Abstract
Purpose
To evaluate the association between dry eye disease (DED) and various psychiatric and systemic diseases in an adult Korean population aged 40 years or older.
Methods
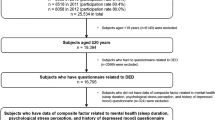
Population-based cross-sectional data of 6,732 participants aged ≥40 years was extracted from the Korea National Health and Nutrition Examination Survey 2017–2018 (KNHANES VII). Data including DED, demographic variables, behavioral factors, psychiatric conditions, and systemic diseases was analysed to determine the prevalence and psychiatric and systemic risk factors for DED.
Results
The weighted prevalence of DED was 7.9 ± 0.4% (mean ± SE). Multivariate analysis showed that female sex and urban residence were associated with an increased risk of DED. The prevalence of DED was lower in patients aged ≥70 years than in those aged 40–69 years. Self-reported psychological conditions including perceived stress and depression were associated with the risk of DED. Self-reported Systemic conditions, such as rheumatoid arthritis, degenerative arthritis, osteoporosis, ischemic heart disease, and chronic renal failure had association with an increased risk of DED.
Conclusion
DED may be associated with several self-reported psychiatric and systemic conditions, which highlights the need for an integrated approach to manage these diseases for optimal treatment of DED.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data are available from the Korea Center for Chronic Disease and Control Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data. Data can also be downloaded from the following website: https://knhanes.cdc.go.kr/knhanes/eng/index.do.
References
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–65.
Qian L, Wei W. Identified risk factors for dry eye syndrome: a systematic review and meta-analysis. PloS One. 2022;17:e0271267.
Hyon JY, Yang HK, Han SB. Dry eye symptoms may have association with psychological stress in medical students. Eye and Contact lens. 2019;45:310–4.
Hyon JY, Yang HK, Han SB. Association between dry eye disease and psychological stress among paramedical workers in Korea. Sci Rep. 2019;9:3783.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Sayegh RR, Yu Y, Farrar JT, Kuklinski EJ, Shtein RM, Asbell PA, et al. ocular discomfort and quality of life among patients in the dry eye assessment and management study. Cornea. 2021;40:869–76.
Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–15.
Morthen MK, Magno MS, Utheim TP, Snieder H, Hammond CJ, Vehof J. The physical and mental burden of dry eye disease: a large population-based study investigating the relationship with health-related quality of life and its determinants. Ocul Surf. 2021;21:107–17.
Wolffsohn JS, Wang MTM, Vidal-Rohr M, Menduni F, Dhallu S, Ipek T, et al. Demographic and lifestyle risk factors of dry eye disease subtypes: a cross-sectional study. Ocu Surf. 2021;21:58–63.
Wang MTM, Muntz A, Mamidi B, Wolffsohn JS, Craig JP. Modifiable lifestyle risk factors for dry eye disease. Contact lens & Anterior Eye. 2021;44:101409.
Vehof J, Snieder H, Jansonius N, Hammond CJ. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul Surf. 2021;19:83–93.
Roh HC, Lee JK, Kim M, Oh JH, Chang MW, Chuck RS, et al. Systemic comorbidities of dry eye syndrome: the Korean National Health and Nutrition Examination Survey V, 2010 to 2012. Cornea. 2016;35:187–92.
Kim KW, Han SB, Han ER, Woo SJ, Lee JJ, Yoon JC, et al. Association between depression and dry eye disease in an elderly population. Invest Ophthalmol Vis Sci. 2011;52:7954–8.
García-Marqués JV, Talens-Estarelles C, García-Lázaro S, Wolffsohn JS, Cerviño A. Systemic, environmental and lifestyle risk factors for dry eye disease in a mediterranean caucasian population. Contact lens & Anterior Eye. 2021;45:101539.
Wang MT, Muntz A, Wolffsohn JS, Craig JP. Association between dry eye disease, self-perceived health status, and self-reported psychological stress burden. Clin Exp Optom. 2021: 1−6.
