Abstract
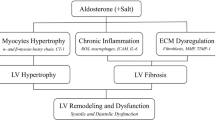
Primary aldosteronism is the most frequent secondary hypertensive disease and is characterized by an elevated risk for cardiovascular disease. The current standard treatments are adrenalectomy and/or administration of mineralocorticoid receptor blockers, both of which are effective at ameliorating hypertension via intervention for hyperaldosteronism. However, both of these approaches have side effects and contraindications, and mineralocorticoid receptor blockers also have limited preventive efficacy against cardiovascular events. Recently, in vitro experiments have shown that aldosterone regulation is closely related to abdominal fat accumulation and that there is crosstalk between aldosterone and visceral fat tissue accumulation. We previously reported that this interaction was clinically significant in renal dysfunction; however, its effects on the heart remain unclear. Here, we analyzed data from 49 patients with primary aldosteronism and 29 patients with essential hypertension to examine the potential effect of the interaction between the ratio of visceral-to-subcutaneous fat tissue volume and the plasma aldosterone concentration on echocardiographic indices, including the tissue Doppler-derived E/e’ ratio. A significant interaction was found in patients with primary aldosteronism (p < 0.05), indicating that patients with the combination of a high plasma aldosterone concentration and high visceral-to-subcutaneous fat ratio show an increased E/e’ ratio, which is a well-known risk factor for future cardiovascular events. Our results confirm the clinical importance of the interaction between aldosterone and abdominal fat tissue, suggesting that an improvement in the visceral-to-subcutaneous fat ratio may be synergistically and complementarily effective in reducing the elevated risk of cardiovascular disease in patients with primary aldosteronism when combined with conventional therapies for reducing aldosterone activity.

A significant effect of the interaction between plasma aldosterone concentration and the visceral-to-subcutaneous fat ratio on the tissue Doppler-derived E/e' ratio in patients with primary aldosteronism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Conn JW, Knopf RF, Nesbit RM. Clinical characteristics of primary aldosteronism from an analysis of 145 cases. Am J Surg. 1964;107:159–72.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism -The Japan Endocrine Society 2009. Endocr J. 2011;advpub:1108040599-1108040599.
Naruse M, Katabami T, Shibata H, Sone M, Takahashi K, Tanabe A, et al. Japan Endocrine society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr J. 2022;69:327–59.
Rossi GP, Bello VD, Ganzaroli C, Sacchetto A, Cesari M, Bertini A, et al. Excess idosterone is associated with alterations of myocardial texture in primary aldosteronism. Hypertension. 2002;40:23–7.
Neves MF, Cunha AR, Cunha MR, Gismondi RA, Oigman W. The role of renin-angiotensin-aldosterone system and its new components in arterial stiffness and vascular aging. High Blood Press Cardiovasc Prev. 2018;25:137–45.
Wu X, Yu J, Tian H. Cardiovascular risk in primary aldosteronism: A systematic review and meta-analysis. Med (Baltim). 2019;98:e15985.
Chang Y-Y, Liao C-W, Tsai C-H, Chen C-W, Pan C-T, Chen Z-W, et al. Left ventricular dysfunction in patients with primary aldosteronism: a propensity score-matching follow-up study with tissue doppler imaging. J Am Heart Assoc. 2019;8:e013263–e013263.
Chen Y-L, Xu T-Y, Xu J-Z, Zhu L-M, Li Y, Wang J-G. A non-invasive left ventricular pressure-strain loop study on myocardial work in primary aldosteronism. Hypertens Res. 2021;44:1462–70-1462.
Chen Y-L, Xu T-Y, Xu J-Z, Zhu L-M, Li Y, Wang J-G. A prospective comparative study on cardiac alterations after surgery and drug treatment of primary aldosteronism. Front Endocrinol (Lausanne). 2021;12:770711–770711.
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6:51–9.
Briet M, Schiffrin EL. The role of aldosterone in the metabolic syndrome. Curr Hypertens Rep. 2011;13:163–72.
Ingelsson E, Pencina MJ, Tofler GH, Benjamin EJ, Lanier KJ, Jacques PF, et al. Multimarker approach to evaluate the incidence of the metabolic syndrome and longitudinal changes in metabolic risk factors: the framingham offspring study. Circulation. 2007;116:984–92.
