Abstract
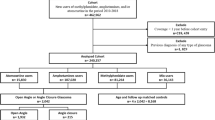
Obstructive sleep apnea (OSA) and primary aldosteronism (PA) often coexist in hypertension, whereas whether hypertensive patients with OSA should be screened for PA is controversial and whether gender, age, obesity and OSA severity should be considered is unexplored. We explored cross-sectionally prevalence and associated factors of PA in co-existent hypertension and OSA by considering gender, age, obesity and OSA severity. OSA was defined as AHI ≥5 events/h. PA diagnosis was defined, based on the 2016 Endocrine Society Guideline. We included 3306 patients with hypertension (2564 with OSA). PA prevalence was significantly higher in hypertensives with OSA than in those without OSA (13.2 vs 10.0%, P = 0.018). In gender-specific analysis, PA prevalence was significantly higher in hypertensive men with OSA, compared to non-OSA ones (13.8 vs 7.7%, P = 0.001). In further analysis, PA prevalence was significantly higher in hypertensive men with OSA aged <45 years (12.7 vs 7.0%), 45–59 years (16.6 vs 8.5%), and with overweight and obesity (14.1 vs 7.1%) than did their counterparts (P < 0.05). For OSA severity, men participants showed increased PA prevalence from non to moderate OSA and a decrease in the severe OSA group (7.7 vs 12.9 vs 15.1 vs 13.7%, P = 0.008). Young and middle age, moderate-severe OSA, weight, and blood pressure showed a positive independent association with PA presence in logistic regression. In conclusion, PA is prevalent in co-existent hypertension and OSA, indicating the need for PA screening. Studies are needed for women, older and lean population due to the smaller samples in this study.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a life course strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388:2665–712.
Funder JW, Carey RM, Mantero F, Murad MH, Reincke M, Shibata H, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916.
Brown JM, Siddiqui M, Calhoun DA, Carey RM, Hopkins PN, Williams GH, et al. The unrecognized prevalence of primary aldosteronism: a cross-sectional study. Ann Intern Med. 2020;173:10–20.
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and metaanalysis. Lancet Diabetes Endocrinol. 2018;6:41–50.
Rossi GP, Bisogni V, Rossitto G, Maiolino G, Cesari M, Zhu R, et al. Practice recommendations for diagnosis and treatment of the most common forms of secondary hypertension. High Blood Press Cardiovasc Prev. 2020;27:547–60.
Byrd JB, Turcu AF, Auchus RJ. Primary aldosteronism: practical approach to diagnosis and management. Circulation. 2018;138:823–35.
Pecori A, Buffolo F, Pieroni J, Forestiero V, Sconfienza E, Veglio F, et al. Primary aldosteronism and obstructive sleep apnea: casual association or pathophysiological link? Horm Metab Res. 2020;52:366–72.
Friedman O, Bradley TD, Chan CT, Parkes R, Logan AG. Relationship between overnight rostral fluid shift and obstructive sleep apnea in drug resistant hypertension. Hypertension. 2010;56:1077–82.
Di Murro A, Petramala L, Cotesta D, Zinnamosca L, Crescenzi E, Marinelli C, et al. Reninangiotensin-aldosterone system in patients with sleep apnoea: prevalence of primary aldosteronism. J Renin Angiotensin Aldosterone Syst. 2010;11:165–72.
Ehrhart-Bornstein M, Lamounier-Zepter V, Schraven A, Langenbach J, Willenberg HS, Barthel A, et al. Human adipocytes secrete mineralocorticoid-releasing factors. Proc Natl Acad Sci USA. 2003;100:14211–16.
Arlt W, Lang K, Sitch AJ, Dietz AS, Rhayem Y, Bancos I, et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight. 2017;2:e93136.
Wang LU, Wang TY, Bai YM, Hsu JW, Huang KL, Su TP, et al. Risk of obstructive sleep apnea among patients with Cushing’s syndrome: a nationwide longitudinal study. Sleep Med. 2017;36:44–7.
Calhoun DA, Nishizaka MK, Zaman MA, Harding SM. Aldosterone excretion among subjects with resistant hypertension and symptoms of sleep apnea. Chest. 2004;125:112–17.
Prejbisz A, Kołodziejczyk-Kruk S, Lenders JWM, Januszewicz A. Primary aldosteronism and obstructive sleep apnea: is this a bidirectional relationship? Horm Metab Res. 2017;49:969–76.
Dobrowolski P, Kołodziejczyk-Kruk S, Warchoł-Celińska E, Kabat M, Ambroziak U, Wróbel A, et al. Primary aldosteronism is highly prevalent in patients with hypertension and moderate to severe obstructive sleep apnea. J Clin Sleep Med. 2021;17:629–37.
Buffolo F, Li Q, Monticone S, Heinrich DA, Mattei A, Pieroni J, et al. Primary aldosteronism and obstructive sleep apnea: a cross-sectional multi-ethnic study. Hypertension. 2019;74:1532–40.
