Abstract
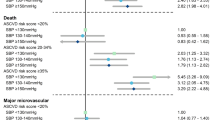
Intensive lipid-lowering therapy is recommended in individuals exhibiting type 2 diabetes mellitus (T2DM) with microvascular complications (as high-risk patients), even without known cardiovascular disease (CVD). However, evidence is insufficient to stratify the patients who would benefit from intensive therapy among them. Hypertension is a major risk factor, and uncontrolled blood pressure (BP) is associated with increased CVD risk. We evaluated the efficacy of intensive vs. standard statin therapy for primary CVD prevention among T2DM patients with retinopathy stratified by BP levels. We used the dataset from the EMPATHY study, which compared intensive statin therapy targeting low-density lipoprotein cholesterol (LDL-C) levels of <70 mg/dL and standard therapy targeting LDL-C levels ranging from ≥100 to <120 mg/dL in T2DM patients with retinopathy without known CVD. A total of 4980 patients were divided into BP ≥ 130/80 mmHg (systolic BP ≥ 130 mmHg and/or diastolic BP ≥ 80 mmHg, n = 3335) and BP < 130/80 mmHg (n = 1645) subgroups by baseline BP levels. During the median follow-up of 36.8 months, 281 CVD events were observed. Consistent with previous studies, CVD events occurred more frequently in the BP ≥ 130/80 mmHg subgroup than in the BP < 130/80 mmHg subgroup (P < 0.001). In the BP ≥ 130/80 mmHg subgroup, intensive statin therapy was associated with lower CVD risk (HR 0.70, P = 0.015) than standard therapy after adjustment. No such association was observed in the BP < 130/80 mmHg subgroup. The interaction between BP subgroup and statin therapy was significant. In conclusion, intensive statin therapy targeting LDL-C < 70 mg/dL provided benefits in primary CVD prevention when compared with standard therapy among T2DM patients with retinopathy and BP ≥ 130/80 mmHg.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary Prevention of Cardiovascular Mortality and Events With Statin Treatments. J Am Coll Cardiol. 2008;52:1769–81.
Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy of cholesterol-lowering therapy in 18 686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371:117–25.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:e177–e232. 2019
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Itoh H, Komuro I, Takeuchi M, Akasaka T, Daida H, Egashira Y, et al. Intensive Treat-to-Target Statin Therapy in High-Risk Japanese Patients With Hypercholesterolemia and Diabetic Retinopathy: report of a randomized study. Diabetes Care. 2018;41:1275–84.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: a report of the American college of cardiology/American Heart Association task. Hypertension. 2018;71:1269–324. 2017
Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, Burnier M, et al. ESC/ESH Guidelines for themanagement of arterial hypertension. Eur Heart J. 2018;39:3021–104. 2018
Imai Y, Hirata T, Saitoh S, Ninomiya T, Miyamoto Y, Ohnishi H, et al. Impact of hypertension stratified by diabetes on the lifetime risk of cardiovascular disease mortality in Japan: a pooled analysis of data from the Evidence for Cardiovascular Prevention from Observational Cohorts in Japan study. Hypertens Res. 2020;43:1437–44.
Newman JD, Schwartzbard AZ, Weintraub HS, Goldberg IJ, Berger JS. Primary Prevention of Cardiovascular Disease in Diabetes Mellitus. J Am Coll Cardiol. 2017;70:883–93.
