Abstract
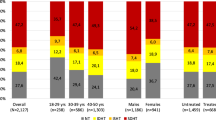
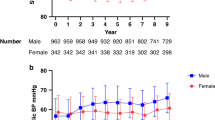
We aimed to evaluate the agreements between the guidelines used for both office blood pressure (OBP) and ambulatory blood pressure monitoring (ABPM). Our secondary aim was to define the best threshold to assess children at risk of left ventricular hypertrophy (LVH). Thresholds proposed by the Fourth Report (FR), European Society of Hypertension (ESH), and American Academy of Pediatrics (AAP) for OBP and the Wühl, ESH, and American Heart Association (AHA) for ABPM were used, and nine different BP phenotype combinations were created. The agreements between the thresholds, the sensitivity of the thresholds, and the BP phenotypes used to predict LVH were determined in 949 patients with different ages and body mass indices (BMIs). The agreements between the guidelines for OBP and ABPM were “good” and “very good” (κ = 0.639; 95% CI, 0.638–0.640, κ = 0.986; 95% CI, 0.985–0.988), respectively. To classify OBP and ABPM into BP phenotypes, we obtained nine different combinations, which had “very good” agreement (κ = 0.880; 95% CI, 0.879–0.880). The sensitivity of AAP for detecting LVH was the highest in <12-year-old obese children (S = 75.8, 95% CI, 56.4–89.7). The sensitivity of ABPM in detecting LVH was similar among different age and BMI groups. The sensitivity of different BP phenotypes tended to be higher in the groups where OBP was evaluated according to AAP. The highest sensitivity was detected in the 13- to 15-year-old normal weight group.(S: 88.8, 95% CI, 51.7–99.7). The AAP guideline is more sensitive and decisive for BP phenotypes to detect LVH, especially in normal-weight children ≤ 15 years, while ABPM thresholds for children have limited effect.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data are available.
References
Guzman-Limon M, Samuels J. Pediatric hypertension: diagnosis, evaluation, and treatment. Pediatr Clin North Am. 2019;66:45–57. https://doi.org/10.1016/j.pcl.2018.09.001. PMID: 30454750.
Awazu M Hypertension. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N (Eds). Pediatric Nephrology, six edition. Berlin Heidelberg, Springer Verlag. 2009;1457–41.
Kjeldsen SE. Hypertension and cardiovascular risk: General aspects. Pharm Res. 2018;129:95–99. https://doi.org/10.1016/j.phrs.2017.11.003. Epub 2017 Nov 7. PMID: 29127059.
Stergiou GS, Nasothimiou E, Giovas P, Kapoyiannis A, Vazeou A. Diagnosis of hypertension in children and adolescents based on home versus ambulatory blood pressure monitoring. J Hypertens. 2008;26:1556–62. https://doi.org/10.1097/HJH.0b013e328301c411. PMID: 18622232.
Flynn JT, Daniels SR, Hayman LL, Maahs DM, McCrindle BW, Mitsnefes M, et al. American Heart Association Atherosclerosis, Hypertension and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young. Update: ambulatory blood pressure monitoring in children and adolescents: a scientific statement from the American Heart Association. Hypertension 2014;63:1116–35. https://doi.org/10.1161/HYP.0000000000000007. Epub 2014 Mar 3. PMID: 24591341; PMCID: PMC4146525.
Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, et al. Office versus Ambulatory Pressure Study Investigators. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N. Engl J Med. 2003;348:2407–15. https://doi.org/10.1056/NEJMoa022273. PMID: 12802026.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555–76. PMID: 15286277.
Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–920. https://doi.org/10.1097/HJH.0000000000001039. PMID: 27467768.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Subcommittee on screening and management of high blood pressure in children. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017;140:e20171904 https://doi.org/10.1542/peds.2017-1904. Epub 2017 Aug 21. Erratum in: Pediatrics. 2017 Nov 30;: Erratum in: Pediatrics. 2018 Sep;142(3): PMID: 28827377.
Wühl E, Witte K, Soergel M, Mehls O, Schaefer F. German Working Group on Pediatric Hypertension. Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens. 2002;20:1995–2007. https://doi.org/10.1097/00004872-200210000-00019. Erratum in: J Hypertens. 2003 Nov; 21(11):2205-6. PMID: 12359978.
Whelton PK, Carey RM, Aronow WS, Casey DE,Jr, Collins KJ, Dennison Himmelfarb C. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS /APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. https://doi.org/10.1161/HYP.0000000000000065. Epub 2017 Nov 13. Erratum in: Hypertension. 2018 Jun;71(6):e140-e144. PMID: 29133356.
Sivén SS, Niiranen TJ, Kantola IM, Jula AM. White-coat and masked hypertension as risk factors for progression to sustained hypertension: the Finn-Home study. J Hypertens. 2016;34:54–60. https://doi.org/10.1097/HJH.0000000000000750. PMID: 26630213.
Lurbe E, Torro I, Alvarez V, Nawrot T, Paya R, Redon J. et al. Prevalence, persistence, and clinical significance of masked hypertension in youth. Hypertension. 2005;45:493–8. https://doi.org/10.1161/01.HYP.0000160320.39303.ab. Epub 2005 Mar 14. PMID: 15767467.
Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R. et al. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: Data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] Study). Circulation. 2001;104:1385–92. https://doi.org/10.1161/hc3701.096100. PMID: 11560854.
