Abstract
Objective
To provide a reference for future policy and measure formulation by conducting a detailed analysis of the burden of vision loss due to cataract by year, age, and gender in China from 1990 to 2019.
Methods
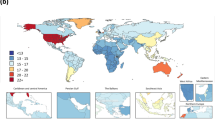
Data on the prevalence and disability-adjusted life-years (DALYs) due to cataract in China and neighboring and other G20 countries were extracted from the 2019 Global Burden of Disease (GBD) study to observe the changing trends of vision loss.
Results
The number and rate of all-age prevalence and DALYs for cataract in China increased significantly from 1990 to 2019. The age-standardized DALYs rate witnessed a slowly declining trend by 10.16%. And the age-standardized prevalence increased by 14.35% over the 30-year period. Higher prevalence and DALYs were observed in female population from 1990 through 2019, with little improvement over the decades(all p < 0.001). The disease burden of cataract is higher in middle-aged and elderly people. Blindness accounted for the largest proportion of vision impairment burden caused by cataract in China. The age-standardized prevalence and DALY rate of cataract in China were lower than those in India and Pakistan, but higher than those in Russia, South Korea, North Korea, Singapore, and Japan.
Conclusions
In the past 30 years, although the age-standardized DALYs rate has decreased slightly in China, the all-age prevalence and DALYs have both increased. This study highlights the importance of reducing cataract burden by providing timely and easily accessible quality care, especially in females and the elderly population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ruiss M, Findl O, Kronschläger M. The human lens: an antioxidant-dependent tissue revealed by the role of caffeine. Ageing Res Rev. 2022;79:101664.
Naidoo K, Kempen JH, Gichuhi S, Braithwaite T, Casson RJ, Cicinelli MV, et al. Prevalence and causes of vision loss in sub-Saharan Africa in 2015: magnitude, temporal trends and projections. Br J Ophthalmol. 2020;104:1658–68.
Lee CM, Afshari NA. The global state of cataract blindness. Curr Opin Ophthalmol. 2017;28:98–103.
Khairallah M, Kahloun R, Bourne R, Limburg H, Flaxman SR, Jonas JB, et al. Number of people blind or visually impaired by cataract worldwide and in world regions, 1990 to 2010. Investig Ophthalmol Vis Sci. 2015;56:6762–9.
Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–8.
Lee CS, Gibbons LE, Lee AY, Yanagihara RT, Blazes MS, Lee ML, et al. Association between cataract extraction and development of dementia. JAMA Intern Med. 2022;182:134–41.
Foss A. Prompt access to cataract surgery is vital for preventing falls in older people. Med J Aust. 2022;217:84–85.
Keay L, Ho KC, Rogers K, McCluskey P, White AJ, Morlet N, et al. The incidence of falls after first and second eye cataract surgery: a longitudinal cohort study.[J]. Med J Aust. 2022;217:94–99.
Wang W, Yan W, Müller A, He M. A global view on output and outcomes of cataract surgery with national indices of socioeconomic development. Investig Ophthalmol Vis Sci. 2017;58:3669–76.
Lundström M, Dickman M, Henry Y, Manning S, Rosen P, Tassignon MJ, et al. Changing practice patterns in European cataract surgery as reflected in the European registry of quality outcomes for cataract and refractive surgery 2008 to 2017. J Cataract Refract Surg. 2021;47:373–8.
McCormick I, Butcher R, Evans JR, Mactaggart IZ, Limburg H, Jolley E, et al. Effective cataract surgical coverage in adults aged 50 years and older: estimates from population-based surveys in 55 countries. Lancet Glob Health. 2022;10:e1744–53.
Armstrong KL, Jovic M, Vo-Phuoc JL, Thorpe JG, Doolan BL. The global cost of eliminating avoidable blindness. Indian J Ophthalmol. 2012;60:475–80.
Tu WJ, Zeng X, Liu Q. Aging tsunami coming: the main finding from China’s seventh national population census. Aging Clin Exp Res. 2022;34:1159–63.
