Abstract
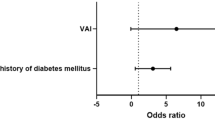
Aldosterone excess is present in obesity and is associated with involvement in the pathogenesis of obesity. We evaluate the impact of body obesity as measured by body composition monitor (BCM) on clinical outcomes in patients with unilateral primary aldosteronism (uPA) after adrenalectomy. The BCM device was used to assess body composition before and after adrenalectomy. We used fat mass (FM) and body mass index (BMI) to classify obesity and divided obesity into three groups: clinical overweight (BMI (kg/m2) ≥25); normal weight obesity (NWO, FM (%) ≥ 35 for women, >25 for men & BMI < 25); and no obesity (FM < 35 for women, <25 for men & BMI < 25). A total of 130 unilateral PA (uPA) patients received adrenalectomy, and 27 EH patients were identified; uPA patients with hypertension remission were found to have lower FM (p = 0.046), BMI (p < 0.001), and lower prevalence of overweight (p = 0.001). In the logistic regression model, patients with clinical overweight (OR = 2.9, p = 0.007), NWO (OR = 3.04, p = 0.041) and longer HTN duration (years, OR = 1.065, p = 0.013) were at the risk of persistent hypertension after adrenalectomy. Obesity status was strongly associated with persistent hypertension in uPA patients after adrenalectomy. However, patients in the NWO group also carried higher risk of persistent hypertension. Therefore, assessment of pre-obesity and overweight in uPA patients are extremely important, especially in those who have normal BMI.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Monticone S, Burrello J, Tizzani D, Bertello C, Viola A, Buffolo F, et al. Prevalence and Clinical Manifestations of Primary Aldosteronism Encountered in Primary Care Practice. J Am Coll Cardiol. 2017;69:1811–20.
Horton R. Aldosterone: review of its physiology and diagnostic aspects of primary aldosteronism. Metabolism 1973;22:1525–45.
Nicholls MG, Ramsay LE, Boddy K, Fraser R, Morton JJ, Robertson JI. Mineralocorticoid-induced blood pressure, electrolyte, and hormone changes, and reversal with spironolactone, in healthy men. Metabolism 1979;28:584–93.
Young WF Jr. Minireview: primary aldosteronism–changing concepts in diagnosis and treatment. Endocrinology 2003;144:2208–13.
Huang WC, Chen YY, Lin YH, Chen L, Lin PC, Lin YF, et al. Incidental Congestive Heart Failure in Patients With Aldosterone-Producing Adenomas. J Am Heart Assoc. 2019;8:e012410.
Wu CH, Yang YW, Hung SC, Tsai YC, Hu YH, Lin YH, et al. Effect of Treatment on Body Fluid in Patients with Unilateral Aldosterone Producing Adenoma: Adrenalectomy versus Spironolactone. Sci Rep. 2015;5:15297.
Heymsfield SB, Glenn JF, Retraction, Darsee JR, Heymsfield SB. Decreased myocardial taurine levels and hypertaurinuria in a kindred with mitral-valve prolapse and congestive cardiomyopathy. N Engl J Med. 1981;304:129–35.
Rocchini AP, Katch VL, Grekin R, Moorehead C, Anderson J. Role for aldosterone in blood pressure regulation of obese adolescents. Am J Cardiol. 1986;57:613–8.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32:959–66.
Prospective Studies C, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083–96.
Global BMIMC, Di Angelantonio E, Bhupathiraju Sh N, Wormser D, Gao P, Kaptoge S, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–86.
Lin HJ, Wang TD, Yu-Chih Chen M, Hsu CY, Wang KL, Huang CC, et al. 2020 Consensus Statement of the Taiwan Hypertension Society and the Taiwan Society of Cardiology on Home Blood Pressure Monitoring for the Management of Arterial Hypertension. Acta Cardiol Sin. 2020;36:537–61.