Brownrigg JRW, Hughes CO, Burleigh D, Karthikesalingam A, Patterson BO, Holt PJ, et al. Microvascular disease and risk of cardiovascular events among individuals with type 2 diabetes: a population-level cohort study. Lancet Diabetes Endocrinol. 2016;4:588–97. https://doi.org/10.1016/S2213-8587(16)30057-2
Selvin E, Marinopoulos S, Berkenblit G, Rami T, Brancati FL, Powe NR, et al. Meta-analysis: Glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141. https://doi.org/10.7326/0003-4819-141-6-200409210-00007
Tadic M, Cuspidi C, Grassi G. Heart rate as a predictor of cardiovascular risk. Eur J Clin Investig. 2018;48:1–11. https://doi.org/10.1111/eci.12892
Kokubo Y. Associations of impaired glucose metabolism and dyslipidemia with cardiovascular diseases: what have we learned from Japanese cohort studies for individualized prevention and treatment? EPMA J. 2011;2:75–81. https://doi.org/10.1007/s13167-011-0074-1
Nishimura K, Okamura T, Watanabe M, Nakai M, Takegami M, Higashiyama A, et al. Predicting coronary heart disease using risk factor categories for a Japanese urban population, and comparison with the Framingham risk score: the Suita study. J Atheroscler Thromb. 2014;21:784–98. https://doi.org/10.5551/jat.19356
Chen G, McAlister FA, Walker RL, Hemmelgarn BR, Campbell NRC. Cardiovascular outcomes in framingham participants with diabetes: the importance of blood pressure. Hypertension. 2011;57:891–7. https://doi.org/10.1161/HYPERTENSIONAHA.110.162446
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA - J Am Med Assoc. 2015;313:603–15. https://doi.org/10.1001/jama.2014.18574
Quarti Trevano F, Seravalle G, Macchiarulo M, Villa P, Valena C, Dell’Oro R, et al. Reliability of heart rate as neuroadrenergic marker in the metabolic syndrome. J Hypertens. 2017;35:1685–90. https://doi.org/10.1097/HJH.0000000000001370
Grassi G, Bombelli M, Brambilla G, Trevano FQ, Dell’oro R, Mancia G. Total cardiovascular risk, blood pressure variability and adrenergic overdrive in hypertension: evidence, mechanisms and clinical implications. Curr Hypertens Rep. 2012;14:333–8. https://doi.org/10.1007/s11906-012-0273-8
Kishi T. Heart failure as an autonomic nervous system dysfunction. J Cardiol. 2012;59:117–22. https://doi.org/10.1016/j.jjcc.2011.12.006
Lewandowski J, Symonides B, Gaciong Z, Siński M. The effect of statins on sympathetic activity: a meta-analysis. Clin Auton Res. 2015;25:125–31. https://doi.org/10.1007/s10286-015-0274-1
Millar PJ, Floras JS. Statins and the autonomic nervous system. Clin Sci. 2014;126:401–15.
Figueiredo VN, Yugar-Toledo JC, Martins LC, Martins LB, De Faria APC, De Haro Moraes C, et al. Vascular stiffness and endothelial dysfunction: correlations at different levels of blood pressure. Blood Press. 2012;21:31–8. https://doi.org/10.3109/08037051.2011.617045
Fujii M, Tomiyama H, Nakano H, Iwasaki Y, Matsumoto C, Shiina K, et al. Differences in longitudinal associations of cardiovascular risk factors with arterial stiffness and pressure wave reflection in middle-aged Japanese men. Hypertens Res. 2021;44:98–106. https://doi.org/10.1038/s41440-020-0523-0
Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. 2018;34:575–84. https://doi.org/10.1016/j.cjca.2017.12.005
Oesterle A, Laufs U, Liao JK. Pleiotropic Effects of Statins on the Cardiovascular System. Circ Res. 2017;120:229–43. https://doi.org/10.1161/CIRCRESAHA.116.308537
Ridker PM. Clinician’s Guide to Reducing Inflammation to Reduce Atherothrombotic Risk: JACC Review Topic of the Week. J Am Coll Cardiol. 2018;72:3320–31. https://doi.org/10.1016/j.jacc.2018.06.082
Mason RP, Walter MF, Jacob RF. Effects of HMG-CoA reductase inhibitors on endothelial function: role of microdomains and oxidative stress. Circulation. 2004;109:II34–41. https://doi.org/10.1161/01.CIR.0000129503.62747.03
Horiuchi M, Cui TX, Li Z, Li JM, Nakagami H, Iwai M. Fluvastatin enhances the inhibitory effects of a selective angiotensin II type 1 receptor blocker, valsartan, on vascular neointimal formation. Circulation. 2003;107:106–12. https://doi.org/10.1161/01.CIR.0000043244.13596.20