Hanslik G, Wallaschofski H, Dietz A, Riester A, Reincke M, Allolio B, et al. Increased prevalence of diabetes mellitus and the metabolic syndrome in patients with primary aldosteronism of the German Conn’s Registry. Eur J Endocrinol. 2015;173:665–75.
Shibayama Y, Wada N, Baba S, Miyano Y, Obara S, Iwasaki R, et al. Relationship between visceral fat and plasma aldosterone concentration in patients with primary aldosteronism. J Endocr Soc. 2018;2:1236–45.
Werner N, Nickenig G. From fat fighter to risk factor: the zigzag trek of leptin. Arterioscler Thromb Vasc Biol. 2004;24:7–9.
Iwashima Y, Katsuya T, Ishikawa K, Ouchi N, Ohishi M, Sugimoto K, et al. Hypoadiponectinemia is an independent risk factor for hypertension. Hypertension. 2004;43:1318–23.
Tan KC, Xu A, Chow WS, Lam MC, Ai VH, Tam SC, et al. Hypoadiponectinemia is associated with impaired endothelium-dependent vasodilation. J Clin Endocrinol Metab. 2004;89:765–9.
Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S. Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes. 2007;56:1010–3.
Lemieux I, Pascot A, Prud’homme D, Almeras N, Bogaty P, Nadeau A, et al. Elevated C-reactive protein: another component of the atherothrombotic profile of abdominal obesity. Arterioscler Thromb Vasc Biol. 2001;21:961–7.
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–808.
Fain JN, Madan AK, Hiler ML, Cheema P, Bahouth SW. Comparison of the release of adipokines by adipose tissue, adipose tissue matrix, and adipocytes from visceral and subcutaneous abdominal adipose tissues of obese humans. Endocrinology. 2004;145:2273–82.
Kataoka H, Mochizuki T, Iwadoh K, Ushio Y, Kawachi K, Watanabe S, et al. Visceral to subcutaneous fat ratio as an indicator of a >/=30% eGFR decline in chronic kidney disease. PLoS One. 2020;15:e0241626.
Silveira EA, Kliemann N, Noll M, Sarrafzadegan N, de Oliveira C. Visceral obesity and incident cancer and cardiovascular disease: An integrative review of the epidemiological evidence. Obes Rev. 2021;22:e13088.
Lind L, Michaelsson K, Söderberg S, Larsson A, Johansson L, Kullberg J, et al. On the association between body fat and left ventricular mass. J Hypertens. 2019;37:1699–704.
Di Chiara T, Licata A, Argano C, Duro G, Corrao S, Scaglione R. Plasma adiponectin: a contributing factor for cardiac changes in visceral obesity-associated hypertension. Blood Press. 2014;23:147–53.
Ehrhart-Bornstein M, Lamounier-Zepter V, Schraven A, Langenbach J, Willenberg HS, Barthel A, et al. Human adipocytes secrete mineralocorticoid-releasing factors. Proc Natl Acad Sci USA. 2003;100:14211–6.
Huby AC, Antonova G, Groenendyk J, Gomez-Sanchez CE, Bollag WB, Filosa JA, et al. Adipocyte-derived hormone leptin is a direct regulator of aldosterone secretion, which promotes endothelial dysfunction and cardiac fibrosis. Circulation. 2015;132:2134–45.
Guo C, Ricchiuti V, Lian BQ, Yao TM, Coutinho P, Romero JR, et al. Mineralocorticoid receptor blockade reverses obesity-related changes in expression of adiponectin, peroxisome proliferator-activated receptor-gamma, and proinflammatory adipokines. Circulation. 2008;117:2253–61.
Kraus D, Jager J, Meier B, Fasshauer M, Klein J. Aldosterone inhibits uncoupling protein-1, induces insulin resistance, and stimulates proinflammatory adipokines in adipocytes. Horm Metab Res. 2005;37:455–9.
Jia G, Aroor AR, Sowers JR. The role of mineralocorticoid receptor signaling in the cross-talk between adipose tissue and the vascular wall. Cardiovasc Res. 2017;113:1055–63.
