Abstract
Objective
The study attempted to identify clinical characteristics associated with structural progression in open-angle glaucoma (OAG) in the presence of MvD in different locations.
Methods
A total of 181 consecutive OAG eyes (follow-up 7.3 ± 4.0 years), which demonstrated peripapillary choroidal MvD (defined as a focal capillary loss with no visible microvascular network in choroidal layer) on optical coherence tomography (OCT) angiography (OCTA), were divided based on the location of MvD. Structural progression was determined using trend-based analysis of the Guided Progression Analysis software of Cirrus OCT.
Results
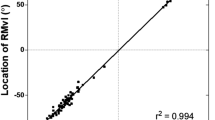
MvD was identified in the temporal quadrant in 110 eyes (temporal MvD; 60.5 ± 12.6 years), and in the inferior quadrant in 71 eyes (inferior MvD; 60.3 ± 11.1 years). After adjusting for age, average intraocular pressure (IOP) and baseline retinal nerve fibre layer (RNFL) thickness and visual field mean deviation, inferior MvD eyes showed faster rates of thinning in the inferior RNFL (mean (95% CI); −0.833 (−1.298 to −0.367)) compared to temporal MvD eyes (−0.144 (−0.496 to 0.207)) when long-term IOP fluctuation was larger than the median value (1.7 mmHg; P = 0.022). Long-term IOP fluctuations were independently associated with inferior RNFL thinning in eyes with inferior MvD (P = 0.002) but not in eyes with temporal MvD.
Conclusions
In OAG eyes, the rates of RNFL and GCIPL thinning were comparable regardless of MvD locations. However, inferior MvD is associated with faster RNFL and GCIPL thinning in the same quadrant when long-term IOP fluctuation is present. Structural progression in the presence of temporal MvD was less associated with IOP fluctuation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to patient confidentiality but are available from the corresponding author on reasonable request.
References
Weinreb RN. Ocular blood flow in glaucoma. Can J Ophthalmol. 2008;43:281–3.
Flammer J, Orgul S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res. 2002;21:359–93.
Kim JA, Son DH, Lee EJ, Kim H, Kim TW. Intereye comparison of the characteristics of the peripapillary choroid in patients with unilateral normal-tension glaucoma. Ophthalmol Glaucoma. 2021;4:512–21.
Lee EJ, Lee KM, Lee SH, Kim TW. Parapapillary choroidal microvasculature dropout in glaucoma: a comparison between optical coherence tomography angiography and indocyanine green angiography. Ophthalmology. 2017;124:1209–17.
Lee EJ, Lee SH, Kim JA, Kim TW. Parapapillary deep-layer microvasculature dropout in glaucoma: topographic association with glaucomatous damage. Investig Ophthalmol Vis Sci. 2017;58:3004–10.
Suh MH, Zangwill LM, Manalastas PI, Belghith A, Yarmohammadi A, Medeiros FA, et al. Deep retinal layer microvasculature dropout detected by the optical coherence tomography angiography in glaucoma. Ophthalmology. 2016;123:2509–18.
Shin JW, Jo YH, Song MK, Won HJ, Kook MS. Nocturnal blood pressure dip and parapapillary choroidal microvasculature dropout in normal-tension glaucoma. Sci Rep. 2021;11:206.
Lee EJ, Kim TW, Kim JA, Kim JA. Central visual field damage and parapapillary choroidal microvasculature dropout in primary open-angle glaucoma. Ophthalmology. 2018;125:588–96.
Park HL, Kim JW, Park CK. Choroidal microvasculature dropout is associated with progressive retinal nerve fiber layer thinning in glaucoma with disc hemorrhage. Ophthalmology. 2018;125:1003–13.
Jo YH, Kwon J, Jeong D, Shon K, Kook MS. Rapid central visual field progression rate in eyes with open-angle glaucoma and choroidal microvasculature dropout. Sci Rep. 2019;9:8525.
Kwon JM, Weinreb RN, Zangwill LM, Suh MH. Juxtapapillary deep-layer microvasculature dropout and retinal nerve fiber layer thinning in glaucoma. Am J Ophthalmol. 2021;227:154–65.
Lee EJ, Kim JA, Kim TW, Kim H, Yang HK, Hwang JM. Glaucoma-like parapapillary choroidal microvasculature dropout in patients with compressive optic neuropathy. Ophthalmology. 2020;127:1652–62.
Shin JW, Lee JY, Lee BJ, Lim HT, Kook MS. Clinical characteristics of choroidal microvasculature dropout in normal-tension glaucoma versus nonarteritic anterior ischemic optic neuropathy: an optical coherence tomography angiography study. Sci Rep. 2021;11:21391.
Mwanza JC, Kim HY, Budenz DL, Warren JL, Margolis M, Lawrence SD, et al. Residual and dynamic range of retinal nerve fiber layer thickness in glaucoma: comparison of three OCT platforms. Investig Ophthalmol Vis Sci. 2015;56:6344–51.
Hood DC, Kardon RH. A framework for comparing structural and functional measures of glaucomatous damage. Prog Retin Eye Res. 2007;26:688–710.
