Abstract
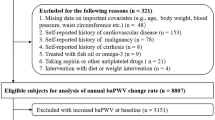
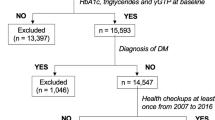
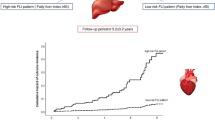
Metabolic dysfunction-associated fatty liver disease (MAFLD), a new feature of fatty liver (FL) disease that is defined as FL with overweight/obesity, type 2 diabetes mellitus or metabolic dysregulation, has been reported to be associated with the development of diabetes mellitus, chronic kidney disease and cardiovascular disease. However, the association between MAFLD and hypertension remains unclear. We investigated the association between MAFLD and systolic blood pressure (SBP) over a 10-year period in 28,990 Japanese subjects who received annual health examinations. After exclusion of subjects without data for SBP and abdominal ultrasonography at baseline, a total of 17,021 subjects (men/women: 10,973/6048; mean age: 49 years) were recruited. Linear mixed-effects model analyses using diagnoses of FL, nonalcoholic fatty liver disease (NAFLD) or MAFLD and age, sex, SBP, use of anti-hypertensive drugs, levels of uric acid and estimated glomerular filtration rate, family history of hypertension and habits of current smoking and alcohol drinking at baseline as well as the duration of the observation period and the interaction between each covariate and the duration of the observation period showed that the significant association of change in SBP over time with diagnosis of MAFLD (estimate: 0.223 mmHg/year, P < 0.001) was greater than that with diagnoses of FL (estimate: 0.196 mmHg/year, P < 0.001) and NAFLD (estimate: 0.203 mmHg/year, P < 0.001). Furthermore, the rate of increase in SBP over time was higher in subjects with MAFLD than in subjects without FL and subjects with FL who had no MAFLD. In conclusion, MAFLD is significantly associated with an increase in SBP over time.

The presence of metabolic dysfunction-associated fatty liver disease (MAFLD) is significantly associated with an increase in systolic blood pressure over time.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15:11–20.
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA 2015;313:2263–73.
Brunt EM, Wong VW, Nobili V, Day CP, Sookoian S, Maher JJ, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Prim. 2015;1:15080.
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–57.
Ryoo JH, Suh YJ, Shin HC, Cho YK, Choi JM, Park SK. Clinical association between non-alcoholic fatty liver disease and the development of hypertension. J Gastroenterol Hepatol. 2014;29:1926–31.
Zhao YC, Zhao GJ, Chen Z, She ZG, Cai J, Li H. Nonalcoholic Fatty Liver Disease: An Emerging Driver of Hypertension. Hypertension. 2020;75:275–84.
Li G, Peng Y, Chen Z, Li H, Liu D, Ye X. Bidirectional Association between Hypertension and NAFLD: A Systematic Review and Meta-Analysis of Observational Studies. Int J Endocrinol. 2022;2022:8463640.
Ciardullo S, Grassi G, Mancia G, Perseghin G. Nonalcoholic fatty liver disease and risk of incident hypertension: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2022;34:365–71.
Targher G, Corey KE, Byrne CD, Roden M. The complex link between NAFLD and type 2 diabetes mellitus - mechanisms and treatments. Nat Rev Gastroenterol Hepatol. 2021;18:599–612.
Targher G, Byrne CD. Non-alcoholic fatty liver disease: an emerging driving force in chronic kidney disease. Nat Rev Nephrol. 2017;13:297–310.
Stahl EP, Dhindsa DS, Lee SK, Sandesara PB, Chalasani NP, Sperling LS. Nonalcoholic Fatty Liver Disease and the Heart: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73:948–63.
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33.
Takahashi S, Tanaka M, Higashiura Y, Mori K, Hanawa N, Ohnishi H, et al. Prediction and validation of nonalcoholic fatty liver disease by fatty liver index in a Japanese population. Endocr J. 2022;69:463–71.
Higashiura Y, Furuhashi M, Tanaka M, Takahashi S, Mori K, Miyamori D, et al. Elevated Fatty Liver Index Is Independently Associated With New Onset of Hypertension During a 10-Year Period in Both Male and Female Subjects. J Am Heart Assoc. 2021;10:e021430.
