Abstract
Introduction
Glauc-Strat-Fast is a clinical tool recommended by The Royal College of Ophthalmologists to classify glaucoma patients into strata of risk for significant future sight loss and an estimate of resource requirement. The aim of this study was to map the movement of glaucoma patients across stratification boundaries on Glauc-Strat-Fast during the COVID-19 pandemic.
Subjects and methods
Glauc-Strat-Fast was applied to a consecutive sample of 100 primary open angle glaucoma patients in a backlog at Worcestershire Acute Hospitals NHS Trust. Stratification outcomes were compared between clinic visits prior to the COVID-19 pandemic versus the follow-up visit. Patients were stratified twice separately based on their worse eye (i.e., most affected) and better eye (i.e., least affected) according to Glauc-Strat-Fast.
Results
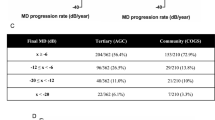
Amount of slippage (difference between target follow-up and actual follow-up) ranged from 2 to 32 months. There was a statistically significant average reduction in visual field mean deviation for better and worse eyes between visits (p = <0.001). At follow-up, no worse eyes were classified as being low risk (green), while 96 were classified as high risk (red). For better eyes, elevation of risk into the highest strata of Glauc-Strat-Fast observed a three-fold increase in patients (19 versus 56) between visits.
Discussion
This retrospective real-world analysis highlights patients’ movement into the highest strata on the Glauc-Strat-Fast tool and demonstrates a significant deterioration in visual outcomes during a period of extensive appointment slippage. The findings demonstrate the utility of Glauc-Strat-Fast as a tool for improved patient management.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Cousins MS, Shickle LM, Bander JA. An introduction to predictive modeling for disease management risk stratification. Dis Manag. 2002;5:157–67.
Kharrazi H, Chi W, Chang HY, Richards TM, Gallagher JM, Knudson SM, et al. Comparing population-based risk-stratification model performance using demographic, diagnosis and medication data extracted from outpatient electronic health records versus administrative claims. Med Care. 2017;55:789–96.
NHS Digital. Available at: Hospital Outpatient Activity 2020-21 - NHS Digital. Accessed 20 Nov 2022.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–90.
The Royal College of Ophthalmologists. Workforce census, 2018. Available at: New RCOphth Workforce Census illustrates the severe shortage of eye doctors in the UK | The Royal College of Ophthalmologists. Accessed 20 Nov 2022.
Healthcare Safety Investigation Branch. Lack of timely monitoring of patients with glaucoma, 2020. Available at: Lack of timely monitoring of patients with glaucoma | HSIB. Accessed 20 Nov 2022.
Tatham A, Murdoch I. The effect of appointment rescheduling on monitoring interval and patient attendance in the glaucoma outpatient clinic. Eye. 2012;26:729–33.
Clarke J, Puertas R, Kotecha A, Foster PJ, Barton K. Virtual clinics in glaucoma care: face-to-face versus remote decision-making. Br J Ophthalmol. 2017;101:892–5.
Jones L, Bryan SR, Miranda MA, Crabb DP, Kotecha A. Example of monitoring measurements in a virtual eye clinic using ‘big data’. Br J Ophthalmol. 2018;102:911–5.
Harper RA, Gunn PJ, Spry PG, Fenerty CH, Lawrenson JG. Care pathways for glaucoma detection and monitoring in the UK. Eye. 2020;34:89–102.
The Royal College of Ophthalmologists. Joint RCOphth and UKEGS glaucoma risk stratification tool. Available at: Glaucoma Risk Stratification Tool August 2020.docx. Accessed 20 Nov 2022.
Shah P Guidance on glaucoma. Medical Defence Union Journal. Available at: Guidance on glaucoma (themdu.com). Accessed 23 Feb 2023.
Konstantakopoulou E, Kastner A, Gazzard G, Jayaram H. Validation of the RCOphth and UKEGS glaucoma risk stratification tool ‘GLAUC-STRAT-fast’. Br J Ophthalmol. 2023;107:1258–63.
The Royal College of Ophthalmologists. Designing glaucoma care pathways using Glauc-Strat-Fast. Available at: Designing Glaucoma Care Pathways using GLAUC-STRAT-FAST | The Royal College of Ophthalmologists (rcophth.ac.uk). Accessed 23 Feb 2023.
Jayaram H, Strouthidis NG, Gazzard G. The COVID-19 pandemic will redefine the future delivery of glaucoma care. Eye. 2020;34:1203–5.
Jayaram H, Baneke AJ, Adesanya J, Gazzard G. Managing risk in the face of adversity: design and outcomes of rapid glaucoma assessment clinics during a pandemic recovery. Eye. 2022;36:1799–803.
Hodapp E, Parrish II RK, Anderson DR Clinical Decisions in Glaucoma. St. Louis, Missouri: Mosby Yearbook, 1993.
