Abstract
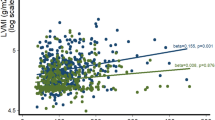
Left ventricular (LV) diastolic dysfunction is associated with heart failure with preserved ejection fraction, and metabolic syndrome (MetS) is a risk factor. However, there is limited knowledge regarding the metabolic factors that contribute to LV dysfunction in postmenopausal women without comorbidities. This study aimed to analyze the relationship between LV diastolic dysfunction and MetS, as well as other cardiovascular risk factors, and to determine risks for LV diastolic dysfunction. Postmenopausal women without hypertension, diabetes mellitus, LV systolic dysfunction, or other heart diseases underwent physical examinations, including echocardiography. The study participants were diagnosed with LV diastolic dysfunction based on several echocardiographic parameters. Logistic regression analyses of LV diastolic dysfunction and cardiovascular risk factors were performed. Of the 269 postmenopausal women examined, 29 (10.7%) and 40 (14.9%) had MetS and LV diastolic dysfunction, respectively. Abnormal diastolic blood pressure (odds ratio, 3.6; 95% confidence interval, 1.16–10.9; P < 0.05) and age (odds ratio, 1.1; 95% confidence interval, 1.07–1.19; P < 0.01) were predictors of LV diastolic dysfunction. In healthy postmenopausal women, high-normal diastolic blood pressure was the only independent risk factor for LV diastolic dysfunction, and it thus may be a useful predictor of diastolic heart failure during routine physical examinations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–9.
Tsuchihashi-Makaya M, Hamaguchi S, Kinugawa S, Yokota T, Goto D, Yokoshiki H, et al. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 2009;73:1893–900.
Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation. 2003;107:714–20.
Shah AM. Ventricular remodeling in heart failure with preserved ejection fraction. Curr Heart Fail Rep. 2013;10:341–9.
Bleumink GS, Knetsch AM, Sturkenboom MC, Straus SM, Hofman A, Deckers JW, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur Heart J. 2004;25:1614–9.
Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol. 1999;33:1948–55.
Zhao Z, Wang H, Jessup JA, Lindsey SH, Chappell MC, Groban L. Role of estrogen in diastolic dysfunction. Am J Physiol Heart Circ Physiol. 2014;306:H628–40.
Goldberg RJ, Spencer FA, Farmer C, Meyer TE, Pezzella S. Incidence and hospital death rates associated with heart failure: a community-wide perspective. Am J Med. 2005;118:728–34.
Kim E, Kwon HY, Baek SH, Lee H, Yoo BS, Kang SM, et al. Medical costs in patients with heart failure after acute heart failure events: one-year follow-up study. J Med Econ. 2018;21:288–93.
Bibbins-Domingo K, Lin F, Vittinghoff E, Barett-Connor E, Hulley SB, Grady D, et al. Predictors of heart failure among women with coronary disease. Circulation. 2004;110:1424–30.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60.
Definition and the diagnostic standard for metabolic syndrome-Committee to evaluate diagnostic standards for metabolic syndrome. Nihon Naika Gakkai Zasshi 2005;94:794–809.
Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62:263–71.
Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19:1550–8.
Goto T, Ohte N, Fukuta H, Wakami K, Tani T, Kimura G. Relationship between effective arterial elastance, total vascular resistance, and augmentation index at the ascending aorta and left ventricular diastolic function in older women. Circ J. 2013;77:123–9.
SPRINT Research Group, Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A Randomized trial of intensive versus standard blood-pressure control. N. Engl J Med. 2015;373:2103–16.
Son MK, Lim NK, Lim JY, Cho J, Chang Y, Ryu S, et al. Difference in blood pressure between early and late menopausal transition was significant in healthy Korean women. BMC Women’s Health. 2015;15:64.
Libhaber CD, Woodiwiss AJ, Booysen HL, Maseko MJ, Majane OH, Sareli P, et al. Differential relationships of systolic and diastolic blood pressure with components of left ventricular diastolic dysfunction. J Hypertens. 2014;32:4.
Nethononda RM, Lewandowski AJ, Stewart R, Kylinterias I, Whitworth P, Francis P, et al. Gender specific patterns of age-related decline in aortic stiffness: a cardiovascular magnetic resonance study including normal ranges. J Cardiovasc Magn Reson. 2015;17:20.
(NCD-RisC) NRFC. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389:37.
Stanley SF, Martin GL, Shehzad AK, Nathan DW, Eric PL, William BK, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;6:103.
Acknowledgements
We thank Nature Research Editing Service for English language editing and publication support.
Author information
Authors and Affiliations
Contributions
Conceptualization: KS and MK; writing—original draft preparation: MK and NH; writing—review and editing: MK, TY, NH, and JY. All authors have read and agreed to the version of the manuscript to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
The study was conducted in accordance withthe Declaration of Helsinki and approved by the Human Research Protection Office ofTokyo Women’s Medical University (protocol code #2507, approved June 25, 2012).
Informed consent
Informed consent was obtained from all individuals involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kimura, M., Sekiguchi, H., Shimamoto, K. et al. High-normal diastolic blood pressure as a risk factor for left ventricular diastolic dysfunction in healthy postmenopausal women. Hypertens Res 45, 1891–1898 (2022). https://doi.org/10.1038/s41440-022-01024-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01024-w
Keywords
This article is cited by
-
Is diastolic blood pressure key to detecting risk and preventing heart failure with preserved ejection fraction?
Hypertension Research (2023)
-
Uncontrolled hypertension: the greatest challenge and perspectives in Asia
Hypertension Research (2022)