Abstract
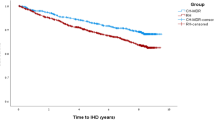
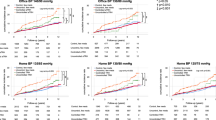
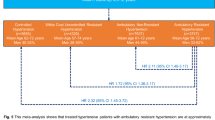
Resistant hypertension (RH) has been poorly studied due to the difficulty in distinguishing it from nonadherence—the exclusion of which is necessary to accurately diagnose RH. Therefore, little is known about the prevalence, predictors, and outcomes of true RH. We evaluated 1838 patients from the standard blood pressure (BP) arm of the Action to Control Cardiovascular Risk in Diabetes Trial. We classified patients into three groups: “true RH”, “pseudo-RH” (i.e., patients with BP levels that would classify them as RH but who were non-adherent), and “other” (i.e., those who could not be classified as having “true RH” or “pseudo-RH”). We examined predictors of true and pseudo-RH and the relationship between true RH and the composite outcome of nonfatal MI, nonfatal stroke, or cardiovascular death. Among 1838 participants with complete information, 489 (26.6%) met the definition of true RH, and 94 (16.1%) RH patients had “pseudo-RH” on ≥1 visit over the first 12 months. Predictors of RH included: baseline SBP ≥ 160 mmHg (OR = 8.79; 95% CI: 5.70–13.68) and baseline SBP between 140–159 (OR = 2.91; 95% CI: 2.13–4.00) compared to SBP < 140, additional baseline BP medication (OR = 3.40; 95% CI: 2.83–4.11), macroalbuminuria (OR = 2.35; 95% CI: 1.50–3.67), CKD (OR = 1.53; 95% CI: 0.99–2.33), history of stroke (OR = 1.73; 95% CI: 1.04–2.82), and black race (OR = 1.39; 95% CI: 1.02–1.88); the cross-validated C-statistic was 0.80. “True RH” patients had a 65% increased hazard in composite outcome (HR = 1.65; 95% CI: 1.13–2.42). In conclusion, the majority of patients classified as having RH had “true RH,” which was more common among those who are black, have macroalbuminuria, CKD, stroke, higher baseline SBP, and are taking more baseline antihypertensives. These patients are at increased risk for cardiovascular and mortality events.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990–2015. JAMA 2017;317:165–82.
Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058.
Yoon SS, Fryar CD, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. Hyattsville, MD, USA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics 2015.
Correction to: 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;72:e33.
Carey RM, Calhoun DA, Bakris GL, Brook RD, Daugherty SL, Dennison-Himmelfarb CR, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American heart association. Hypertension 2018;72:e53–90.
Sarafidis PA, Bakris GL. Resistant hypertension: an overview of evaluation and treatment. J Am Coll Cardiol. 2008;52:1749–57.
Sarafidis PA, Bakris GL. State of Hypertension Management in the United States: Confluence of Risk Factors and the Prevalence of Resistant Hypertension. J Clin Hypertens. 2008;10:130–9. https://doi.org/10.1111/j.1751-7176.2008.07309.x.
Cushman WC, Grimm RH Jr, Cutler JA, Evans GW, Capes S, Corson MA, et al. Rationale and design for the blood pressure intervention of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol. 2007;99:44i–55i.
Cushman WC, Evans GW, Byington RP, Goff Jr DC, Grimm Jr RH, Cutler JA, et al.. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Eng. J. Med. 2010;362:1575–85.
Haley WE, Gilbert ON, Riley RF, Newman JC, Roumie CL, Whittle J, et al. The association between Self-Reported Medication Adherence scores and systolic blood pressure control: a SPRINT baseline data study. J Am Soc Hypertens. 2016;10:857–64.e2.
Kronish IM, Lynch AI, Oparil S, Whittle J, Davis BR, Simpson LM, et al. The Association Between Antihypertensive Medication Nonadherence and Visit-to-Visit Variability of Blood Pressure: Findings From the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Hypertension 2016;68:39–45.
Friedman J, Hastie T, Tibshirani R. Additive logistic regression: a statistical view of boosting (with discussion and a rejoinder by the authors). Ann. Stat. 2000;28:337–407.
Efron B, Gong G. A Leisurely Look at the Bootstrap, the Jackknife, and Cross-Validation [Internet]. Am Statistician. 1983;37:36. https://doi.org/10.2307/2685844.
Daugherty SL, David Powers J, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and Prognosis of Resistant Hypertension in Hypertensive Patients [Internet]. Circulation. 2012;125:1635–42. https://doi.org/10.1161/circulationaha.111.068064.
Sinnott S-J, Smeeth L, Williamson E, Douglas IJ. Trends for prevalence and incidence of resistant hypertension: population based cohort study in the UK 1995-2015. BMJ 2017;358:j3984.
Jung O, Gechter JL, Wunder C, Paulke A, Bartel C, Geiger H, et al. Resistant hypertension? Assessment of adherence by toxicological urine analysis. J Hypertens. 2013;31:766–74.