The Royal College of Ophthalmologists. Measuring follow up timeliness and risk for performance reporting, improvement actions and targeting failsafe procedures in England, 2020. Available at: Measuring-follow-up-timeliness-and-risk-for-performance-reporting-improvement-actions-and-targeting-failsafe-procedures-in-England.pdf (rcophth.ac.uk). Accessed 22 Sep 2023.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. “Hand motion” and “counting fingers” can be quantified using the Freiburg visual acuity test. Invest Ophthalmol Vis Sci. 2006;47:1236–40.
Heijl A, Aspberg J, Bengtsson B. The effect of different criteria on the number of patients blind from open-angle glaucoma. BMC Ophthalmol. 2011;11:31.
Chauhan BC, Malik R, Shuba LM, Rafuse PE, Nicolela MT, Artes PH. Rates of glaucomatous visual field change in a large clinical population. Investig Ophthalmol Vis Sci. 2014;55:4135–43.
Gardiner SK, Crabb DP. Examination of different pointwise linear regression methods for determining visual field progression. Investi Ophthalmol Vis Sci. 2002;43:1400–7.
De Moraes CG, Juthani VJ, Liebmann JM, Teng CC, Tello C, Susanna R, et al. Risk factors for visual field progression in treated glaucoma. Arch Ophthalmol. 2011;129:562–8.
Medeiros FA, Jammal AA. Validation of rates of mean deviation change as clinically relevant end points for glaucoma progression. Ophthalmology. 2023;130:469–77.
Kirwan JF, Hustler A, Bobat H, Toms L, Crabb DP, McNaught AI. Portsmouth visual field database: an audit of glaucoma progression. Eye. 2014;28:974–9.
COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–9.
Thomas DS, Warwick A, Olvera-Barrios A, Egan C, Schwartz R, Patra S, et al. Estimating excess visual loss in people with neovascular age-related macular degeneration during the COVID-19 pandemic. MedRxiv, 2020.
Allegrini D, Raimondi R, Montesano G, Borgia A, Sorrentino T, Tsoutsanis P, et al. Short-term outcomes after COVID-19-related treatment interruption among patients with neovascular age-related macular degeneration receiving intravitreal Bevacizumab. Clin Ophthalmol. 2021;15:4073–9.
Getting It Right First Time. Ophthalmology, GIRFT Programme National Speciality Report. Available at: Ophthalmology – Getting It Right First Time – GIRFT. Accessed 20 Nov 2022.
Marks JR, Harding AK, Harper RA, Williams E, Haque S, Spencer AF, et al. Agreement between specially trained and accredited optometrists and glaucoma specialist consultant ophthalmologists in their management of glaucoma patients. Eye. 2012;26:853–61.
Jones L, Konstantakopoulou E, Gazzard G. Selective laser trabeculoplasty (SLT) performed by optometrists for patients with glaucoma and ocular hypertension: a scoping review. BMJ Open Ophthalmol. 2021;6:e000611.
Turner S, Vasilakis C, Utley M, Foster P, Kotecha A, Fulop NJ. Analysing barriers to service improvement using a multi‐level theory of innovation: the case of glaucoma outpatient clinics. Sociol Health Illn. 2018;40:654–69.
Burgos-Blasco B, Vidal-Villegas B, Yap TE, Normando EM, Ameen S, Crawley L, et al. Effects of COVID-19 pandemic on glaucoma appointment scheduling in a tertiary hospital in London, UK. Eur J Ophthalmol. 2023. https://doi.org/10.1177/11206721231171704.
Heijl A, Buchholz P, Norrgren G, Bengtsson B. Rates of visual field progression in clinical glaucoma care. Acta Ophthalmol. 2013;91:406–12.
Saunders LJ, Russell RA, Kirwan JF, McNaught AI, Crabb DP. Examining visual field loss in patients in glaucoma clinics during their predicted remaining lifetime. Investig Ophthalmol Vis Sci. 2014;55:102–9.
Olmastroni E, Galimberti F, Tragni E, Catapano AL, Casula M. Impact of COVID-19 pandemic on adherence to chronic therapies: a systematic review. Int J Environ Res Public Health. 2023;20:3825.
Racette L, Abu SL, Poleon S, Thomas T, Sabbagh N, Girkin CA. The impact of the coronavirus disease 2019 pandemic on adherence to ocular hypotensive medication in patients with primary open-angle glaucoma. Ophthalmology. 2022;129:258–66.
Subathra GN, Rajendrababu SR, Senthilkumar VA, Mani I, Udayakumar B. Impact of COVID-19 on follow-up and medication adherence in patients with glaucoma in a tertiary eye care centre in south India. Indian J Ophthalmol. 2021;69:1264.
Kang JM, Chatterjee A, Rosdahl JA, Bosworth HB, Woolson S, Olsen M, et al. Health literacy and success with glaucoma drop administration. Ophthalmol Glaucoma. 2022;5:26–31.
Zhou W, Lin H, Ren Y, Lin H, Liang Y, Chen Y, et al. Mental health and self-management in glaucoma patients during the COVID-19 pandemic: a cross-sectional study in China. BMC Ophthalmol. 2022;22:1–8.