Mulatero P, Monticone S, Deinum J, Amar L, Prejbisz A, Zennaro MC, et al. Genetics, prevalence, screening and confirmation of primary aldosteronism: a position statement and consensus of the Working Group on Endocrine Hypertension of The European Society of Hypertension. J Hypertens. 2020;38:1919–28.
Chee MR, Hoo J, Libianto R, Gwini SM, Hamilton G, Narayan O, et al. Prospective screening for primary aldosteronism in patients with suspected obstructive sleep apnea. Hypertension. 2021;77:2094–103.
Gan L, Li N, Heizati M, Lin M, Zhu Q, Hong J, et al. Diurnal cortisol features with cardiovascular disease in hypertensive patients: a cohort study. Eur J Endocrinol. 2022;187:629–36.
Gan L, Li N, Heizhati M, Lin M, Zhu Q, Yao X, et al. Higher plasma aldosterone is associated with increased risk of cardiovascular events in hypertensive patients with suspected OSA: UROSAH data. Front Endocrinol (Lausanne). 2022;13:1017177.
Wang L, Li N, Yao X, Chang G, Zhang D, Heizhati M, et al. Detection of secondary causes and coexisting diseases in hypertensive patients: OSA and PA are the common causes associated with hypertension. BioMed Res Int. 2017;2017:8295010.
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–70.
Yang W, Shao L, Heizhati M, Wu T, Yao X, Wang Y, et al. Oropharyngeal microbiome in obstructive sleep apnea: decreased diversity and abundance. J Clin Sleep Med. 2019;15:1777–88.
Yan B, Zhao B, Jin X, Xi W, Yang J, Yang L, et al. Sleep efficiency may predict depression in a large population-based study. Front Psychiatry. 2022;13:838907.
Zhu Q, Heizhati M, Lin M, Wang M, Yao X, Gan L, et al. Higher plasma aldosterone concentrations are associated with elevated risk of aortic dissection and aneurysm: a case-control study. Hypertension. 2022;79:736–46.
Chen C, Lu FC. Department of Disease Control Ministry of Health, PR China The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci. 2004;17:1–36.
Anand V, Paolo M, Rene B, Adler GK. The expanding spectrum of primary aldosteronism: implications for diagnosis, pathogenesis, and treatment. Endocr Rev. 2018;39:1057–88.
Jin ZN, Wei YX. Meta-analysis of effects of obstructive sleep apnea on the renin-angiotensin-aldosterone system. J Geriatr Cardiol. 2016;13:333–43.
Li M, Ge Q, Sheng CS, Zhang J, Li H, Niu W, et al. Clinical characteristics of snoring patients with primary aldosteronism and obstructive sleep apnea–hypopnea syndrome. J Hum Hypertens. 2019;33:693–700.
Soltysiak M, Miazgowski T, Jaroszynska E. Impaired aldosterone response to the saline infusion test in patients with resistant hypertension and obstructive sleep apnea. Nadcisnienie Tetnicze. 2015;1:13–8.
Nanba K, Omata K, Else T, Beck PCC, Nanba AT, Turcu AF, et al. Targeted molecular characterization of aldosterone-producing adenomas in white Americans. J Clin Endocrinol Metab. 2018;103:3869–76.
Caroccia B, Seccia TM, Campos AG, Gioco F, Kuppusamy M, Ceolotto G, et al. GPER-1 and estrogen receptor-β ligands modulate aldosterone synthesis. Endocrinology. 2014;155:4296–304.
Nanba K, Rainey WE. Genetics in endocrionology: impact of race and sex on genetic causes of aldosterone-producing adenomas. Eur J Endocrinol. 2021;185:R1–11.
Zhang L, Ou X, Zhu T, Lv X. Beneficial effects of estrogens in obstructive sleep apnea hypopnea syndrome. Sleep Breath. 2020;24:7–13.
Gargaglioni LH, Marques DA, Patrone LGA. Sex differences in breathing. Comp Biochem Physiol A Mol Integr Physiol. 2019;238:110543.
Acknowledgements
NL provided the idea, obtained the fund support, participated in the design, gave critical advice in data analysis, interpretation, and in writing. MH designed the study, collected and analyzed the data, and wrote the paper. XA, LG, ML, QL, MW, JH, NM, GD, WY, LY and QZ participated in the design, collected the data, gave data advice in data analysis and interpretation, and in writing.
Funding
This study was supported by the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2020-RW330-002).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heizhati, M., Aierken, X., Gan, L. et al. Prevalence of primary aldosteronism in patients with concomitant hypertension and obstructive sleep apnea, baseline data of a cohort. Hypertens Res 46, 1385–1394 (2023). https://doi.org/10.1038/s41440-023-01226-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01226-w
Keywords
This article is cited by
-
Topics 2023 in Hypertension Research leading to guidelines in Asia
Hypertension Research (2023)
-
Primary aldosteronism and obstructive sleep apnea: the strong ties between them
Hypertension Research (2023)