Abstract
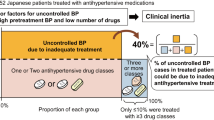
Hypertension remains a major global healthcare issue. Considering that most Japanese patients with hypertension are managed by general practitioners, hypertension specialists should be involved in actual clinical practice. We investigated the blood pressure (BP), guidelines recommended for achievement rate of the target BP, and clinical variables of patients with hypertension treated by hypertension specialists and those treated by non-specialists in a real-world setting. Factors associated with the target BP achievement in this population were also investigated. Outpatients with hypertension from 12 medical facilities in Okinawa Prefecture were enrolled (n = 1469 [specialist group, 794; non-specialist group, 675]; mean age, 64.2 years; females, 45.8%). For all patients, BP and rate of the target BP achievement were 129.0 ± 15.5/74.6 ± 10.6 mmHg, and 51.8%, respectively. BP and the rate of target of BP achievement were 128.0 ± 15.1/73.4 ± 10.4 mmHg and 56.7% in the specialist group, and they were 130.1 ± 15.9/76.0 ± 10.8 mmHg and 46.1% in the non-specialist group. The urinary salt excretion and obesity rates were comparable between the specialist and non-specialist groups. Multivariable logistic analyses indicated that hypertension specialists and good medication adherence were positive factors, whereas obesity, chronic kidney disease, diabetes mellitus, and urinary salt excretion were inverse factors associated with target BP achievement in this population. Initiatives for salt reduction, medication adherence, and proper obesity management are crucial to improving BP management in patients with hypertension. Hypertension specialists are expected to play an essential role in them.

For all patients, the target blood pressure (BP) achievement rate were 51.8%. Hypertension specialists and good medication adherence were positive factors in achieving target BP; conversely, obesity, diabetes mellitus, chronic kidney disease, and high urinary salt excretion were inverse factors in achieving target BP among patients with hypertension.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71:e13–e115.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104.
Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia. Ann Intern Med. 2001;135:825–34.
Obara T, Ubeda SR, Ohkubo T, Matsuura H, Ishimitsu T, Takata M, et al. Awareness of the Japanese Society of Hypertension guidelines for the management of hypertension and their use in clinical practices: 2009 survey results. Hypertens Res. 2015;38:400–4.
Mogi M, Hasebe N, Horiuchi M, Shimamoto K, Umemura S. The results of a survey of physicians about the Japanese Society of Hypertension guidelines for the management of hypertension 2014 and its clinical use. Hypertens Res. 2016;39:660–3.
Yoshida T, Nishigaki N, Saita S, Shimasaki Y, Hasebe N. Perspectives of patients and physicians regarding hypertensive management from an online survey for excellence: a subanalysis of the PARADOX study by physician categories. Hypertens Res. 2020;43:431–41.
Yamazato M, Sakima A, Ishida A, Kohagura K, Matayoshi T, Tana T, et al. Salt and potassium intake evaluated with spot urine and brief questionnaires in combination with blood pressure control status in hypertensive outpatients in a real-world setting. Hypertens Res. 2021;44:1316–25.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Japanese Society of Nephrology. Essential points from Evidence-based Clinical Practice Guidelines for Chronic Kidney Disease 2018. Clin Exp Nephrol. 2019;23:1–15.
Japanese Society of Nephrology. Evidence-Based Clinical Practice Guideline for CKD 2018. Tokyo: Tokyo Igakusha; 2018.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16:97–103.
Yasutake K, Miyoshi E, Kajiyama T, Umeki Y, Misumi Y, Horita N, et al. Comparison of a salt check sheet with 24-h urinary salt excretion measurement in local residents. Hypertens Res. 2016;39:879–85.
Sakata S, Tsuchihashi T, Oniki H, Tominaga M, Arakawa K, Sakaki M, et al. Relationship between salt intake as estimated by a brief self-administered diet-history questionnaire (BDHQ) and 24-h urinary salt excretion in hypertensive patients. Hypertens Res. 2015;38:560–3.
Sasaki S, Yanagibori R, Amano K. Self-administered diet history questionnaire developed for health education: a relative validation of the test-version by comparison with 3-day diet record in women. J Epidemiol. 1998;8:203–15.
Ohe K, Yasutake K, Murata Y, Tsuchihashi T, Enjoji M. Assessment of dietary salt and sodium intake: from device to questionnaire. Qual Prim Care. 2017;25:101–8.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2009;32:3–107.
Nishigaki N, Shimasaki Y, Yoshida T, Hasebe N. Physician and patient perspectives on hypertension management and factors associated with lifestyle modifications in Japan: results from an online survey. Hypertens Res. 2020;43:450–62.
Tsuchihashi T, Ishimitsu T, Ando K, Kusaka M, Ichihara A, Miura K, et al. JSH Statement: Tokyo declaration promoting salt reduction by the Japanese Society of Hypertension-the JSH Tokyo declaration. Hypertens Res. 2020;43:1133–4.
Tsuchihashi T. Dietary salt intake in Japan-past, present, and future. Hypertens Res. 2022;45:748–57.
Kario K, Nomura A, Harada N, Okura A, Nakagawa K, Tanigawa T, et al. Efficacy of a digital therapeutics system in the management of essential hypertension: the HERB-DH1 pivotal trial. Eur Heart J. 2021;42:4111–22.
