Abstract
Background/ Aims
To describe the visual outcomes in eyes with dropped nucleus during phacoemulsification surgery.
Setting
Singapore National Eye Centre (SNEC).
Design
Retrospective chart review of prospectively reported cases of dropped nucleus.
Methods
The clinical charts of all cases of dropped nucleus (Jan 2001 to Dec 2016) were retrospectively reviewed for patient demographics, surgeon type, stage of surgery, timing of pars plana vitrectomy (PPV), and complications. Visual success was defined as best corrected visual acuity (BCVA) ≥ 20/40 at last review. Final risk factors affecting visual success were identified using multivariate logistic regression analysis.
Results
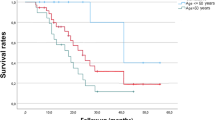
Incidence of dropped nucleus following cataract surgery was 0.17% (n = 292). Duration of follow-up was 25.5 months (mean), 18.5 months (median). There was a statistically significant difference in dropped nucleus rate between Residents (0.3%) and Faculty (0.14%) (x2 = 38.2, P < 0.001), but ensuing major complications rates were similar. PPV was performed in 251 eyes (87.2%). At final examination, 202 cases (85.2%) achieved BCVA 20/40 or better, after excluding patients with co-existing ocular pathology. Timing of vitrectomy (delayed vs same-day) did not influence the final visual success (x2 = 0.969, p = 0.51). Risk factors for poor visual outcomes included age >70 years, absence of intraocular lens (IOL) implant, and presence of major complications.
Conclusion
Overall incidence of dropped nucleus in SNEC was 0.17%, with BCVA of 20/40 or better in 85.2% cases. Visual prognosis was influenced by patient’s age, presence of IOL implant or additional major complications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data used in this study cannot be shared publicly due to privacy concerns in accordance with the Personal Data Protection Act (PDPA) of Singapore. The PDPA safeguards the personal information of individuals and imposes restrictions on the collection, use, and disclosure of such data. The data utilised in this research contain sensitive and personally identifiable information that, if disclosed, could potentially breach the privacy rights of individuals. This includes but is not limited to personal identifiers, contact details, and other confidential information. The research team is committed to upholding the principles of data protection and privacy as outlined by the PDPA. As a result, the data will only be accessible to authorised individuals involved in the study who are bound by strict confidentiality agreements. These individuals will utilise the data solely for the purposes of this study and will not disclose or share it with any unauthorised third parties. While the research findings and conclusions drawn from the data will be disseminated in academic or scientific publications, any information shared will be anonymized or aggregated to ensure that individuals’ privacy is protected. This ensures that no personally identifiable information can be derived from the published results. The restrictions on data availability are implemented to maintain compliance with the PDPA and to ensure the privacy and confidentiality of the individuals involved. The researchers acknowledge the importance of protecting personal data and are dedicated to abiding by the legal and ethical obligations set forth by the PDPA. For any inquiries regarding the data or requests for further information related to the research study, please contact Dr Jeremy Hu at hujeremy@hotmail.com.
References
Osher R. Understanding the dropped nucleus. VJCRGS. 2010;25. https://vjcrgs.com/volume25-issue2/understanding-the-dropped-nucleus.
Ti SE, Yang YN, Lang SS, Chee SP. A 5-year audit of cataract surgery outcomes after posterior capsule rupture and risk factors affecting visual acuity. Am J Ophthalmol. 2014;157:180–5. e1.
Pande M, Dabbs TR. Incidence of lens matter dislocation during phacoemulsification. J Cataract Refract Surg. 1996;22:737–42.
Romero-Aroca P, Fernandez-Ballart J, Mendez-Marin I, Salvat-Serra M, Baget-Bernaldiz M, Buil-Calvo JA. Management of nucleus loss into the vitreous: long term follow up in 63 patients. Clin Ophthalmol. 2007;1:505–12.
Stilma JS, van der Sluijs FA, van Meurs JC, Mertens DA. Occurrence of retained lens fragments after phacoemulsification in The Netherlands. J Cataract Refract Surg. 1997;23:1177–82.
Lundstrom M, Dickman M, Henry Y, Manning S, Rosen P, Tassignon MJ, et al. Risk factors for dropped nucleus in cataract surgery as reflected by the european registry of quality outcomes for cataract and refractive surgery. J Cataract Refract Surg. 2020;46:287–92.