Lee EJ, Kim TW, Kim JA, Kim JA. Parapapillary deep-layer microvasculature dropout in primary open-angle glaucoma eyes with a parapapillary gamma-zone. Investig Ophthalmol Vis Sci. 2017;58:5673–80.
Lee T, Bae HW, Seong GJ, Kim CY, Lee SY. HigH Pulse Wave Velocity Is Associated with Decreased Macular Vessel Density in Normal-tension Glaucoma. Investig Ophthalmol Vis Sci. 2021;62:12.
Lee EJ, Kim JA, Kim TW. Influence of choroidal microvasculature dropout on the rate of glaucomatous progression: a prospective study. Ophthalmol Glaucoma. 2020;3:25–31.
Lin S, Cheng H, Zhang S, Ye C, Pan X, Tao A, et al. Parapapillary choroidal microvasculature dropout is associated with the decrease in retinal nerve fiber layer thickness: a prospective study. Investig Ophthalmol Vis Sci. 2019;60:838–42.
Kwon J, Shin JW, Lee J, Kook MS. Choroidal microvasculature dropout is associated with parafoveal visual field defects in glaucoma. Am J Ophthalmol. 2018;188:141–54.
Micheletti E, Moghimi S, El-Nimri N, Nishida T, Suh MH, Proudfoot JA, et al. Relationship of macular ganglion cell complex thickness to choroidal microvasculature drop-out in primary open-angle glaucoma. Br J Ophthalmol. 2022;107:809–15.
Lee JY, Shin JW, Song MK, Hong JW, Kook MS. An increased choroidal microvasculature dropout size is associated with progressive visual field loss in open-angle glaucoma. Am J Ophthalmol. 2021;223:205–19.
Micheletti E, Moghimi S, Nishida T, El-Nimri N, Mahmoudinedzah G, Kamalipour A, et al. Factors associated with choroidal microvascular dropout change. Br J Ophthalmol. 2022. Epub ahead of print.
Son KY, Han JC, Kee C. Parapapillary deep-layer microvasculature dropout is only found near the retinal nerve fibre layer defect location in open-angle glaucoma. Acta Ophthalmol. 2022;100:e174–80.
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311:1901–11.
Quigley HA, Addicks EM. Regional differences in the structure of the lamina cribrosa and their relation to glaucomatous optic nerve damage. Arch Ophthalmol. 1981;99:137–43.
Kim JH, Caprioli J. Intraocular Pressure Fluctuation: Is It Important? J Ophthalmic Vis Res. 2018;13:170–4.
Hayreh SS. Ischemic optic neuropathy. Prog Retin Eye Res. 2009;28:34–62.
Kaup M, Plange N, Arend KO, Remky A. Retrobulbar haemodynamics in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol. 2006;90:1350–3.
Marshall HN, Andrew NH, Hassall M, Qassim A, Souzeau E, Ridge B, et al. Macular ganglion cell-inner plexiform layer loss precedes peripapillary retinal nerve fiber layer loss in glaucoma with lower intraocular pressure. Ophthalmology. 2019;126:1119–30.
Park HY, Jung KI, Na KS, Park SH, Park CK. Visual field characteristics in normal-tension glaucoma patients with autonomic dysfunction and abnormal peripheral microcirculation. Am J Ophthalmol. 2012;154:466–75.e461.
Yum HR, Park HL, Park CK. Characteristics of normal-tension glaucoma patients with temporal retinal nerve fibre defects. Sci Rep. 2020;10:6362.
Denniss J, Turpin A, McKendrick AM. Relating optical coherence tomography to visual fields in glaucoma: structure-function mapping, limitations and future applications. Clin Exp Optom. 2019;102:291–9.
Fry LE, Fahy E, Chrysostomou V, Hui F, Tang J, van Wijngaarden P, et al. The coma in glaucoma: retinal ganglion cell dysfunction and recovery. Prog Retin Eye Res. 2018;65:77–92.
Malik R, Swanson WH, Garway-Heath DF. ‘Structure-function relationship’ in glaucoma: past thinking and current concepts. Clin Exp Ophthalmol. 2012;40:369–80.
Harwerth RS, Wheat JL, Fredette MJ, Anderson DR. Linking structure and function in glaucoma. Prog Retin Eye Res. 2010;29:249–71.
Miki A, Medeiros FA, Weinreb RN, Jain S, He F, Sharpsten L, et al. Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology. 2014;121:1350–8.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2022R1F1A107625911). The funding organization had no role in the design or conducting of this research.
Author information
Authors and Affiliations
Contributions
Conception and design: HWB. Analysis and interpretation: JSL and HWB. Data collection: JSL, YMP, SP, WC, SYL, and CYK. Obtained funding: HWB. Overall responsibility: JSL and HWB.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, J.S., Park, Y., Park, S. et al. Clinical characteristics of open-angle glaucoma progression with peripapillary microvasculature dropout in different locations. Eye 38, 284–291 (2024). https://doi.org/10.1038/s41433-023-02675-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02675-w