Sun Y, Chen A, Zou M, Liu Z, Young CA, Zheng D, et al. Disease burden of glaucoma in China: findings from the Global Burden of Disease 2019 Study. Clin Epidemiol. 2022;14:827–34.
Shan Y, Xu Y, Lin X, Lou L, Wang Y, Ye J. Burden of vision loss due to diabetic retinopathy in China from 1990 to 2017: findings from the global burden of disease study. Acta Ophthalmol. 2021;99:e267–73.
Lin Y, Gao L, Jiang W. Analysis of the epidemiological burden of age-related macular degeneration in China based on the data of global burden of disease. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2023;48:106–13.
Xu T, Wang B, Liu H, Wang H, Yin P, Dong W, et al. Prevalence and causes of vision loss in China from 1990 to 2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health. 2020;5:e682–91.
GBD 2019. Diseases and injuries collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Fang R, Yu YF, Li EJ, Lv NX, Liu ZC, Zhou HG, et al. Global, regional, national burden and gender disparity of cataract: findings from the global burden of disease study 2019. BMC Public Health. 2022;22:2068.
He M, Wang W, Huang W. Variations and trends in health burden of visual impairment due to cataract: a global analysis. Investig Ophthalmol Vis Sci. 2017;58:4299–306.
Lou L, Wang J, Xu P, Ye X, Ye J. Socioeconomic disparity in global burden of cataract: an analysis for 2013 with time trends since 1990. Am J Ophthalmol. 2017;180:91–96.
GBD 2017. Disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The lancet global health commission on global eye health: vision beyond 2020. Lancet Glob Health. 2021;9:e489–551.
Bourne RRA. Vision 2020: where are we?. Curr Opin Ophthalmol. 2020;31:81–84.
Feng Q, Yeung WJ, Wang Z, Zeng Y. Age of retirement and human capital in an aging China, 2015-2050. Eur J Popul. 2018;35:29–62.
Li HY, Liu YM, Dong L, Zhang RH, Zhou WD, Wu HT, et al. Global, regional, and national prevalence, disability adjusted life years, and time trends for refraction disorders, 1990-2019: findings from the global burden of disease study 2019. BMC Public Health. 2021;21:1619.
Zhang Y, Zou B, Zhang H, Zhang J. Empirical research on male preference in China: a result of gender imbalance in the seventh population census. Int J Environ Res Public Health. 2022;19:6482.
Ono K, Hiratsuka Y, Murakami A. Global inequality in eye health: country-level analysis from the Global Burden of Disease Study. Am J Public Health. 2010;100:1784–8.
Resnikoff S, Lansingh VC, Washburn L, Felch W, Gauthier TM, Taylor HR, et al. Estimated number of ophthalmologists worldwide (International Council of Ophthalmology update): will we meet the needs? Br J Ophthalmol. 2020;104:588–92.
An L, Jan CL, Feng J, Wang Z, Zhan L, Xu X. Inequity in access: cataract surgery throughput of chinese ophthalmologists from the China National Eye Care capacity and resource survey. Ophthalmic Epidemiol. 2020;27:29–38.
Wu X, Shi X, Li H, Guo Z. Temporal and spatial characteristics of cataract surgery rates in China. Risk Manag Healthc Policy. 2021;14:3551–61.
Funding
National Natural Science Foundation of China (82271067). The funding organizations had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
RF developed the concept for the manuscript, enrollment of participants, data gathering and drafting the manuscript, and conducted data analysis. XFD, PLY, NXL, ZL and YXJ critically verified the data obtained from the GBD database. HGZ and XDS drafted and revised the manuscript. XDS and HGZ contributed equally to this work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fang, R., Yue, PL., Ding, XF. et al. The burden of vision loss due to cataract in China: findings from the Global Burden of Disease Study 2019. Eye 38, 885–892 (2024). https://doi.org/10.1038/s41433-023-02798-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02798-0