Higashiura Y, Furuhashi M, Tanaka M, Takahashi S, Koyama M, Ohnishi H, et al. High level of fatty liver index predicts new onset of diabetes mellitus during a 10-year period in healthy subjects. Sci Rep. 2021;11:12830.
Takahashi S, Tanaka M, Furuhashi M, Moniwa N, Koyama M, Higashiura Y, et al. Fatty liver index is independently associated with deterioration of renal function during a 10-year period in healthy subjects. Sci Rep. 2021;11:8606.
Mori K, Tanaka M, Higashiura Y, Hanawa N, Ohnishi H, Furuhashi M. High fatty liver index is an independent predictor of ischemic heart disease during a 10-year period in a Japanese population. Hepatol Res. 2022 (e-pub ahead of print 2022/05/17;https://doi.org/10.1111/hepr.13790).
Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202–9.
Eslam M, Alkhouri N, Vajro P, Baumann U, Weiss R, Socha P, et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol Hepatol. 2021;6:864–73.
Mendez-Sanchez N, Bugianesi E, Gish RG, Lammert F, Tilg H, Nguyen MH, et al. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol Hepatol. 2022;7:388–90.
Tanaka M, Mori K, Takahashi S, Higashiura Y, Ohnishi H, Hanawa N, et al. Metabolic dysfunction-associated fatty liver disease predicts new onset of chronic kidney disease better than does fatty liver or nonalcoholic fatty liver disease. Nephrol Dial Transplant. 2022 (e-pub ahead of print 2022/05/26;https://doi.org/10.1093/ndt/gfac188).
Chen YL, Li H, Li S, Xu Z, Tian S, Wu J, et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: a cross-sectional comparative study. BMC Gastroenterol. 2021;21:212.
Wong RJ, Cheung R. Trends in the Prevalence of Metabolic Dysfunction-Associated Fatty Liver Disease in the United States, 2011-2018. Clin Gastroenterol Hepatol. 2022;20:e610–e3.
Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40:2082–9.
Miyake T, Matsuura B, Furukawa S, Ishihara T, Yoshida O, Miyazaki M, et al. Fatty liver with metabolic disorder, such as metabolic dysfunction-associated fatty liver disease, indicates high risk for developing diabetes mellitus. J Diabetes Investig. 2022(e-pub ahead of print 2022/02/16;https://doi.org/10.1111/jdi.13772).
Liang Y, Chen H, Liu Y, Hou X, Wei L, Bao Y, et al. Association of MAFLD With Diabetes, Chronic Kidney Disease, and Cardiovascular Disease: A 4.6-Year Cohort Study in China. J Clin Endocrinol Metab. 2022;107:88–97.
Wang TY, Wang RF, Bu ZY, Targher G, Byrne CD, Sun DQ, et al. Association of metabolic dysfunction-associated fatty liver disease with kidney disease. Nat Rev Nephrol. 2022;18:259–68.
Tsutsumi T, Eslam M, Kawaguchi T, Yamamura S, Kawaguchi A, Nakano D, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: Generalized estimating equation approach. Hepatol Res. 2021;51:1115–28.
Lee H, Lee YH, Kim SU, Kim HC. Metabolic Dysfunction-Associated Fatty Liver Disease and Incident Cardiovascular Disease Risk: A Nationwide Cohort Study. Clin Gastroenterol Hepatol. 2021;19:2138–47.e10.
Yoneda M, Yamamoto T, Honda Y, Imajo K, Ogawa Y, Kessoku T, et al. Risk of cardiovascular disease in patients with fatty liver disease as defined from the metabolic dysfunction associated fatty liver disease or nonalcoholic fatty liver disease point of view: a retrospective nationwide claims database study in Japan. J Gastroenterol. 2021;56:1022–32.
Gutierrez-Cuevas J, Santos A, Armendariz-Borunda J. Pathophysiological Molecular Mechanisms of Obesity: A Link between MAFLD and NASH with Cardiovascular Diseases. Int J Mol Sci. 2021;22.
