Abstract
Background/objectives
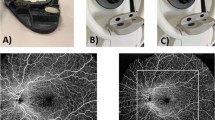
To evaluate the diagnostic performance of B-scan kinetic ultrasonography (USG), standard ultra-widefield (UWF) imaging, and indirect ophthalmoscopy (IDO) in retinal break detection in cataractous eyes.
Subjects/methods
We consecutively enrolled 126 cataract patients (including 246 eyes) with no comorbidities that could decrease best corrected visual acuity (BCVA). Three index tests (USG, nonmydriatic UWF, and mydriatic IDO) were performed preoperatively to screen for retinal breaks. One week after cataract extraction, a dilated IDO examination was repeated for the definitive diagnosis of retinal break as the reference standard. The sensitivity, specificity, Youden index (YI), and predictive values of each index test were calculated according to postoperative ophthalmoscopic findings. A deep-learning nomogram was developed to quantify the risk of retinal break presence using patients’ baseline data and findings reported from preoperative ophthalmic tests.
Results
Fifty-two eyes (21%) were excluded from appropriate preoperative UWF imaging because of massive lens opacity. The BCVA cutoff point with maximum YI indicating UWF applicability was 0.6 logMAR (YI = 0.3; area under curve [AUC] = 0.7). Among all 246 eyes, preoperative IDO, USG, and UWF showed fair interobserver agreement (all κ > 0.2). According to postoperative IDO findings, the index tests with the highest sensitivity and specificity were USG (100%) and preoperative IDO (99%), respectively.
Conclusions
For cataractous eyes without vision-impairing comorbidities, a BCVA better than 0.6 logMAR (Snellen acuity, 20/80) allows for appropriate nonmydriatic standard UWF imaging. In a high-volume clinic equipped with skilled ophthalmic examiners, screening with USG followed by directed IDO allows the efficient identification of retinal breaks in cataractous eyes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Uhr JH, Obeid A, Wibbelsman TD, Wu CM, Levin HJ, Garrigan H, et al. Delayed retinal breaks and detachments after acute posterior vitreous detachment. Ophthalmology. 2020;127:516–22.
Chen YP, Chen TL, Yang KR, Lee WH, Kuo YH, Chao AN, et al. Treatment of retinal detachment resulting from posterior staphyloma-associated macular hole in highly myopic eyes. Retina. 2006;26:25–31.
Lorenzo-Carrero J, Perez-Flores I, Cid-Galano M, Fernandez-Fernandez M, Heras-Raposo F, Vazquez-Nuñez R, et al. B-scan ultrasonography to screen for retinal tears in acute symptomatic age-related posterior vitreous detachment. Ophthalmology. 2009;116:94–9.
Kumar V, Surve A, Kumawat D, Takkar B, Azad S, Chawla R, et al. Ultra-wide field retinal imaging: a wider clinical perspective. Indian J Ophthalmol. 2021;69:824–35.
Jinabhai AN, Charman WN. Factors affecting image magnification in indirect ophthalmoscopy with Volk or similar lenses and a biomicroscope. Ophthalmic Physiol Opt. 2022;42:717–29.
Peng J, Zhang Q, Jin HY, Lu WY, Zhao PQ. Ultra-wide field imaging system and traditional retinal examinations for screening fundus changes after cataract surgery. Int J Ophthalmol. 2016;9:1299–303.
Nagiel A, Lalane RA, Sadda SR, Schwartz SD. ULTRA-WIDEFIELD FUNDUS IMAGING: a review of clinical applications and future trends. Retina. 2016;36:660–78.
Oh BL, Park UC, Kim BH, Lee EK, Yoon CK, Choe HR, et al. Role of Ultra-widefield Imaging in the evaluation of long-term change of highly myopic fundus. Acta Ophthalmol. 2022;100:e977–e85.
Li M, Yang D, Shen Y, Shang J, Niu L, Yu Y, et al. Application of mydriasis and eye steering in ultrawide field imaging for detecting peripheral retinal lesions in myopic patients. Br J Ophthalmol. 2023;107:1018–24.