Haze T, Hatakeyama M, Komiya S, Kawano R, Ohki Y, Suzuki S, et al. Association of the ratio of visceral-to-subcutaneous fat volume with renal function among patients with primary aldosteronism. Hypertens Res. 2021;44:1341–51.
Nishikawa T, Omura M, Satoh F, Shibata H, Takahashi K, Tamura N, et al. Guidelines for the diagnosis and treatment of primary aldosteronism-the Japan Endocrine Society 2009. Endocr J. 2011;58:711–21.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, Developed in Conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–71.
Fuchs A, Kühl JT, Sigvardsen PE, Knudsen AD, Nilsson EJP, Stisen ZR, et al. Arterial hypertension and morphologic abnormalities of cardiac chambers: results from the Copenhagen General Population Study. J Hypertens. 2021;39:703–10.
Galderisi M, Cosyns B, Edvardsen T, Cardim N, Delgado V, Di Salvo G, et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017;18:1301–10.
Schussheim AE, Devereux RB, de Simone G, Borer JS, Herrold EM, Laragh JH. Usefulness of subnormal midwall fractional shortening in predicting left ventricular exercise dysfunction in asymptomatic patients with systemic hypertension. Am J Card. 1997;79:1070–4.
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314.
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function-a study in normals and dilated cardiomyopathy. J Cardiol. 1995;26:357–66.
Yasuoka K, Harada K, Toyono M, Tamura M, Yamamoto F. Tei index determined by tissue doppler imaging in patients with pulmonary regurgitation after repair of tetralogy of fallot. Pediatr Cardiol. 2004;25:131–6.
Mansour H, Nassar AI, Abdel Rehim WA, Roushdy AM, Abobakr M, Zaki HM, et al. Can Tei index predict high syntax score in patients with chronic coronary syndrome and normal left ventricular systolic function? J Cardiovasc Echogr. 2021;31:11–6.
Rossi GP, Auchus RJ, Brown M, Lenders JWM, Naruse M, Plouin PF, et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension. 2014;63:151–60.
Kempers MJE, Lenders JWM, van Outheusden L, van der Wilt GJ, Schultze Kool LJ, Hermus ARMM, et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009;151:329–37.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Parra Ramírez P, Rojas-Marcos PM, Paja Fano M, González Boillos M, Pascual-Corrales E, García-Cano A, et al. Differences in the presentation and evolution of primary aldosteronism in elderly (≥65 years) and young patients (<65 years). Endocr Connect. 2022;11:e220169.
Haze T, Hirawa N, Yano Y, Tamura K, Kurihara I, Kobayashi H, et al. Association of aldosterone and blood pressure with the risk for cardiovascular events after treatments in primary aldosteronism. Atherosclerosis 2021;324:84–90.
Haze T, Yano Y, Hatano Y, Tamura K, Kurihara I, Kobayashi H, et al. Association of achieved blood pressure after treatment for primary aldosteronism with long-term kidney function. J Hum Hypertens. 2021.).
Sharp ASP, Tapp RJ, Thom SAM, Francis DP, Hughes AD, Stanton AV, et al. Tissue Doppler E/E′ ratio is a powerful predictor of primary cardiac events in a hypertensive population: an ASCOT substudy. Eur Heart J. 2009;31:747–52.
Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature 2006;444:881–7.
D’Marco L, Puchades MJ, Gorriz JL, Romero-Parra M, Lima-Martinez M, Soto C, et al. Epicardial adipose tissue, adiponectin and leptin: a potential source of cardiovascular risk in chronic kidney disease. Int J Mol Sci. 2020;21:978.
Otero M, Lago R, Lago F, Casanueva FF, Dieguez C, Gómez-Reino JJ, et al. Leptin, from fat to inflammation: old questions and new insights. FEBS Lett. 2005;579:295–301.
Poetsch MS, Strano A, Guan K. Role of leptin in cardiovascular diseases. Front Endocrinol (Lausanne). 2020;11:354.
Gutiérrez-Tenorio J, Marín-Royo G, Martínez-Martínez E, Martín R, Miana M, López-Andrés N, et al. The role of oxidative stress in the crosstalk between leptin and mineralocorticoid receptor in the cardiac fibrosis associated with obesity. Sci Rep. 2017;7:16802.
Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun. 1999;257:79–83.
Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R. Visceral fat is an independent predictor of all-cause mortality in men. Obes (Silver Spring). 2006;14:336–41.
Fontes-Carvalho R, Fontes-Oliveira M, Sampaio F, Mancio J, Bettencourt N, Teixeira M, et al. Influence of epicardial and visceral fat on left ventricular diastolic and systolic functions in patients after myocardial infarction. Am J Cardiol. 2014;114:1663–9.
Capoulade R, Larose E, Mathieu P, Clavel M-A, Dahou A, Arsenault M, et al. Visceral adiposity and left ventricular mass and function in patients with aortic stenosis: the PROGRESSA study. Can J Cardiol. 2014;30:1080–7.
Caprio M, Antelmi A, Chetrite G, Muscat A, Mammi C, Marzolla V, et al. Antiadipogenic effects of the mineralocorticoid receptor antagonist drospirenone: potential implications for the treatment of metabolic syndrome. Endocrinology. 2011;152:113–25.
Rocchini AP, Moorehead C, DeRemer S, Goodfriend TL, Ball DL. Hyperinsulinemia and the aldosterone and pressor responses to angiotensin II. Hypertension. 1990;15:861–6.
Petrasek D, Jensen G, Tuck M, Stern N. In vitro effects of insulin on aldosterone production in rat zona glomerulosa cells. Life Sci. 1992;50:1781–7.
Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010;11:11–8.
Ghantous CM, Azrak Z, Hanache S, Abou-Kheir W, Zeidan A. Differential role of leptin and adiponectin in cardiovascular system. Int J Endocrinol. 2015;2015:534320.
Cuspidi C, Tadic M, Sala C, Quarti-Trevano F, Gherbesi E, Mancia G, et al. Regression of left ventricular hypertrophy in primary aldosteronism after adrenalectomy: a meta-analysis of echocardiographic studies. J Hypertens. 2021;39:775–83.
Riggs K, Ali H, Taegtmeyer H, Gutierrez AD. The use of SGLT-2 inhibitors in type 2 diabetes and heart failure. Metab Syndr Relat Disord. 2015;13:292–7.
Itcho K, Oki K, Ohno H, Yoneda M. Update on genetics of primary aldosteronism. Biomedicines 2021;9:409.
Omata K, Satoh F, Morimoto R, Ito S, Yamazaki Y, Nakamura Y, et al. Cellular and genetic causes of idiopathic hyperaldosteronism. Hypertension 2018;72:874–80.
Käyser SC, Dekkers T, Groenewoud HJ, van der Wilt GJ, Carel Bakx J, van der Wel MC, et al. Study heterogeneity and estimation of prevalence of primary aldosteronism: a systematic review and meta-regression analysis. J Clin Endocrinol Metab. 2016;101:2826–35.
Ranasinghe P, Mathangasinghe Y, Jayawardena R, Hills AP, Misra A. Prevalence and trends of metabolic syndrome among adults in the asia-pacific region: a systematic review. BMC Public Health. 2017;17:101.
Alberti KGMM, Zimmet P, Shaw J. Metabolic syndrome—a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80.
Acknowledgements
This study was supported by a basic research grant from Yokohama City University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haze, T., Ozawa, M., Kawano, R. et al. Effect of the interaction between the visceral-to-subcutaneous fat ratio and aldosterone on cardiac function in patients with primary aldosteronism. Hypertens Res 46, 1132–1144 (2023). https://doi.org/10.1038/s41440-023-01170-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01170-9
Keywords
This article is cited by
-
Possible relationship between primary aldosteronism and small vessel disease
Hypertension Research (2024)
-
Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism
Hypertension Research (2024)
-
Recent progress in unraveling cardiovascular complications associated with primary aldosteronism: a succinct review
Hypertension Research (2024)
-
Esaxerenone for nocturnal hypertension and possible future direction for treatment of hypertension-cardiovascular-kidney comorbidity
Hypertension Research (2023)
-
Visceral fat: a bad companion for mineralocorticoid receptor overactivation
Hypertension Research (2023)