Higashiura Y, Tanaka M, Furuhashi M, Koyama M, Ohnishi H, Numata K, et al. Low urine pH predicts new onset of diabetes mellitus during a 10-year period in men: BOREAS-DM1 study. J Diabetes Investig. 2020;11:1490–7.
Higashiura Y, Tanaka M, Mori K, Mikami T, Hosaka I, Ohnishi H, et al. High fibrosis-4 index predicts the new onset of ischaemic heart disease during a 10-year period in a general population. Eur Heart Jl Open. 2022;2.
Osanami A, Tanaka M, Furuhashi M, Ohnishi H, Hanawa N, Yamashita T, et al. Increased LDL-cholesterol level is associated with deterioration of renal function in males. Clin Kidney J. 2022;https://doi.org/10.1093/ckj/sfac111).
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
American Diabetes A. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2017;40:S11–S24.
Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T, et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102:2708–15.
Lee SS, Park SH. Radiologic evaluation of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:7392–402.
Tokushige K, Ikejima K, Ono M, Eguchi Y, Kamada Y, Itoh Y, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. J Gastroenterol. 2021;56:951–63.
Tokushige K, Ikejima K, Ono M, Eguchi Y, Kamada Y, Itoh Y, et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. Hepatol Res. 2021;51:1013–25.
Leffondre K, Boucquemont J, Tripepi G, Stel VS, Heinze G, Dunkler D. Analysis of risk factors associated with renal function trajectory over time: a comparison of different statistical approaches. Nephrol Dial Transpl. 2015;30:1237–43.
Janmaat CJ, van Diepen M, Tsonaka R, Jager KJ, Zoccali C, Dekker FW. Pitfalls of linear regression for estimating slopes over time and how to avoid them by using linear mixed-effects models. Nephrol Dial Transpl. 2019;34:561–6.
Mori K, Furuhashi M, Tanaka M, Higashiura Y, Koyama M, Hanawa N, et al. Serum uric acid level is associated with an increase in systolic blood pressure over time in female subjects: Linear mixed-effects model analyses. Hypertens Res. 2022;45:344–53.
Shieh G. Clarifying the role of mean centring in multicollinearity of interaction effects. Br J Math Stat Psychol. 2011;64:462–77.
Haukeland JW, Damas JK, Konopski Z, Loberg EM, Haaland T, Goverud I, et al. Systemic inflammation in nonalcoholic fatty liver disease is characterized by elevated levels of CCL2. J Hepatol. 2006;44:1167–74.
Bai L, Li H. Innate immune regulatory networks in hepatic lipid metabolism. J Mol Med (Berl). 2019;97:593–604.
Carnagarin R, Matthews V, Zaldivia MTK, Peter K, Schlaich MP. The bidirectional interaction between the sympathetic nervous system and immune mechanisms in the pathogenesis of hypertension. Br J Pharm. 2019;176:1839–52.
Houghton D, Zalewski P, Hallsworth K, Cassidy S, Thoma C, Avery L, et al. The degree of hepatic steatosis associates with impaired cardiac and autonomic function. J Hepatol. 2019;70:1203–13.
Satou R, Penrose H, Navar LG. Inflammation as a Regulator of the Renin-Angiotensin System and Blood Pressure. Curr Hypertens Rep. 2018;20:100.
Watt MJ, Miotto PM, De Nardo W, Montgomery MK. The Liver as an Endocrine Organ-Linking NAFLD and Insulin Resistance. Endocr Rev. 2019;40:1367–93.
Anderson EA, Hoffman RP, Balon TW, Sinkey CA, Mark AL. Hyperinsulinemia produces both sympathetic neural activation and vasodilation in normal humans. J Clin Invest. 1991;87:2246–52.
Lembo G, Napoli R, Capaldo B, Rendina V, Iaccarino G, Volpe M, et al. Abnormal sympathetic overactivity evoked by insulin in the skeletal muscle of patients with essential hypertension. J Clin Invest. 1992;90:24–9.
Tanaka M, Takahashi S, Higashiura Y, Sakai A, Koyama M, Saitoh S, et al. Circulating level of fatty acid-binding protein 4 is an independent predictor of metabolic dysfunction-associated fatty liver disease in middle-aged and elderly individuals. J Diabetes Investig. 2022;13:878–88.