Yang SS, Jiang T. Vitrectomy combined with silicone oil tamponade in the treatment of severely traumatized eyes with the visual acuity of no light perception. Int J Ophthalmol. 2013;6:198–203.
Bhambra N, Antaki F, Malt FE, Xu A, Duval R. Deep learning for ultra-widefield imaging: a scoping review. Graefes Arch Clin Exp Ophthalmol. 2022;260:3737–78.
Vaiano AS, Coronado Quitllet E, Zinzanella G, De Benedetti G, Caramello G. Ultrasound measurements of the distance between limbus and retinal break in eyes with media opacities. Retina. 2017;37:1400–6.
Ryan EH. Current treatment strategies for symptomatic vitreous opacities. Curr Opin Ophthalmol. 2021;32:198–202.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012;22:276–82.
Cheng W, Song Y, Gao X, Lin F, Li F, Wang P, et al. Axial length and choriocapillaris flow deficits in non-pathological high myopia. Am J Ophthalmol. 2022;244:68–78.
Radeck V, Schindler F, Helbig H, Gamulescu MA, Cvetkov Y, Barth T, et al. Characteristics of bilateral retinal detachment. Ophthalmologica. 2023;246:99–106.
Agarkar S, Gokhale VV, Raman R, Bhende M, Swaminathan G, Jain M. Incidence, risk factors, and outcomes of retinal detachment after pediatric cataract surgery. Ophthalmology. 2018;125:36–42.
Yang D, Li M, Li W, Wang Y, Niu L, Shen Y, et al. Prediction of refractive error based on ultrawide field images with deep learning models in myopia patients. Front Med. 2022;9:834281.
Kim MJ, Lee JH, Park JI, Choi JY, Sohn J, Hwang HS, et al. Novel utilisation of ultrawide-field fundus photography for detecting retinal nerve fibre layer defects in glaucomatous eyes. Br J Ophthalmol. 2022;106:1524–9.
Li M, Yang D, Shen Y, Shang J, Niu L, Yu Y, et al. Application of mydriasis and eye steering in ultrawide field imaging for detecting peripheral retinal lesions in myopic patients. Br J Ophthalmol. 2023;107:1018–24.
Javitt JC, Tielsch JM, Canner JK, Kolb MM, Sommer A, Steinberg EP. National outcomes of cataract extraction. Increased risk of retinal complications associated with Nd: YAG laser capsulotomy. The Cataract Patient Outcomes Research Team. Ophthalmology. 1992;99:1487–97.
Takkar B, Azad S, Bhatia I, Azad R. Clinical patterns and risk factors for rhegmatogenous retinal detachment at a tertiary eye care centre of northern India. Nepal J Ophthalmol. 2017;9:60–5.
Funding
National Natural Science Foundation of China (NSFC 81300747, NSFC 82101103, and NSFC 82101087), General Program of Shanghai Municipal Natural Science Foundation (Research Project of Science and Technology Commission of Shanghai Municipality (19ZR1408600 and 22ZR1410400)), Young Clinical Scientist Training Program, Shanghai Medical College, Fudan University (2023, DGF828019–2/038), Excellent Young Doctor Training Program of Shanghai, Shanghai Municipal Health Commission (2015–2018).
Author information
Authors and Affiliations
Contributions
AM, YXJ, and TYZ were responsible for designing the protocol, writing the protocol and report, conducting the search, extracting and analyzing data, interpreting results, updating reference lists, and creating “Summary of findings” tables. PML, YXJ, and YL were responsible for designing the protocol, writing the report, extracting, and analyzing the data, and interpreting the results. LLN and KW built the nomogram and contributed to the design of the protocol, writing the report, extracting, and analyzing data, and interpreting results. YMS, JX, and DJQ contributed to data extraction and provided feedback on the report.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miao, A., Xu, J., Wei, K. et al. Comparison of B-Scan ultrasonography, ultra-widefield fundus imaging, and indirect ophthalmoscopy in detecting retinal breaks in cataractous eyes. Eye (2024). https://doi.org/10.1038/s41433-024-03093-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41433-024-03093-2