Abstract
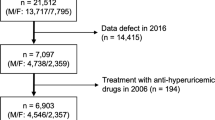
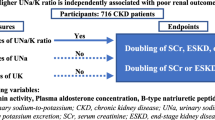
Chronic kidney disease (CKD) is a major risk factor for cardiovascular diseases as well as end-stage kidney disease. Increased dietary sodium (Na) or decreased dietary potassium (K) deteriorates kidney function; however, findings regarding the association of dietary Na/K ratio with kidney function are limited and conflicting. Therefore, the present study investigated the impact of urinary Na/K ratio on the development of CKD, defined as estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2, in the Japanese general population. In total, 14,549 subjects without CKD who participated in our medical checkup were enrolled. The urinary Na/K ratio was measured using a sample of overnight urine. The subjects were followed up until the endpoint (onset of CKD). During the median follow-up period of 61.4 months, CKD developed in 2096 participants (25.9 per 1000 person-years). The risk of developing CKD increased across the quartiles of baseline urinary Na/K ratio in the Kaplan–Meier analysis (log-rank, P < 0.001). In multivariate Cox proportional hazard regression analysis, urinary Na/K ratio was a significant predictor of new-onset CKD after adjustment for important factors including eGFR at baseline (hazard ratio, 2.013; 95% confidence interval, 1.658–2.445; p < 0.001). Moreover, baseline urinary Na/K ratio was found to be independently correlated with yearly decline in eGFR. Similar results were obtained in subgroups of participants with and without hypertension. Thus, urinary Na/K ratio is significantly associated with the development of CKD in the general population.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hirata A, Okamura T, Sugiyama D, Kuwabara K, Kadota A, Fujiyoshi A.NIPPON DATA90 and 2010 Research Group et al. Impacts of chronic kidney disease and diabetes on cardiovascular mortality in a general Japanese population: a 20-year follow-up of the NIPPON DATA90 study. Eur J Prev Cardiol. 2017;24:505–13.
Park SK, Kim MH, Ha E, Jung JY, Oh CM, Choi JM, et al. The risk for incident ischemic heart disease according to estimated glomerular filtration rate in a Korean population. J Atheroscler Thromb. 2020;27:461–70.
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
Gopinath B, Harris DC, Flood VM, Burlutsky G, Mitchell P. A better diet quality is associated with a reduced likelihood of CKD in older adults. Nutr Metab Cardiovasc Dis. 2013;23:937–43.
Jain N, Reilly RF. Effects of dietary interventions on incidence and progression of CKD. Nat Rev Nephrol. 2014;10:712–24.
Yuzbashian E, Asghari G, Mirmiran P, Hosseini FS, Azizi F. Associations of dietary macronutrients with glomerular filtration rate and kidney dysfunction: Tehran lipid and glucose study. J Nephrol. 2015;28:173–80.
Sugiura T, Takase H, Ohte N, Dohi Y. Dietary Salt Intake is a significant determinant of impaired kidney function in the general population. Kidney Blood Press Res. 2018;43:1245–54.
Lin J, Hu FB, Curhan GC. Associations of diet with albuminuria and kidney function decline. Clin J Am Soc Nephrol. 2010;5:836–43.
He J, Mills KT, Appel LJ, Yang W, Chen J, Lee BT. Chronic Renal Insufficiency Cohort Study Investigators et al. Urinary sodium and potassium excretion and CKD progression. J Am Soc Nephrol. 2016;27:1202–12.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH, Jr, Kostis JB. TONE Collaborative Research Group et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). JAMA . 1998;279:839–46.
Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A. PURE Investigators et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 2014;371:601–11.
Takase H, Sugiura T, Kimura G, Ohte N, Dohi Y. Dietary sodium consumption predicts future blood pressure and incident hypertension in the Japanese normotensive general population. J Am Heart Assoc. 2015;4:e001959.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Fan L, Tighiouart H, Levey AS, Beck GJ, Sarnak MJ. Urinary sodium excretion and kidney failure in nondiabetic chronic kidney disease. Kidney Int. 2014;86:582–8.
Lin HB, Young DB, Smith MJ Jr. Stimulation of renin release by hyperkalemia in the nonfiltering kidney. Am J Physiol. 1991;260:F170–6.
Kim HW, Park JT, Yoo TH, Lee J, Chung W, Lee KB. KNOW-CKD study investigators et al. Urinary potassium excretion and progression of CKD. Clin J Am Soc Nephrol. 2019;14:330–40.
Kieneker LM, Bakker SJ, de BoerRA, Navis GJ, Gansevoort RT, Joosten MM. Low potassium excretion but not high sodium excretion is associated with increased risk of developing chronic kidney disease. Kidney Int. 2016;90:888–96.
Leonberg-Yoo AK, Tighiouart H, Levey AS, Beck GJ, Sarnak MJ. Urine potassium excretion, kidney failure, and mortality in CKD. Am J Kidney Dis. 2017;69:341–9.