Björklund K, Lind L, Zethelius B, Andrén B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297–302. https://doi.org/10.1161/01.cir.0000054622.45012.12
Neyzi O, Bundak R, Gökçay G, Günöz H, Furman A, Darendeliler F, et al. Reference values for weight, height, head circumference, and body mass index in Turkish children. J Clin Res Pediatr Endocrinol. 2015;7:280–93. https://doi.org/10.4274/jcrpe.2183. PMID: 26777039; PMCID: PMC4805217.
Demir K, Konakçı E, Özkaya G, Kasap Demir B, Özen S, Aydın M, et al. New features for child metrics: further growth references and blood pressure calculations. J Clin Res Pediatr Endocrinol 2020;12:125–9. https://doi.org/10.4274/jcrpe.galenos.2019.2019.0127. Epub 2019 Sep 2. PMID: 31475511; PMCID: PMC7291402.
Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anat Valid Method Circ. 1977;55:613–8. https://doi.org/10.1161/01.cir.55.4.613. PMID: 138494.
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR. Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr. 2009;22:709–14. https://doi.org/10.1016/j.echo.2009.03.003. Epub 2009 May 7. PMID: 19423289.
Antolini L, Giussani M, Orlando A, Nava E, Valsecchi MG, Parati G, et al. Nomograms to identify elevated blood pressure values and left ventricular hypertrophy in a paediatric population: American Academy of Pediatrics Clinical Practice vs. Fourth Report/European Society of Hypertension Guidelines. J Hypertens. 2019;37:1213–22. https://doi.org/10.1097/HJH.0000000000002069. PMID: 31022109.
Samuel JP, Bell CS, Hebert SA, Varughese A, Samuels JA, Tyson JE. Office blood pressure measurement alone often misclassifies treatment status in children with primary hypertension. Blood Press Monit. 2017;22:328–32. https://doi.org/10.1097/MBP.0000000000000299. PMID: 29076885; PMCID: PMC5679273.
Hamdani G, Mitsnefes MM, Flynn JT, Becker RC, Daniels S, Falkner BE et al. Pediatric and adult ambulatory blood pressure thresholds and blood pressure load as predictors of left ventricular hypertrophy in adolescents. Hypertension. 2021 May: HYPERTENSIONAHA12016896. https://doi.org/10.1161/HYPERTENSIONAHA.120.16896. Epub ahead of print. PMID: 33966453.
Thomas J, Stonebrook E, Klamer B, Patel HP, Kallash M. Challenges of diagnosing pediatric hypertension using ambulatory blood pressure monitoring. Pediatr Nephrol. 2021;36:373–8. https://doi.org/10.1007/s00467-020-04725-x. Epub 2020 Aug 6. PMID: 32761266.
Lurbe E, Torró I, Álvarez J, Aguilar F, Mancia G, Redon J, et al. Impact of ESH and AAP hypertension guidelines for children and adolescents on office and ambulatory blood pressure-based classifications. J Hypertens. 2019;37:2414–21. https://doi.org/10.1097/HJH.0000000000002229
Sharma A, Altamirano-Diaz L, Grattan M, Filler G, Sharma AP. Comparative analysis of American Heart Association and European Society of Hypertension Ambulatory Blood Pressure Thresholds for Diagnosing Hypertension in Children. Kidney Int Rep. 2020;5:611–7. https://doi.org/10.1016/j.ekir.2020.01.017. PMID: 32405582; PMCID: PMC7210743.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42(Sep):1235–481. https://doi.org/10.1038/s41440-019-0284-9. PMID: 31375757.
Yegül-Gülnar G, Kasap-Demir B, Alparslan C, Çatli G, Mutlubaş F, Yavaşcan Ö, et al. Ambulatory blood pressure monitoring parameters in obese children and adolescents with masked hypertension. Blood Press Monit. 2019;24:277–83. https://doi.org/10.1097/MBP.0000000000000402. PMID: 31567187.
Hashimoto I, Ichida F, Tsubata S, Hamamichi Y, Uese K, Miyazaki A, et al. A novel method for indexing echocardiographic left ventricular mass in infants, children and adolescents: evaluation of obesity-induced left ventricular hypertrophy. Pediatr Int. 1999;41(Apr):126–31. https://doi.org/10.1046/j.1442-200x.1999.4121047.x. PMID: 10221013.
Khoury M, Khoury PR, Dolan LM, Kimball TR, Urbina EM. Clinical implications of the revised AAP Pediatric Hypertension Guidelines. Pediatrics 2018;142(Aug):e20180245 https://doi.org/10.1542/peds.2018-0245. Epub 2018 Jul 5. PMID: 29976572; PMCID: PMC6317543.
Funding
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Contributions
CB conceptualized and designed the study, performed data analysis, and drafted the initial manuscript. BKD reviewed and revised the manuscript; FM, DA, and SAC assisted with the data analysis and critically reviewed the manuscript for important intellectual content; CA, GE and OS assisted with the study design and reviewed and revised the manuscript. FE and MAT reviewed the statistical analysis.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained.
Consent for publication
All authors consent to the publication of this manuscript.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Basaran, C., Kasap Demir, B., Tekindal, M.A. et al. Re-evaluating hypertension in children according to different guidelines: a single-center study. Hypertens Res 45, 1047–1057 (2022). https://doi.org/10.1038/s41440-022-00896-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-00896-2
Keywords
This article is cited by
-
Updates to Pediatric Ambulatory Blood Pressure Monitoring in Clinical Practice: a Review and Strategies for Expanding Access
Current Pediatrics Reports (2022)