Wu VC, Chang HW, Liu KL, Lin YH, Chueh SC, Lin WC, et al. Primary aldosteronism: diagnostic accuracy of the losartan and captopril tests. Am J Hypertens. 2009;22:821–7.
Wu VC, Hu YH, Er LK, Yen RF, Chang CH, Chang YL, et al. Case detection and diagnosis of primary aldosteronism - The consensus of Taiwan Society of Aldosteronism. J Formos Med Assoc. 2017;116:993–1005.
Peng KY, Liao HW, Chan CK, Lin WC, Yang SY, Tsai YC, et al. Presence of Subclinical Hypercortisolism in Clinical Aldosterone-Producing Adenomas Predicts Lower Clinical Success. Hypertension 2020;76:1537–44.
Wu VC, Kuo CC, Wang SM, Liu KL, Huang KH, Lin YH, et al. Primary aldosteronism: changes in cystatin C-based kidney filtration, proteinuria, and renal duplex indices with treatment. J Hypertens. 2011;29:1778–86.
Wu VC, Lo SC, Chen YL, Huang PH, Tsai CT, Liang CJ, et al. Endothelial progenitor cells in primary aldosteronism: a biomarker of severity for aldosterone vasculopathy and prognosis. J Clin Endocrinol Metab. 2011;96:3175–83.
Wu VC, Huang KH, Peng KY, Tsai YC, Wu CH, Wang SM, et al. Prevalence and clinical correlates of somatic mutation in aldosterone producing adenoma-Taiwanese population. Sci Rep. 2015;5:11396.
Wu VC, Chueh SC, Chang HW, Lin LY, Liu KL, Lin YH, et al. Association of kidney function with residual hypertension after treatment of aldosterone-producing adenoma. Am J Kidney Dis. 2009;54:665–73.
Wu VC, Yang SY, Lin JW, Cheng BW, Kuo CC, Tsai CT, et al. Kidney impairment in primary aldosteronism. Clin Chim Acta. 2011;412:1319–25.
Wu VC, Wang SM, Chang CH, Hu YH, Lin LY, Lin YH, et al. Long term outcome of Aldosteronism after target treatments. Sci Rep. 2016;6:32103.
Cheng CY, Liao HW, Peng KY, Chen TH, Lin YH, Chueh JS, et al. Characteristics and Outcomes in Primary Aldosteronism Patients Harboring Glucocorticoid-Remediable Aldosteronism. Biomedicines 2021;9:1816.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70.
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, et al. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27:921–33.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1–253.
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701.
Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017;5:689–99.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Segura J, Ruilope LM. Obesity, essential hypertension and renin-angiotensin system. Public Health Nutr. 2007;10:1151–5.
Kalupahana NS, Moustaid-Moussa N. The renin-angiotensin system: a link between obesity, inflammation and insulin resistance. Obes Rev. 2012;13:136–49.
Canale MP, Manca di Villahermosa S, Martino G, Rovella V, Noce A, De Lorenzo A, et al. Obesity-related metabolic syndrome: mechanisms of sympathetic overactivity. Int J Endocrinol. 2013;2013:865965.
De Lorenzo A, Martinoli R, Vaia F, Di Renzo L. Normal weight obese (now) women: an evaluation of a candidate new syndrome. Nutr Metab Cardiovasc Dis. 2006;16:513–23.
Williams JS. Evolving research in nongenomic actions of aldosterone. Curr Opin Endocrinol Diabetes Obes. 2013;20:198–203.
Caprio M, Feve B, Claes A, Viengchareun S, Lombes M, Zennaro MC. Pivotal role of the mineralocorticoid receptor in corticosteroid-induced adipogenesis. FASEB J. 2007;21:2185–94.
Hung CS, Sung SH, Liao CW, Pan CT, Chang CC, Chen ZW, et al. Aldosterone Induces Vascular Damage. Hypertension 2019;74:623–9.