Wang MTM, Vidal-Rohr M, Muntz A, Diprose WK, Ormonde SE, Wolffsohn JS, et al. Systemic risk factors of dry eye disease subtypes: a New Zealand cross-sectional study. Ocul Surf. 2020;18:374–80.
Han SB, Jang J, Yang HK, Hwang JM, Park SK. Prevalence and risk factors of myopia in adult Korean population: Korea national health and nutrition examination survey 2013-2014 (KNHANES VI). PloS One. 2019;14:e0211204.
Han SB, Hyon JY, Woo SJ, Lee JJ, Kim TH, Kim KW. Prevalence of dry eye disease in an elderly Korean population. Arch Ophthalmol. 2011;129:633–8.
Uchino M, Dogru M, Uchino Y, Fukagawa K, Shimmura S, Takebayashi T, et al. Japan ministry of health study on prevalence of dry eye disease among Japanese high school students. Am J Ophthalmol. 2008;146:925–929.e922.
Uchino M, Schaumberg DA, Dogru M, Uchino Y, Fukagawa K, Shimmura S, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115:1982–8.
McMonnies CW. Why the symptoms and objective signs of dry eye disease may not correlate. J Optom. 2021;14:3–10.
Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140:774–815.
Geva N, Pruessner J, Defrin R. Acute psychosocial stress reduces pain modulation capabilities in healthy men. Pain. 2014;155:2418–25.
Burton T, Farley D, Rhea A. Stress-induced somatization in spouses of deployed and nondeployed servicemen. J Am Acad Nurse Practitioners. 2009;21:332–9.
Wan KH, Chen LJ, Young AL. Depression and anxiety in dry eye disease: a systematic review and meta-analysis. Eye. 2016;30:1558–67.
Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron. 2020;107:234–56.
Wang TJ, Wang IJ, Hu CC, Lin HC. Comorbidities of dry eye disease: a nationwide population-based study. Acta Ophthalmol. 2012;90:663–8.
Jeng YT, Lin SY, Hu HY, Lee OK, Kuo LL. Osteoporosis and dry eye syndrome: a previously unappreciated association that may alert active prevention of fall. PloS one. 2018;13:e0207008.
Shokr H, Wolffsohn JS, Trave Huarte S, Scarpello E, Gherghel D. Dry eye disease is associated with retinal microvascular dysfunction and possible risk for cardiovascular disease. Acta Ophthalmol. 2021;99:e1236–e1242.
Chen W, Batawi HI, Alava JR, Galor A, Yuan J, Sarantopoulos CD, et al. Bulbar conjunctival microvascular responses in dry eye. Ocul Surf. 2017;15:193–201.
Aktaş S, Sağdık HM, Aktaş H, Gülcan E, Tetikoğlu M, Coşgun S, et al. Tear function in patients with chronic renal failure undergoing hemodialysis. Ren Fail. 2015;37:245–8.
Akinci A, Cakar N, Kara N, Uncu N. Ocular findings in children with chronic renal failure. Cornea. 2009;28:5–6.
Yoo TK, Oh E. Diabetes mellitus is associated with dry eye syndrome: a meta-analysis. Int Ophthalmol. 2019;39:2611–20.
Funding
This paper was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (Grant No. NRF- 2021R1F1A1048448).
Author information
Authors and Affiliations
Contributions
MNL is responsible for design of the study protocol, acquisition and analysis of the data, literature search, and drafting the work. JYL is responsible for design of the study protocol, acquisition and interpretation of the data, literature search, and drafting the work. JYH is responsible for conception of the study protocol, analysis and interpretation of the data, and critical revision of the work. SBH is responsible for conception and design of the study protocol, analysis and interpretation of the data, and critical revision of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lim, M.N., Lee, J.Y., Hyon, J.Y. et al. Association of self-reported psychiatric and systemic risk factors in dry eye disease in adult Korean population. Eye 38, 917–922 (2024). https://doi.org/10.1038/s41433-023-02803-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02803-6
This article is cited by
-
Is there a relationship between the severity of disease in major depressive disorder patients and dry eye disease?
International Ophthalmology (2024)