Irvin MR, Shimbo D, Mann DM, Reynolds K, Krousel-Wood M, Limdi NA, et al. Prevalence and correlates of low medication adherence in apparent treatment-resistant hypertension. J Clin Hypertens. 2012;14:694–700.
Sim JJ, Bhandari SK, Shi J, Liu ILA, Calhoun DA, McGlynn EA, et al. Characteristics of Resistant Hypertension in a Large, Ethnically Diverse Hypertension Population of an Integrated Health System [Internet]. Mayo Clin Proc. 2013;88:1099–107. https://doi.org/10.1016/j.mayocp.2013.06.017.
Acharya T, Tringali S, Singh M, Huang J. Resistant Hypertension and Associated Comorbidities in a Veterans Affairs Population [Internet]. J Clin Hypertension. 2014;16:741–5. https://doi.org/10.1111/jch.12410.
Holecki M, Duława J, Chudek J. Resistant hypertension in visceral obesity [Internet]. Eur J Intern Med. 2012;23:643–8. https://doi.org/10.1016/j.ejim.2012.04.012.
Demede M, Pandey A, Zizi F, Bachmann R, Donat M, McFarlane SI, et al. Resistant Hypertension and Obstructive Sleep Apnea in the Primary-Care Setting. Int J Hypertens. 2011;2011:1–5. https://doi.org/10.4061/2011/340929.
Persell SD. Prevalence of resistant hypertension in the United States, 2003-2008. Hypertension 2011;57:1076–80.
Oliveras A, Armario P, Hernández-del Rey R, Arroyo JA, Poch E, Larrousse M, et al. Urinary albumin excretion is associated with true resistant hypertension [Internet]. J Hum Hypertension. 2010;24:27–33. https://doi.org/10.1038/jhh.2009.35.
Hildrum B, Romild U, Holmen J. Anxiety and depression lowers blood pressure: 22-year follow-up of the population based HUNT study, Norway. BMC Public Health. 2011;11:601.
Licht CMM, de Geus EJC, Seldenrijk A, van Hout HPJ, Zitman FG, van Dyck R, et al. Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension 2009;53:631–8.
Hildrum B, Mykletun A, Holmen J, Dahl AA. Effect of anxiety and depression on blood pressure: 11-year longitudinal population study. Br J Psychiatry. 2008;193:108–13.
Paterniti S, Alperovitch A, Ducimetiere P, Dealberto M-J, Lepine J-P, Bisserbe J-C. Anxiety But Not Depression Is Associated With Elevated Blood Pressure in a Community Group of French Elderly [Internet]. Psychosom Med. 1999;61:77–83. https://doi.org/10.1097/00006842-199901000-00013.
Head GA. Central monoamine neurons and cardiovascular control. Kidney Int Suppl. 1992;37:S8–13.
Stahl SM. Blue genes and the monoamine hypothesis of depression. J Clin Psychiatry. 2000;61:77–8.
Tsioufis C, Kasiakogias A, Kordalis A, Dimitriadis K, Thomopoulos C, Tsiachris D, et al. Dynamic resistant hypertension patterns as predictors of cardiovascular morbidity: a 4-year prospective study. J Hypertens. 2014;32:415–22.
Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens. 2005;18:1422–8.
Salles GF, Cardoso CRL, Muxfeldt ES. Prognostic Influence of Office and Ambulatory Blood Pressures in Resistant Hypertension [Internet]. Arch Intern Med. 2008;168:2340. https://doi.org/10.1001/archinte.168.21.2340.
Muxfeldt ES, Cardoso CRL, Salles GF. Prognostic Value of Nocturnal Blood Pressure Reduction in Resistant Hypertension [Internet]. Arch Intern Med. 2009;169:874. https://doi.org/10.1001/archinternmed.2009.68.
Acknowledgements
Data from the ACCORD trial were supplied by the NHLBI BioLINCC repository. We thank the ACCORD investigators for conducting the clinical trial and granting access to their dataset. This manuscript was not prepared in collaboration with investigators of ACCORD and does not necessarily reflect the opinions of the original study investigators.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chiu, N., Lauffenburger, J.C., Franklin, J.M. et al. Prevalence, predictors, and outcomes of both true- and pseudo-resistant hypertension in the action to control cardiovascular risk in diabetes trial: a cohort study. Hypertens Res 44, 1471–1482 (2021). https://doi.org/10.1038/s41440-021-00739-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-021-00739-6
Keywords
This article is cited by
-
Systematic Review Article: New Drug Strategies for Treating Resistant Hypertension—the Importance of a Mechanistic, Personalized Approach
High Blood Pressure & Cardiovascular Prevention (2024)
-
Role of home blood pressure monitoring in resistant hypertension
Clinical Hypertension (2023)
-
Lifestyle Medicine as a Treatment for Resistant Hypertension
Current Hypertension Reports (2023)