Mathai A, Thomas R. Incidence and management of posteriorly dislocated nuclear fragments following phacoemulsification. Indian J Ophthalmol. 1999;47:173–6.
Tajunisah I, Reddy SC. Dropped nucleus following phacoemulsification cataract surgery. Med J Malays. 2007;62:364–7.
Borne MJ, Tasman W, Regillo C, Malecha M, Sarin L. Outcomes of vitrectomy for retained lens fragments. Ophthalmology. 1996;103:971–6.
Ho LY, Doft BH, Wang L, Bunker CH. Clinical predictors and outcomes of pars plana vitrectomy for retained lens material after cataract extraction. Am J Ophthalmol. 2009;147:587–94. e1.
Merani R, Hunyor AP, Playfair TJ, Chang A, Gregory-Roberts J, Hunyor AB, et al. Pars plana vitrectomy for the management of retained lens material after cataract surgery. Am J Ophthalmol. 2007;144:364–70.
Olsson RB, Ritland JS, Bjornsson OM, Syrdalen P, Eide N, Overgard R. A retrospective study of patients with retained nuclear fragments after cataract extraction. Acta ophthalmol Scand. 2000;78:677–9.
Salam GA, Greene JM, Deramo VA, Tibrewala RK, Ferrone PJ, Fastenberg DM. Retinal tears and retinal detachment as factors affecting visual outcome after cataract extraction complicated by posteriorly dislocated lens material. Retina. 2005;25:570–5.
Scott IU, Flynn HW Jr., Smiddy WE, Murray TG, Moore JK, Lemus DR, et al. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments. Ophthalmology. 2003;110:1567–72.
Smiddy WE, Guererro JL, Pinto R, Feuer W. Retinal detachment rate after vitrectomy for retained lens material after phacoemulsification. Am J Ophthalmol. 2003;135:183–7.
Kapusta MA, Chen JC, Lam WC. Outcomes of dropped nucleus during phacoemulsification. Ophthalmology. 1996;103:1184–7.
Moore JK, Scott IU, Flynn HW Jr., Smiddy WE, Murray TG, Kim JE, et al. Retinal detachment in eyes undergoing pars plana vitrectomy for removal of retained lens fragments. Ophthalmology 2003;110:709–13.
Ho SF, Zaman A. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments after phacoemulsification. J Cataract Refract Surg. 2007;33:2106–10.
Cohen SM, Davis A, Cukrowski C. Cystoid macular edema after pars plana vitrectomy for retained lens fragments. J Cataract Refract Surg. 2006;32:1521–6.
Stefaniotou M, Aspiotis M, Pappa C, Eftaxias V, Psilas K. Timing of dislocated nuclear fragment management after cataract surgery. J Cataract Refract Surg. 2003;29:1985–8.
Rossetti A, Doro D. Retained intravitreal lens fragments after phacoemulsification: complications and visual outcome in vitrectomized and nonvitrectomized eyes. J Cataract Refract Surg. 2002;28:310–5.
Vanner EA, Stewart MW. Vitrectomy timing for retained lens fragments after surgery for age-related cataracts: a systematic review and meta-analysis. Am J Ophthalmol. 2011;152:345–57. e3.
Anteby R, Barzelay A, Barak A. Vitrectomy in patients 85 years of age and older: surgical outcomes and visual prognosis. Clin Interv Aging. 2018;13:243–9.
Chan EW, Yang E, Eldeeb M, Bainbridge JW, da Cruz L, Sullivan PS, et al. Contemporary outcomes and prognostic factors of 23-gauge vitrectomy for retained lens fragments after phacoemulsification. Am J Ophthalmol. 2020;219:271–83.
Jammal AA, Berchuck SI, Thompson AC, Costa VP, Medeiros FA. The effect of age on increasing susceptibility to retinal nerve fiber layer loss in glaucoma. Investig Ophthalmol Vis Sci. 2020;61:8.
Author information
Authors and Affiliations
Contributions
JH: Conceived and designed the study, collected and analysed data, and draughted and revised the manuscript. TSE: contributed to data analysis, and interpretation, and provided substantial manuscript revisions. CSP: Provided guidance in study design, contributed to data analysis and interpretation, and critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, J.Y., Ti, SE. & Chee, SP. Risk factors affecting visual outcomes following dropped nucleus after cataract surgery. Eye 38, 253–258 (2024). https://doi.org/10.1038/s41433-023-02668-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02668-9