Furuhashi M, Ura N, Higashiura K, Murakami H, Tanaka M, Moniwa N, et al. Blockade of the renin-angiotensin system increases adiponectin concentrations in patients with essential hypertension. Hypertension 2003;42:76–81.
Murakami H, Ura N, Furuhashi M, Higashiura K, Miura T, Shimamoto K. Role of adiponectin in insulin-resistant hypertension and atherosclerosis. Hypertens Res. 2003;26:705–10.
Furuhashi M, Ura N, Higashiura K, Miyazaki Y, Murakami H, Hyakukoku M, et al. Low adiponectin level in young normotensive men with a family history of essential hypertension. Hypertens Res. 2005;28:141–6.
Ota H, Furuhashi M, Ishimura S, Koyama M, Okazaki Y, Mita T, et al. Elevation of fatty acid-binding protein 4 is predisposed by family history of hypertension and contributes to blood pressure elevation. Am J Hypertens. 2012;25:1124–30.
Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Disco. 2008;7:489–503.
Furuhashi M. Fatty Acid-Binding Protein 4 in Cardiovascular and Metabolic Diseases. J Atheroscler Thromb. 2019;26:216–32.
Furuhashi M. New insights into purine metabolism in metabolic diseases: role of xanthine oxidoreductase activity. Am J Physiol Endocrinol Metab. 2020;319:E827–E34.
Furuhashi M, Matsumoto M, Tanaka M, Moniwa N, Murase T, Nakamura T, et al. Plasma Xanthine Oxidoreductase Activity as a Novel Biomarker of Metabolic Disorders in a General Population. Circ J. 2018;82:1892–9.
Furuhashi M, Koyama M, Matsumoto M, Murase T, Nakamura T, Higashiura Y, et al. Annual change in plasma xanthine oxidoreductase activity is associated with changes in liver enzymes and body weight. Endocr J. 2019;66:777–86.
Furuhashi M, Matsumoto M, Murase T, Nakamura T, Higashiura Y, Koyama M, et al. Independent links between plasma xanthine oxidoreductase activity and levels of adipokines. J Diabetes Investig. 2019;10:1059–67.
Furuhashi M, Higashiura Y, Koyama M, Tanaka M, Murase T, Nakamura T, et al. Independent association of plasma xanthine oxidoreductase activity with hypertension in nondiabetic subjects not using medication. Hypertens Res. 2021;44:1213–20.
Tanaka J, Kumagai J, Katayama K, Komiya Y, Mizui M, Yamanaka R, et al. Sex- and age-specific carriers of hepatitis B and C viruses in Japan estimated by the prevalence in the 3,485,648 first-time blood donors during 1995-2000. Intervirology. 2004;47:32–40.
Tanaka J, Koyama T, Mizui M, Uchida S, Katayama K, Matsuo J, et al. Total numbers of undiagnosed carriers of hepatitis C and B viruses in Japan estimated by age- and area-specific prevalence on the national scale. Intervirology. 2011;54:185–95.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Acknowledgements
The authors are grateful to Keita Numata and Takashi Hisasue for data management.
Funding
MT and MF were supported by grants from the Japan Society for the Promotion of Science (19K08708, 20K08913, 22K08313).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mori, K., Tanaka, M., Hosaka, I. et al. Metabolic dysfunction-associated fatty liver disease is associated with an increase in systolic blood pressure over time: linear mixed-effects model analyses. Hypertens Res 46, 1110–1121 (2023). https://doi.org/10.1038/s41440-023-01179-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01179-0
Keywords
This article is cited by
-
Preface–Metabolic aspects of hypertension in Asia
Hypertension Research (2023)
-
Metabolic dysfunction-associated fatty liver disease reflects a significantly higher risk of hypertension than non-alcoholic fatty liver disease
Hypertension Research (2023)
-
An increase in calculated small dense low-density lipoprotein cholesterol predicts new onset of hypertension in a Japanese cohort
Hypertension Research (2023)
-
Current understanding and future perspectives on the impact of changing NAFLD to MAFLD on global epidemiology and clinical outcomes
Hepatology International (2023)