Lešin Gaćina D, Jandroković S, Marčinko D, Škegro I, Vidas Pauk S, Tomić M, et al. Anxiety and treatment adherence among glaucoma patients during COVID-19 pandemic and earthquakes in Croatia. Psychiatr Danubina. 2022;34:348–55.
Sleath B, Blalock SJ, Robin A, Hartnett ME, Covert D, DeVellis B, et al. Development of an instrument to measure glaucoma medication self-efficacy and outcome expectations. Eye. 2010;24:624–31.
Baker DW. Trust in health care in the time of COVID-19. JAMA. 2020;324:2373–5.
Lane M, Lane V, Abbott J, Braithwaite T, Shah P, Denniston AK. Multiple deprivation, vision loss, and ophthalmic disease in adults: global perspectives. Surv Ophthalmol. 2018;63:406–36.
Peters D, Heijl A, Brenner L, Bengtsson B. Visual impairment and vision‐related quality of life in the early manifest glaucoma trial after 20 years of follow‐up. Acta Ophthalmol. 2015;93:745–52.
Gutierrez P, Wilson MR, Johnson C, Gordon M, Cioffi GA, Ritch R, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–84.
Parrish RK, Gedde SJ, Scott IU, Feuer WJ, Schiffman JC, Mangione CM, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–55.
Mills RP, Janz NK, Wren PA, Guire KE. Cigts Study Grp. Correlation of visual field with quality-of-life measures at diagnosis in the Collaborative Initial Glaucoma Treatment Study (CIGTS). J Glaucoma. 2001;10:192–8.
Sumi I, Shirato S, Matsumoto S, Araie M. The relationship between visual disability and visual field in patients with glaucoma. Ophthalmology. 2003;110:332–9.
Hyman LG, Komaroff E, Heijl A, Bengtsson B, Leske MC. Treatment and vision related quality of life in the early manifest glaucoma trial. Ophthalmology. 2005;112:1505–13.
McKean-Cowdin R, Wang Y, Wu J, Azen SP, Varma R, Los Angeles Latino Eye Study Group. Impact of visual field loss on health-related quality of life in glaucoma – The Los Angeles Latino Eye Study. Ophthalmology. 2008;115:941–8.
van Gestel A, Webers CAB, Beckers HJM, van Dongen M, Severens JL, Hendrikse F, et al. The relationship between visual field loss in glaucoma and health related quality-of-life. Eye. 2010;24:1759–69.
Jones L, Taylor DJ, Sii F, Masood I, Crabb DP, Shah P. Only eye study 2 (OnES 2):‘Am I going to be able to see when the patch comes off?’A qualitative study of patient experiences of undergoing high-stakes only eye surgery. BMJ Open. 2020;10:e038916.
Jones L, Taylor DJ, Sii F, Masood I, Crabb DP, Shah P. The Only Eye Study (OnES): a qualitative study of surgeon experiences of only eye surgery and recommendations for patient safety. BMJ Open. 2019;9:e030068.
Whyte JP, Lee G, Jones L, Shah P. Only eye study 3 (OnES 3): a qualitative study into how surgeons approach surgery in patients with only one seeing eye. BMJ Open. 2022;12:e064597.
Bommakanti NK, Zhou Y, Ehrlich JR, Elam AR, John D, Kamat SS, et al. Application of the sight outcomes research collaborative ophthalmology data repository for triaging patients with glaucoma and clinic appointments during pandemics such as COVID-19. JAMA Ophthalmol. 2020;138:974–80.
Russell RA, Garway-Heath DF, Crabb DP. New insights into measurement variability in glaucomatous visual fields from computer modelling. PloS One. 2013;30:e83595.
Wormald R, Basauri E, Wright L, Evans J. The African Caribbean eye survey: risk factors for glaucoma in a sample of African Caribbean people living in London. Eye. 1994;8:315–20.
Heinze N, Jones L, Makwana B. A rapid review of evidence relating to service use, experiences, and support needs of adults from minority ethnic communities along the eyecare pathway in the United Kingdom. Front Public Health. 2023;28:1119540.
Author information
Authors and Affiliations
Contributions
OS: Data acquisition, Data analysis, Revising the manuscript. LJ: Data analysis, Data visualisation, Writing the manuscript. FS: Conceptualisation, Data analysis, Revising the manuscript. JW: Data analysis, Revising the manuscript. SD: Revising the manuscript. GL: Revising the manuscript. JK: Revising the manuscript. TS: Conceptualisation, Data acquisition, Revising the manuscript. PS: Conceptualisation, Data analysis, Data Visualisation, Revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sharma, O., Jones, L., Sii, F. et al. Mapping vision loss of patients in a glaucoma backlog following the COVID-19 pandemic: a real-world analysis using the Glauc-Strat-Fast risk stratification tool. Eye 38, 1005–1011 (2024). https://doi.org/10.1038/s41433-023-02821-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02821-4