidosis should be counselled regarding the risk of recurrence at the biopsy site as scar sarcoidosis following trauma has been reported in the literature [9]. Sarcoidosis can remit spontaneously, and treatment can be targeted to alleviate symptoms and for disfiguring and cosmetically distressing disease [1]. The use of intralesional triamcinolone in the management of sarcoid lesions of the eyelid has been reported in the literature with good effect [10]. Patients 1 and 3 were symptomatic and opted for treatment. Patient 1 did respond to intralesional triamcinolone with almost complete resolution of the lesion, however, as expected the lesion recurred in 3 months when the effect of triamcinolone wore off. Patient 3 did not notice any improvement with the intralesional triamcinolone and opted not to have further treatment. Of note she declined treatment for her pulmonary disease other than the inhalers she was using to give her symptom relief for asthma. Intralesional Fluorouracil (5-FU), however, could represent a steroid-sparing agent with a single report in the literature describing the successful treatment of periocular sarcoid lesions with complete regression and minimal scarring or pigmentary change [11].
Given the potential for local side effects with eyelid involvement, if patients desire treatment, the option of oral corticosteroids and/or systemic immunosuppression can be considered as for patient 1 who benefitted from oral methotrexate with resolution of his cutaneous changes. Despite extensive clinical experience with many treatments for cutaneous sarcoidosis, few have been evaluated in the management of periocular sarcoidosis with no current gold standard regimen. Steroid-sparing agents commonly used in cutaneous sarcoid include systemic methotrexate, antimalarial and tetracyclines therapy with mycophenolate mofetil and Tumour Necrosis Factor Alpha (TNF-α) antagonists reserved for either rapidly disfiguring lesions, recalcitrant disease or concomitant extracutaneous involvement.
Conclusion
Our short series reiterates the importance of the traditional practice of diagnostic biopsy for clinically difficult periocular presentations. It also highlights the varied clinical presentation of periocular sarcoidosis and the importance of having a high degree of clinical suspicion when confronted with such clinical scenarios. This interesting series demonstrates the vital role of oculoplastic surgeons in diagnosing periocular cutaneous sarcoidosis with histopathological confirmation, which in turn can pave the way for a systemic work up as the association of systemic sarcoidosis appears to be as high as 75%. Though there are several anecdotal options of therapy for periocular sarcoidosis, our series demonstrates the need for patient engagement and a potential option of watchful observation as the condition may remain stable even without any therapy.
Summary
What was known before
The skin is the second most common organ to be involved in sarcoidosis.
In one-third of patients, it is the presenting feature of this condition.
What this study adds
Sarcoidosis patients can present to adnexal services with disfiguring eyelid lesions of varying morphology.
Novel illustration of lupus pernio affecting the eyelids.
The therapeutic options of managing periocular sarcoidosis including intralesional triamcinolone and watchful observation over an 18-month period.
References
Haimovic A, Sanchez M, Judson MA, Prystowsky S. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. Cutaneous disease. J Am Acad Dermatol. 2012;66:699.
Demirci H, Christianson MD. Orbital and adnexal involvement in sarcoidosis: analysis of clinical features and systemic disease in 30 cases. Am J Ophthalmol. 2011;151:1074–80.
Noe MH, Rosenbach M. Cutaneous sarcoidosis. Curr Opin Pulm Med. 2017;23:482–6.
Yanardag H, Tetikkurt C, Bilir M, Demirci S, Iscimen A. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
Prabhakaran VC, Saeed P, Esmaeli B, Sullivan TJ, McNab A, Davis G, et al. “Orbital and adnexal sarcoidosis”. Arch Ophthalmol. 2007;125:1657–62.
Wanat KA, Rosenbach M. A practical approach to cutaneous sarcoidosis. Am J Clin Dermatol. 2014;15:283–97.
Collins ME, Petronic-Rosic V, Sweiss NJ, Marcet MM. Full thickness eyelid lesions in sarcoidosis. Case Rep Ophthalmol Med. 2013;2013:579121.
Moin M, Kersten RC, Bernardini F, Kulwin DR. Destructive eyelid lesions in sarcoidosis. Ophthal Plast Reconstr Surg. 2001;17:123–5.
Munday WR, Mcniff J, Watsky K, DiCapua D, Galan AI. Sarcoidosis may be associated with sarcoidosis small-fiber neuropathy. J Cutan Pathol. 2015;42:465–70.
Kim YJ, Kim YD. A case of scar sarcoidosis of the eyelid. Korean J Ophthalmol. 2006;20:238–40.
Gharavi N, Diehl J, Soriano T. Cutaneous sarcoidosis successfully treated with intralesional 5-fluorouracil. Dermatol Surg. 2015;41:1082–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rajput, R., Mathewson, P., Mudhar, H.S. et al. Periocular cutaneous sarcoid: case series and review of the literature. Eye 33, 1590–1595 (2019). https://doi.org/10.1038/s41433-019-0448-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0448-5