Clunn GF, Sever PS, Hughes AD. Calcium channel regulation in vascular smooth muscle cells: synergistic effects of statins and calcium channel blockers. Int J Cardiol. 2010;139:2–6. https://doi.org/10.1016/j.ijcard.2009.05.019
Sever P, Dahlöf B, Poulter N, Wedel H, Beevers G, Caulfield M, et al. Potential synergy between lipid-lowering and blood-pressure-lowering in the Anglo-Scandinavian Cardiac Outcomes Trial. Eur Heart J. 2006;27:2982–8. https://doi.org/10.1093/eurheartj/ehl403
Koh KK, Sakuma I, Shimada K, Hayashi T, Quon MJ. Combining potent statin therapy with other drugs to optimize simultaneous cardiovascular and metabolic benefits while minimizing adverse events. Korean Circ J. 2017;47:432–9. https://doi.org/10.4070/kcj.2016.0406
Sundström J, Gulliksson G, Wirén M. Synergistic effects of blood pressure-lowering drugs and statins: systematic review and meta-Analysis. Evid Based Med. 2018;23:64–9. https://doi.org/10.1136/bmjebm-2017-110888
Hennekens CH, Sacks FM, Tonkin A, Jukema JW, Byington RP, Pitt B, et al. Additive Benefits of Pravastatin and Aspirin to Decrease Risks of Cardiovascular Disease: randomized and Observational Comparisons of Secondary Prevention Trials and Their Meta-analyses. Arch Intern Med. 2004;164:40–4. https://doi.org/10.1001/archinte.164.1.40
Dormuth CR, Hemmelgarn BR, Paterson JM, James MT, Teare GF, Raymond CB, et al. Use of high potency statins and rates of admission for acute kidney injury: multicenter, retrospective observational analysis of administrative databases. BMJ. 2013;346:f880 https://doi.org/10.1136/bmj.f880
Amarenco P, Bogousslavsky J, Callahan A, Gold- LB, Hennerici M, Rudolph AE, et al. High-Dose Atorvastatin after Stroke or Transient Ischemic Attack. N Engl J Med. 2006;355:549–59. https://doi.org/10.1056/NEJMoa061894
Wilson PWF, Polonsky TS, Miedema MD, Khera A, Kosinski AS, Kuvin JT. Systematic Review for the 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:E1144–E1161. https://doi.org/10.1161/CIR.0000000000000626
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KS reports grants from Daiichi Sankyo and Nippon Boehringer Ingelheim. HI reports grants and/or personal fees from Shionogi, Takeda Pharmaceutical, Nippon Boehringer Ingelheim, Daiichi Sankyo, MSD, Mitsubishi Tanabe Pharma, Sumitomo Dainippon Pharma, Astellas Pharma, Kyowa Kirin, Ono Pharmaceutical, Chugai Pharmaceutical, Novartis Pharma, Kao, Mochida Pharmaceutical, Oriental Yeast, Abbott Japan, Bayer Yakuhin, LifeScan Japan, SBI Pharmaceuticals, Nipro, and Wakunaga Pharmaceutical. IK reports grants and/or personal fees from Takeda Pharmaceutical, Nippon Boehringer Ingelheim, Astellas Pharma, Daiichi Sankyo, Otsuka Pharmaceutical, MSD, Mitsubishi Tanabe Pharma, Bristol-Myers Squibb, Ono Pharmaceutical, AstraZeneca, Novartis Pharma, Bayer Yakuhin, Pfizer Japan, Idorsia Pharmaceuticals Japan, and Teijin Pharma. HT reports grants and/or personal fees from Daiichi Sankyo, Novartis Pharma, Otsuka Pharmaceutical, Pfizer Japan, Mitsubishi Tanabe Pharma, Teijin Pharma, Nippon Boehringer Ingelheim, Bayer Yakuhin, Bristol-Myers Squibb, AstraZeneca, Ono Pharmaceutical, Kowa, Japan Tobacco, IQVIA Service Japan, Omron Healthcare, MEDINET, Medical Innovation Kyushu, Abbott Medical Japan, Teijin Home Healthcare, and Boston Scientific Japan. The other authors report no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shinohara, K., Ikeda, S., Enzan, N. et al. Efficacy of intensive lipid-lowering therapy with statins stratified by blood pressure levels in patients with type 2 diabetes mellitus and retinopathy: Insight from the EMPATHY study. Hypertens Res 44, 1606–1616 (2021). https://doi.org/10.1038/s41440-021-00734-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00734-x
Keywords
This article is cited by
-
Update on Hypertension Research in 2021
Hypertension Research (2022)
-
Intensive lipid-lowering therapy in high-risk diabetic patients
Hypertension Research (2021)