Abstract
Background
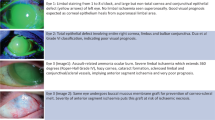
South Asia is experiencing rapid urbanization, which may be changing the risk factor profile for ocular trauma. The objective of this study was to compare risk factors for traumatic corneal abrasions in rural versus urban Nepal, and to assess if any risk factors were associated with a poor outcome.
Methods
In a prospective, cross-sectional, community-based study performed as part of a cluster-randomized trial, community health workers from Nepal were trained to diagnose and treat traumatic corneal abrasions. Participants with an abrasion were invited to complete a risk factor survey. The main exposure variable was the object of eye injury, stratified by rural-urban residence. The main outcome measure was a lack of corneal healing after a three-day course of antimicrobials.
Results
Of 3657 participants diagnosed with a corneal abrasion, 2265 completed a survey. Eye trauma occurred most frequently during agricultural activities. The most common object of injury was vegetative matter, accounting for approximately 40% of injuries in rural, peri-urban, and urban communities. Wood injuries were more common in rural communities (24%) compared with urban or peri-urban communities (13%). Eye injury from an animal was more likely to result in a non-healing corneal abrasion after 3 days of treatment compared with other types of trauma (prevalence ratio 2.59, 95%CI 1.16–5.76).
Conclusions
Health promotion activities for prevention of corneal ulcers in Nepal should focus on agricultural trauma in both rural and urban areas. Community members experiencing eye trauma from an animal may benefit from early referral to an eye clinic.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author, JDK.
References
Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221–34.
Vashist P, Senjam SS, Gupta V, Gupta N, Shamanna BR, Wadhwani M, et al. Blindness and visual impairment and their causes in India: Results of a nationally representative survey. PLoS One. 2022;17:e0271736.
Srinivasan M, Gonzales CA, George C, Cevallos V, Mascarenhas JM, Asokan B, et al. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br J Ophthalmol. 1997;81:965–71.
Upadhyay MP, Karmacharya PC, Koirala S, Shah DN, Shakya S, Shrestha JK, et al. The Bhaktapur eye study: ocular trauma and antibiotic prophylaxis for the prevention of corneal ulceration in Nepal. Br J Ophthalmol. 2001;85:388–92.
Upadhyay MP, Karmacharya PC, Koirala S, Tuladhar NR, Bryan LE, Smolin G, et al. Epidemiologic characteristics, predisposing factors, and etiologic diagnosis of corneal ulceration in Nepal. Am J Ophthalmol. 1991;111:92–9.
Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992;20:95–8.
Getshen K, Srinivasan M, Upadhyay MP, Priyadarsini B, Mahalaksmi R, Whitcher JP. Corneal ulceration in South East Asia. I: a model for the prevention of bacterial ulcers at the village level in rural Bhutan. Br J Ophthalmol. 2006;90:276–8.
O’Brien KS, Byanju R, Kandel RP, Poudyal B, Gonzales JA, Porco TC, et al. Village-integrated eye workers for prevention of corneal ulcers in Nepal (VIEW study): a cluster-randomised controlled trial. Lancet Glob Health. 2022;10:e501–09.
O’Brien KS, Byanju R, Kandel RP, Poudyal B, Gautam M, Gonzales JA, et al. Village-Integrated Eye Worker trial (VIEW): rationale and design of a cluster-randomised trial to prevent corneal ulcers in resource-limited settings. BMJ Open. 2018;8:e021556.
Bhandari S, Nesemann JM, Kandel RP, Poudyal B, Bhandari G, Byanju R, et al. Knowledge and practices in the diagnosis and treatment of corneal infections by nepalese pharmaceutical shop workers. Am J Trop Med Hyg. 2020;103:1694–6.
Government of Nepal Central Bureau of Statistics. National population and housing census 2011. Available at: https://unstats.un.org/unsd/demographic-social/census/documents/Nepal/Nepal-Census-2011-Vol1.pdf. Accessed February 15, 2023.
Chatterjee S, Agrawal D. Primary prevention of ocular injury in agricultural workers with safety eyewear. Indian J Ophthalmol. 2017;65:859–64.
Funding
This study was supported by the National Eye Institute (U10EY022880), the Peierls Foundation, the ALTA Foundation, the All May See Foundation, and Research to Prevent Blindness.
Author information
Authors and Affiliations
Consortia
Contributions
Concept and design: SRB, RPK, MS, MU, JPW, KSO, TML, JDK. Acquisition, analysis, or interpretation of data: SRB, PG, RB, GB, SB, RPK, BP, JAG, KSO, TML, JDK. Drafting of the manuscript: SRB and JDK. Critical revision of the manuscript for important intellectual content: All authors. Administrative, technical, or material support: PG, SB, SP. Supervision: PG, RB, SP, GB, SB, RPK, BP, MS, MU, JPW, KSO, TML, JDK.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A list of members and their affiliations appears in the Supplementary Information.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brekke, S.R., Giri, P., Byanju, R. et al. Risk factors for corneal abrasions in Nepal: a community-based study. Eye 38, 945–950 (2024). https://doi.org/10.1038/s41433-023-02809-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02809-0