Abstract
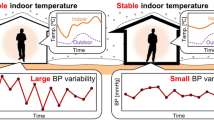
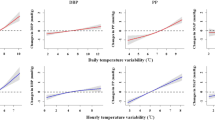
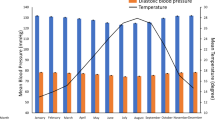
Ambient temperature and blood pressure (BP) are closely related; however, few studies have examined the association of out-of-office BP with indoor or outdoor temperature. The effect of the difference between indoor and outdoor temperatures on BP also remains unknown. Therefore, this study aimed to investigate the association of indoor and outdoor temperatures and their difference with home BP. We studied healthy 352 participants (mean age, 49.8 years; 46.0% women) from a population-based cohort using 2-year data on temperature and self-measured home BP. We measured home BP and indoor temperature at the same time in the morning and evening every day. Outdoor temperature during the same period was based on national data. We observed 82,900 home BP measurements in the morning and 66,420 in the evening. In the mixed-effects model adjusted for age, sex, and possible confounders, indoor temperature was inversely associated with systolic and diastolic BP in the morning and evening. A 1 °C increase in indoor temperature reduced systolic and diastolic BP by 0.37 and 0.22 mmHg, respectively, in the morning and by 0.45 and 0.30 mmHg, respectively, in the evening (all P-values<0.001). The magnitude of associations was stronger for indoor than outdoor temperature. Similarly, a 1 °C increase in indoor temperature above outdoor temperature decreased systolic and diastolic BP by 0.33 and 0.12 mmHg, respectively, in the morning and by 0.45 and 0.26 mmHg, respectively, in the evening independent of outdoor temperature (all P-values <0.001). In conclusion, controlling indoor temperature is important to stabilize home BP levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: A population-based observation in ohasama, japan. J Hypertens. 1998;16:971–5.
Niiranen TJ, Hanninen MR, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn-Home study. Hypertension 2010;55:1346–51.
Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: Systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30:449–56.
Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate E Loro Associazioni. J Hypertens. 1998;16:1585–92.
Rose G. Seasonal variation in blood pressure in man. Nature. 1961;189:235.
Woodhouse PR, Khaw KT, Plummer M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. 1993;11:1267–74.
Saeki K, Obayashi K, Iwamoto J, Tone N, Okamoto N, Tomioka K, et al. Stronger association of indoor temperature than outdoor temperature with blood pressure in colder months. J Hypertens. 2014;32:1582–9.
Kubozono T, Akasaki Y, Kawasoe S, Ojima S, Kawabata T, Makizako H, et al. The relationship between home blood pressure measurement and room temperature in a japanese general population. Hypertens Res. 2021;44:454–63.
Hisamatsu T, Taniguchi K, Fukuda M, Kinuta M, Nakahata N, Kanda H. Effect of Coronavirus Disease 2019 Pandemic on Physical Activity in a Rural Area of Japan: The Masuda Study. J Epidemiol. 2021;31:237–8.
Kuwabara M, Harada K, Hishiki Y, Kario K. Validation of an automatic device for the self-measurement of blood pressure in sitting and supine positions according to the ANSI/AAMI/ISO81060-2: 2013 guidelines: the Omron HEM-9700T. Blood Press Monit. 2019;24:146–50.
Iwahori T, Miura K, Obayashi K, Ohkubo T, Nakajima H, Shiga T, et al. Seasonal variation in home blood pressure: findings from nationwide web-based monitoring in Japan. BMJ Open. 2018;8:e017351. https://doi.org/10.1136/bmjopen-2017-017351.
Hisamatsu T, Lloyd-Jones DM, Colangelo LA, Liu K. Urinary sodium and potassium excretions in young adulthood and blood pressure by middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. J Hypertens. 2021;39:1586–93.
Umishio W, Ikaga T, Kario K, Fujino Y, Hoshi T, Ando S, et al. Cross-Sectional Analysis of the Relationship Between Home Blood Pressure and Indoor Temperature in Winter: A Nationwide Smart Wellness Housing Survey in Japan. Hypertension. 2019;74:756–66.
Huang CC, Chen YH, Hung CS, Lee JK, Hsu TP, Wu HW, et al. Assessment of the Relationship Between Ambient Temperature and Home Blood Pressure in Patients From a Web-Based Synchronous Telehealth Care Program: Retrospective Study. J Med Internet Res. 2019;21:e12369. https://doi.org/10.2196/12369.
Chen Q, Wang J, Tian J, Tang X, Yu C, Marshall RJ, et al. Association between ambient temperature and blood pressure and blood pressure regulators: 1831 hypertensive patients followed up for three years. PLoS One. 2013;8:e84522. https://doi.org/10.1371/journal.pone.0084522.
Rose GA. The strategy of preventive medicine. Oxford University Press; 1992.
Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, et al. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288:1882–8.
Public health england. Minimum home temperature thresholds for health in winter; A systematic literature review. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/776497/Min_temp_threshold_for_homes_in_winter.pdf. Accessed 1 August 2022.
World health organization. Housing and health guidelines. http://apps.who.int/iris/bitstream/handle/10665/276001/9789241550376-eng.pdf. Accessed 1 August 2022.
Yang L, Li L, Lewington S, Guo Y, Sherliker P, Bian Z, et al. Outdoor temperature, blood pressure, and cardiovascular disease mortality among 23 000 individuals with diagnosed cardiovascular diseases from china. Eur Heart J. 2015;36:1178–85.
Analitis A, Katsouyanni K, Biggeri A, Baccini M, Forsberg B, Bisanti L, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol. 2008;168:1397–408.
van Rossum CT, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG. Seasonal variation in cause-specific mortality: are there high-risk groups? 25-year follow-up of civil servants from the first Whitehall study. Int J Epidemiol. 2001;30:1109–16.
Yu B, Jin S, Wang C, Yan S, Zhou X, Cui X, et al. The association of outdoor temperature with blood pressure, and its influence on future cardio-cerebrovascular disease risk in cold areas. J Hypertens. 2020;38:1080–9.
Acknowledgements
We thank the Masuda Healthcare Association, Masuda City, Masuda Medical Association, and the study participants for their commitment and outstanding dedication. We are also grateful to Dr. Yuji Matsumoto, the chairman of the Masuda Medical Association, who greatly contributed to the study. Finally, we thank Angela Morben, DVM, ELS, from Edanz (https://jp.edanz.com/ac), for editing a draft of this manuscript.
Funding
This work was supported by a Grant-in-Aid for Scientific Research (C) [grant number 20K10529] from the Japan Society for the Promotion of Science and a grant from OMRON Healthcare Co., Ltd. The funding sponsors had no role in the study design or conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation of the article; or the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T.H., N.N., and H.K. received a research grant from OMRON Healthcare Co., Ltd. The other authors declare no conflicts of interest in association with the present study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kinuta, M., Hisamatsu, T., Fukuda, M. et al. Associations of indoor and outdoor temperatures and their difference with home blood pressure: The Masuda Study. Hypertens Res 46, 200–207 (2023). https://doi.org/10.1038/s41440-022-01059-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-022-01059-z
Keywords
This article is cited by
-
2023 update and perspectives
Hypertension Research (2024)
-
The impact of short-term exposure to meteorological factors on the risk of death from hypertension and its major complications: a time series analysis based on Hefei, China
International Archives of Occupational and Environmental Health (2024)
-
Management of seasonal variation in blood pressure through the optimal adjustment of antihypertensive medications and indoor temperature
Hypertension Research (2023)