Burrello J, Burrello A, Stowasser M, Nishikawa T, Quinkler M, Prejbisz A, et al. The Primary Aldosteronism Surgical Outcome Score for the Prediction of Clinical Outcomes After Adrenalectomy for Unilateral Primary Aldosteronism. Ann Surg. 2020;272:1125–32.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006.
Er LK, Lin MC, Tsai YC, Hsiao JK, Yang CY, Chang CC, et al. Association of visceral adiposity and clinical outcome among patients with aldosterone producing adenoma. BMJ Open Diabetes Res Care. 2020;8:e001153.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–17.
Chan CK, Yang WS, Lin YH, Huang KH, Lu CC, Hu YH, et al. Arterial Stiffness Is Associated with Clinical Outcome and Cardiorenal Injury in Lateralized Primary Aldosteronism. J Clin Endocrinol Metab. 2020;105:dgaa566.
Chan CK, Kim JH, Chueh E, Chang CC, Lin YF, Lai TS, et al. Aldosterone level after saline infusion test could predict clinical outcome in primary aldosteronism after adrenalectomy. Surgery 2019;166:362–8.
Brilla CG, Weber KT. Mineralocorticoid excess, dietary sodium, and myocardial fibrosis. J Lab Clin Med. 1992;120:893–901.
Funder JW. Mineralocorticoid receptor activation and oxidative stress. Hypertension 2007;50:840–1.
Lim PS, Chen CH, Zhu F, Kotanko P, Jeng Y, Hu CY, et al. Validating Body Fat Assessment by Bioelectric Impedance Spectroscopy in Taiwanese Hemodialysis Patients. J Ren Nutr. 2017;27:37–44.
Hurwitz S, Cohen RJ, Williams GH. Diurnal variation of aldosterone and plasma renin activity: timing relation to melatonin and cortisol and consistency after prolonged bed rest. J Appl Physiol (1985). 2004;96:1406–14.
Acknowledgements
The authors greatly appreciate the Second Core Lab in National Taiwan University Hospital for technical assistance and Member of TAIPAI group (https://doi.org/10.6084/m9.figshare.21669929).
Funding
This study was supported by Ministry of Science and Technology (MOST) of the Republic of China (Taiwan) [grant number, MOST 107-2314-B-002-026-MY3, 108-2314-B-002-058, 110-2314-B-002-241, 110-2314-B-002-239, 111-2314-B-075-011-MY3], National Science and Technology Council (NSTC) [grant number, NSTC 109-2314-B-002-174-MY3, 110-2314-B-002-124-MY3, 111-2314-B-002-046, 111-2314-B-002-058], National Health Research Institutes [PH-102-SP-09], National Taiwan University Hospital [109-S4634, PC-1246, PC-1309, VN109-09, UN109-041, UN110-030, 111-FTN0011] Grant MOHW 110-TDU-B-212-124005 and Mrs Hsiu-Chin Lee Kidney Research Fund. (https://doi.org/10.6084/m9.figshare.21670460) The funds played no role in the design or conduct of the study, in the collection, management, analysis, or interpretation of the data, nor in the preparation, review, or approval of the paper.
Author information
Authors and Affiliations
Contributions
WCH drafted the paper and collected data. V-CW provided the original concept and design of the study, critically modified the statistical models, and provided technical and statistical support during the analyses. All the authors interpreted and had full access to the data, critically revised the paper, and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, WC., Chen, YY., Yang, SY. et al. Fat mass as an important predictor of persistent hypertension in patients with primary aldosteronism after adrenalectomy. Hypertens Res 46, 1375–1384 (2023). https://doi.org/10.1038/s41440-023-01203-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01203-3
Keywords
This article is cited by
-
Prediction of endogenous mineralocorticoid receptor activity by depressor effects of mineralocorticoid receptor antagonists in patients with primary aldosteronism
Hypertension Research (2024)
-
Recent progress in unraveling cardiovascular complications associated with primary aldosteronism: a succinct review
Hypertension Research (2024)
-
Fat mass: the most sensitive predictor of persistent hypertension in unilateral primary aldosteronism
Hypertension Research (2023)