Mirmiran P, Nazeri P, Bahadoran Z, Khalili-Moghadam S, Azizi F. Dietary sodium to potassium ratio and the incidence of chronic kidney disease in adults: a longitudinal follow-up study. Prev Nutr Food Sci. 2018;23:87–93.
Koo H, Hwang S, Kim TH, Kang SW, Oh KH, Ahn C, et al. The ratio of urinary sodium and potassium and chronic kidney disease progression: results from the Korean cohort study for outcomes in patients with chronic kidney disease (KNOW-CKD). Medicine. 2018;97:e12820.
Hattori H, Hirata A, Kubo S, Nishida Y, Nozawa M, Kawamura K, et al. Estimated 24 h urinary sodium-to-potassium ratio is related to renal function decline: a 6-year cohort study of Japanese urban residents. Int J Environ Res Public Health. 2020;17:5811.
Tabara Y, Takahashi Y, Setoh K, Kawaguchi T, Kosugi S, Nakayama T, et al. Prognostic significance of spot urine Na/K for longitudinal changes in blood pressure and renal function: the Nagahama Study. Am J Hypertens. 2017;30:899–906.
Palacios C, Wigertz K, Martin BR, Braun M, Pratt JH, Peacock M, et al. Racial differences in potassium homeostasis in response to differences in dietary sodium in girls. Am J Clin Nutr. 2010;91:597–603.
Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus, Seino Y, Nanjo K, Tajima N, Kadowaki T, Kashiwagi A, Araki E, et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Investig. 2010;1:212–28.
Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, et al. Japan Atherosclerosis Society (JAS) Committee for Epidemiology and Clinical Management of Atherosclerosis. Diagnostic criteria for dyslipidemia. Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerotic cardiovascular diseases for Japanese. J Atheroscler Thromb. 2007;14:155–8.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Travers K, Martin A, Khankhel Z, Boye KS, Lee LJ. Burden and management of chronic kidney disease in Japan: systematic review of the literature. Int J Nephrol Renovasc Dis. 2013;6:1–13.
Kokado Y, Ishii M, Ueta K, Yamamoto H, Kumamaru H, Isshiki M, et al. Characteristics of Japanese patients with non-dialysis-dependent chronic kidney disease initiating treatment for anemia: a retrospective real-world database study. Curr Med Res Opin. 2022;38:2175–82.
Fujita T, Ando K. Hemodynamic and endocrine changes associated with potassium supplementation in sodium-loaded hypertensives. Hypertension. 1984;6:184–92.
McCabe RD, Young DB. Potassium inhibits cultured vascular smooth muscle cell proliferation. Am J Hypertens. 1994;7:346–50.
Dohi Y. Plasma B-type natriuretic peptide level as a possible predictor of dietary salt intake. Hypertens Res. 2022;45:1134–35.
McCabe RD, Bakarich MA, Srivastava K, Young DB. Potassium inhibits free radical formation. Hypertension. 1994;24:77–82.
Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D. et al. Effects of oral potassium on blood pressure: meta-analysis of randomized controlled clinical trials. JAMA. 1997;277:1624–32.
Katori M, Majima M. The renal kallikrein-kinin system: its role as a safety valve for excess sodium intake, and its attenuation as a possible etiologic factor in salt-sensitive hypertension. Crit Rev Clin Lab Sci. 2003;40:4.
He FJ, MacGregor GA. Fortnightly review: beneficial effects of potassium. BMJ. 2001;323:497–501.
Ogihara T, Asano T, Ando K, Sakoda H, Anai M, Shojima N, et al. High-salt diet enhances insulin signaling and induces insulin resistance in Dahl salt-sensitive rats. Hypertension. 2002;40:83–9.
Sharma S, McFann K, Chonchol M, de Boer IH, Kendrick J. Association between dietary sodium and potassium intake with chronic kidney disease in US adults: a cross-sectional study. Am J Nephrol. 2013;37:526–33.
Kieneker LM, Bakker SJ, de Boer RA, Navis GJ, Gansevoort RT, Joosten MM. Low potassium excretion but not high sodium excretion is associated with increased risk of developing chronic kidney disease. Kidney Int. 2016;90:888–96.
Poorolajal J, Zeraati F, Soltanian AR, Sheikh V, Hooshmand E, Maleki A. Oral potassium supplementation for management of essential hypertension: a meta-analysis of randomized controlled trials. PLoS One. 2017;12:e0174967.
Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, et al. Sodium and potassium intake and balance in adults consuming self-selected diets. Am J Clin Nutr. 1984;40:786–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takase, H., Kawakatsu, N., Hayashi, K. et al. Urinary Na/K ratio is a predictor of developing chronic kidney disease in the general population. Hypertens Res 47, 225–232 (2024). https://doi.org/10.1038/s41440-023-01399-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01399-4