Poulter NR, Borghi C, Parati G, Pathak A, Toli D, Williams B, et al. Medication adherence in hypertension. J Hypertens. 2020;38:579–87.
Choudhry NK, Kronish IM, Vongpatanasin W, Ferdinand KC, Pavlik VN, Egan BM, et al. Medication adherence and blood pressure control: a scientific statement from the American Heart Association. Hypertension. 2022;79:e1–e14.
Fukai K, Nagata T, Mori K, Ohtani M, Fujimoto K, Nagata M, et al. Validation of self-reported medication use for hypertension, diabetes, and dyslipidemia among employees of large-sized companies in Japan. J Occup Health. 2020;62:e12138.
Matsumoto M, Harada S, Iida M, Kato S, Sata M, Hirata A, et al. Validity assessment of self-reported medication use for hypertension, diabetes, and dyslipidemia in a pharmacoepidemiologic study by comparison with health insurance claims. J Epidemiol. 2021;31:495–502.
Fujita M, Sato Y, Nagashima K, Takahashi S, Hata A. Validity assessment of self-reported medication use by comparing to pharmacy insurance claims. BMJ Open. 2015;5:e009490.
Hirawa N, Umemura S, Ito S. Viewpoint on guidelines for treatment of hypertension in Japan. Circ Res. 2019;124:981–3.
Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169:1748–55.
Santschi V, Chiolero A, Colosimo AL, Platt RW, Taffé P, Burnier M, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3:e000718.
Siebenhofer A, Winterholer S, Jeitler K, Horvath K, Berghold A, Krenn C, et al. Long-term effects of weight-reducing drugs in people with hypertension. Cochrane Database Syst Rev. 2021;1:CD007654.
Lavie CJ, De Schutter A, Parto P, Jahangir E, Kokkinos P, Ortega FB, et al. Obesity and prevalence of cardiovascular diseases and prognosis-the obesity paradox updated. Prog Cardiovasc Dis. 2016;58:537–47.
Jahangir E, De Schutter A, Lavie CJ. Low weight and overweightness in older adults: risk and clinical management. Prog Cardiovasc Dis. 2014;57:127–33.
Childers DK, Allison DB. The ‘obesity paradox’: a parsimonious explanation for relations among obesity, mortality rate and aging? Int J Obes. 2010;34:1231–8.
Kudo N, Yokokawa H, Fukuda H, Sanada H, Miwa Y, Hisaoka T, et al. Achievement of target blood pressure levels among Japanese workers with hypertension and healthy lifestyle characteristics associated with therapeutic failure. PLoS One. 2015;10:e0133641.
Miyagawa N, Okuda N, Nakagawa H, Takezaki T, Nishi N, Takashima N, et al. Socioeconomic status associated with urinary sodium and potassium excretion in Japan: NIPPON DATA2010. J Epidemiol. 2018;28:S29–34.
Iseki K, Iseki C, Itoh K, Uezono K, Sanefuji M, Ikemiya Y, et al. Urinary excretion of sodium and potassium in a screened cohort in Okinawa, Japan. Hypertens Res. 2002;25:731–6.
Ministry of Health, Labour and Welfare of Japan. Overview of dietary reference intakes for Japanese. 2020. https://www.mhlw.go.jp/content/10900000/000862500.pdf. Accessed 1 February 2023.
WHO. Guideline: potassium intake for adults and children. Geneva: World Health Organization; 2009.
NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639–51.
Chow CK, Gupta R. Blood pressure control: a challenge to global health systems. Lancet. 2019;394:613–5.
Kohro T, Furui Y, Mitsutake N, Fujii R, Morita H, Oku S, et al. The Japanese national health screening and intervention program aimed at preventing worsening of the metabolic syndrome. Int Heart J. 2008;49:193–203.
Kario K, Wang JG. Could 130/80 mm Hg Be adopted as the diagnostic threshold and management goal of hypertension in consideration of the characteristics of Asian Populations? Hypertension. 2018;71:979–84.
Ohya Y, Kario K, Itoh H, Nishiyama A, Ishimitsu T, Ichihara A, et al. Statement of the Asian Hypertension Society Network: the Okinawa Declaration on the unity of hypertension societies in Asian countries and regions to overcome hypertension and hypertension-related diseases. Hypertens Res. 2022;45:1–2.
Acknowledgements
The authors are grateful for the cooperation of the staff of the collaborating medical facilities, particularly doctors Tamashiro M, Hata Y, Naka T, T. Kikumura, N. Nagayoshi, M. Tomori, C. Imai, M. Matsuoka, and Y. Shinzato. The authors are also grateful to our clinical research coordinators, particularly M. Kobayashi and M. Nakahodo for retrieving data from the facilities and F. Aniya and K. Kohama for their excellent assistance as nutritionists. In addition, the authors would like to thank Enago (www.enago.com) for the English language review.
Funding
This work was partly supported by the Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (Grant no. 2530891).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakima, A., Yamazato, M., Kohagura, K. et al. Achievement rate of target blood pressure in patients with hypertension treated by hypertension specialists and non-specialists in a real-world setting. Hypertens Res 46, 2460–2469 (2023). https://doi.org/10.1038/s41440-023-01362-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01362-3
Keywords
This article is cited by
-
Optimal blood pressure and improvement of achievement rate
Hypertension Research (2023)